Cervical Fusion
Am I CandidateThe neck pain started gradually but continued despite conservative care and medications. Your doctor referred you for a surgical consultation leading to a discussion about cervical fusion.
What does this procedure entail? Are there different types of cervical fusions? What happens during surgery? What are the indications for neck fusion surgery? How is the recovery from neck fusion? What are the complications associated with cervical fusion? What are the alternatives to cervical fusion? What regenerative alternatives exist?
Cervical fusion is often recommended when chronic neck pain problems worsen over time, but what exactly is it?
Find out if cervical fusion is the right procedure for you. This post will cover its types and indications.
What is Cervical Spinal Fusion?
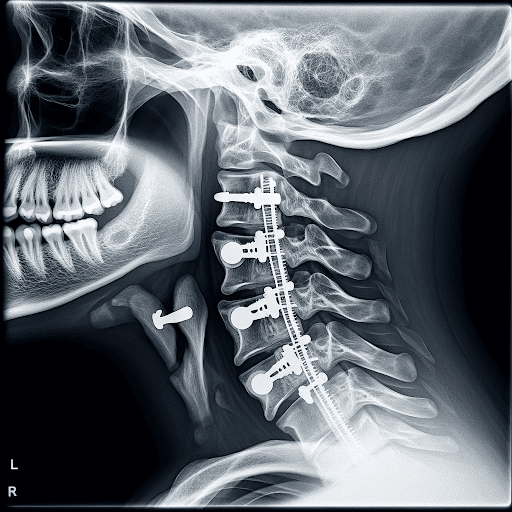
Cervical fusion, or cervical spinal fusion, is a major surgery that involves joining one or more of the spinal bones together using screws, bolts, and plates (1). The hardware may be placed in the front (anterior) or the back (posterior) of the cervical spine. The disc between the spinal bones is often removed and replaced with a bone graft or a spacer.
The neck is composed of seven bony building blocks that are numbered from 1-7. The letter C is associated with the numbers to designate the cervical spine. Hence the bones in the neck are C1 through C7.
Between the neck bones are important shock absorbers called discs. A cervical fusion surgery removes this important shock absorber and joins the adjacent bones together with the hardware.
Types of Cervical Spinal Fusion Surgeries
There are several different types of cervical fusion procedures. The differences in part are due to their approach to the cervical spine. The two most common cervical fusions are the anterior cervical discectomy (ACDF), and the posterior fusion. Both procedures have the goal of treating symptomatic neck conditions that have not responded to conservative therapy and are progressive.
The disc is removed in an effort to decrease the pain and relieve existing nerve root or spinal cord compression. The principal difference between these two surgeries is the approach to the spine. One is from the front (anterior) whereas the other is from the back (posterior).
Anterior Cervical Discectomy and Fusion (ACDF) Interbody Fusion
This is one of the most common types of neck surgery. One study cited an average of 137,000 ACDF surgeries performed annually in the United States (2). It involves removing the disc through the front of the neck, followed by the insertion of a plate with screws to stabilize the spine.
Posterior Fusion
Posterior fusion surgery involves removing the disc from the backside of the neck; the surgical approach is from the posterior. Access to the disc is more difficult through a posterior approach. Accordingly, there are significant postoperative complications with this approach that range from 8.6-49%.
How Does Cervical Fusion Work?
Cervical fusion aims to stabilize the cervical spine by promoting the fusion of adjacent vertebrae. This is achieved by using bone grafts or substitutes to encourage the growth of new bone tissue between the vertebrae. The fusion restricts movement between the vertebrae, alleviating pain caused by instability or pressure on spinal nerves.
Often, a small piece of bone is taken from the patient’s own hip or another part of the body to serve as the graft. Autografts are advantageous as they contain live cells that promote bone growth.
Alternatively, surgeons may use bone tissue from a donor (cadaver). Allografts eliminate the need for a second surgical site on the patient but may take longer to incorporate the graft. In some cases, synthetic materials or bone morphogenetic proteins (BMPs) may be utilized to stimulate bone growth. These substitutes can provide structural support and encourage the natural healing process.
The surgeon accesses the cervical spine through an incision in the front (anterior approach) or back (posterior approach), depending on the patient’s condition. If a herniated disc is present, the surgeon may remove the damaged disc material to relieve pressure on the spinal cord or nerves.
The selected graft or substitute is placed between the vertebrae to create a bridge. Metal plates, screws, or rods may be used to secure the graft and stabilize the spine. Over time, the body naturally fuses the vertebrae, integrating the graft with the existing bone. This process typically takes several months and may be monitored through imaging studies.
Common Conditions Cervical Fusion Treats
There are several cervical spine conditions that may require surgery. The most common include:
Cervical Disc Degeneration/Injury
The disc is an important shock absorber that is sandwiched between the spinal bones in the neck. It is susceptible to injury and degeneration as a result of trauma and repetitive wear and tear. One or more discs may become a source of severe neck pain. That is why when conservative treatments fail, some patients are referred for cervical fusion surgery.
Cervical Spinal Instability (CCI)
The neck, a delicate structure comprising seven vertebrae stacked upon one another, relies on a complex network of ligaments, muscles, tendons, and fascia to maintain stability. When any of these crucial components are weakened or injured, it can lead to a condition known as cervical spinal instability, with potential consequences for the spinal cord, nerve roots, facet joints, and cervical discs.
When one or more vertebrae slip forward in relation to the adjacent bones, it’s termed antero listhesis. This movement can result from weakened or injured ligaments, muscles, or other supporting structures.
Conversely, if a vertebra slips backward from the others, it is referred to as retrolisthesis. Both antero listhesis and retrolisthesis can lead to irritation and injury of critical spinal components.
The movement associated with cervical spinal instability can cause significant irritation or injury to the spinal cord and nerve roots, contributing to debilitating neck and upper extremity pain.
The facet joints and cervical discs may also be affected, further intensifying discomfort and restricting the neck’s range of motion.
When cervical instability involves the ligaments supporting the head and neck, it may lead to a condition known as craniocervical instability (CCI). Patients may experience a range of neurologic symptoms, including brain fog, fatigue, headaches, visual problems, and vertigo.
For a deeper understanding of CCI and its impact on patients, watch the informative video linked below. This video sheds light on the intricacies of CCI, helping individuals grasp the significance of maintaining spinal stability for overall well-being.
Nerve Compression
Nerves exit the cervical spine through a bony doorway called the neural foramen. The foramen can be narrowed by disc protrusion, disc herniation, facet joint overgrowth, ligament instability, disc slippage, or a cyst causing compression or injury to the nerve.
This can cause radiating arm and hand pain, numbness and tingling, and reduced muscle strength. When unresponsive to conservative care, some patients are referred for neck fusion evaluations.
Spinal Cord Compression
The spinal cord is the nerve network that controls most of your body’s function. It starts at the base of the brain and extends into the lower back. It is encased in a protective layer of the bone. It is surrounded and protected by an additional layer of fluid called the cerebral spinal fluid.
The spinal cord is fragile and susceptible to injury. Symptoms can be mild or severe, depending on the extent of the damage. A tragic example is actor Christopher Reeve who sustained a traumatic spinal cord injury after falling from a horse. He was paralyzed and required assistance with all bodily functions, including breathing.
Trauma To Cervical Spine
Trauma to the spine can cause instability and compression of nerves and discs. Cervical fusion is then often recommended in severe cases to stabilize the spine and avoid spinal cord injury and paralysis.
Infection
The cervical bones and disc can become infected, causing significant damage to the neck. Neck fusion is a treatment option when the infection is not controlled with antibiotic therapy.
Tumors
Cancer can occur anywhere in the body. When it appears in the neck, it can compromise the spinal cord, existing spinal nerves, and the discs. When the integrity of the spine is compromised and conservative treatments fail, cervical fusion is often recommended.
The Procedure Of Cervical Fusion
Listed below are the steps involved in the transformative journey of cervical fusion, a surgical marvel designed to bring stability to the delicate neck region, offering relief to those burdened by pain and spinal discomfort.
Before The Surgery
Before cervical fusion surgery, a thorough medical evaluation is conducted. This typically includes a detailed review of the patient’s medical history, physical examination, and diagnostic tests such as X-rays, MRI scans, or CT scans.
These assessments help the medical team understand the specific cervical spine issues and formulate a personalized surgical plan. Cervical fusion is performed at a hospital or outpatient surgical center. It involves general anesthesia in which you are put to sleep for the duration of the surgery.
During The Surgery
Anterior cervical discectomy and fusion have four principal steps.
- Step 1: Anterior surgical approach
Anterior refers to the front of the neck. A horizontal skin incision is made in the front of the neck followed by separation of the different layers of muscle, tendons, and fascia. - Step 2: Removal of disc, aka discectomy
After the correct cervical disc is identified using an X-ray, it is surgically cut out. This removes the problematic disc and allows the evaluation of deeper structures in the cervical spine. - Step 3: Decompression of the cervical canal
Once the disc is removed, the posterior longitudinal ligament (PLL) is identified. This stabilizing ligament is frequently trimmed or cut out to allow for visualization of the central spinal canal.
If an extruded disc, disc fragments, or bone spurs are present within the central canal, they are surgically removed. In addition, the bony doorway through which the spinal nerves exit is evaluated and roto-rooted out if bone spurs are compressing or irritating the spinal nerves. - Step 4: Cervical fusion
A surgical cage or implant along with a bone graft is then inserted into the space previously occupied by the cervical disc. The goal is to maintain the disc space height and promote the two cervical bones to mend together. A small plate is then attached in the front of the neck to the cervical bones. It provides stability and promotes the fusion of the two bones.
After The Surgery
In the subsequent hours, healthcare professionals assess vital signs, manage pain, and address any immediate concerns. As patients regain awareness, they may gradually begin mobility exercises and receive guidance on postoperative care, including wound care and pain management strategies.
The early days post-surgery focus on rest and gentle movements, gradually progressing to more active rehabilitation. Physical therapy becomes a cornerstone of the recovery process, aiding in the restoration of neck strength and flexibility. Regular follow-up appointments with the surgical team allow for ongoing assessment of progress and adjustments to the recovery plan.
What To Expect After The Cervical Fusion Procedure
As every individual is different, the post-operative course can largely vary. Here are some possible things to watch out for after surgery.
Possible Side Effects Of Cervical Fusion
There are inherent risks associated with any surgery. Some possible side effects from a cervical fusion include:
- Difficulty swallowing
Difficulty swallowing is called dysphagia and can occur after neck fusion. The incidence of dysphagia after cervical fusion surgery in one study was 12.7% (4). Difficulty swallowing can compromise calorie and fluid intake, and healing. - Failed fusion
This is BAD news. When the bones don’t fuse, it’s called non-union or pseudo-arthrosis. This means that even after surgery, having screws and plates inserted, doing a lot of rehab, and enduring pain, the bones didn’t come together as they should have.
The intended surgery has failed and now there is instability in the neck. The incidence of non-union is striking and in one study was found to be 52% (5). The treatment for non-union involves another surgery where the fusion is revised, and oftentimes extended up or down an additional level. - Continued neck pain
Despite neck fusion surgery, many patients continue to have ongoing neck pain that requires oral narcotics. According to a recent study, just 39% of patients managed to resume work one year after undergoing neck fusion. - Spinal fluid leak (CSF)
The dura is the outermost membrane that covers the brain and spinal cord. This important membrane can be punctured during surgery, causing a leak of spinal fluid. The incidence ranges from 1-17% (7). Severe headache is a common symptom of spinal fluid leak. If left untreated, a spinal fluid leak (CSF) can lead to infection, brain abscess, and bleeding. - Nerve injury
Nerves can be damaged during surgery and the incidence varies from 0.18% to 2.6% (8). Nerve injury can include existing nerves as well as the spinal cord itself. After cervical fusion surgery, patients may awaken after surgery with new onset pain in the left arm, face, or lower extremity. - Changes in the spinal curve
The natural C curve in the neck is important for optimal function as it ensures proper alignment of all the bones, tendons, and ligaments in the neck. Cervical fusion surgery not only alters the natural C curve in the neck but also adversely affects the curve in the lower back.
A new study demonstrated that patients who underwent cervical fusion noted changes in both the neck, tailbone, and pelvis curves. This often leads to the onset of pain and injury (9). - Infection
Infection is a devastating complication and was found to occur in 16.6% of patients in a recent study. Infection can involve the skin, muscle, or bone. Treatment involves antibiotics and wound care, and 47% of patients in a recent study required additional surgery for wound care and skin grafting. - Adjacent segment disease
Adjacent segment disease (ASD) is a common complication of neck fusion with an incidence of 21% (11). It occurs as a direct result of the fusion surgery, as the neck discs are designed to absorb the forces of daily living.
Fusing one or more discs together results in additional forces being placed on the disc and facet joints above and below the fusion. This additional pressure results in wear and tear and degeneration often requiring additional surgery. See our video below:
Recovering From Neck Fusion Surgery
Recovery from neck fusion surgery is a personalized journey influenced by factors such as the severity of the injury and the number of cervical levels fused. While surgical pain typically improves within one to three weeks, the road to recovery is individualized.
Physical therapy, a crucial component, begins approximately three to four hours post-surgery, focusing on strengthening and enhancing range of motion. The duration of recovery varies, but as patients progress through tailored rehabilitation, they often experience improved comfort and mobility.
Why Use This Treatment
Cervical fusion is recommended when individuals face circumstances of debilitating neck pain, herniated discs, or spinal instability that significantly impact their quality of life. This procedure becomes a viable option when diagnostic assessments reveal conditions such as antero listhesis, retrolisthesis, or craniocervical instability, and conservative treatments prove insufficient.
The severity of the cervical spine issue, coupled with persistent symptoms affecting daily activities, often guides healthcare professionals in recommending cervical fusion as a targeted solution to alleviate pain, stabilize the spine, and enhance overall well-being.
Alternatives To Cervical Spinal Fusion
There are several non-surgical treatment options for ongoing neck and arm pain. The appropriateness and success of these treatment options are based on the severity of the injury, current symptoms, and co-existing medication conditions. The most common treatments include:
Conservative Care
Conservative care, when appropriate, is the first-line treatment for neck and arm pain. Treatment options include rest, stretching, physical therapy, and chiropractic care. The goal is to reduce ongoing pain and increase function.
Medications
Medication is often used in conjunction with conservative care. Examples include anti-inflammatory agents and muscle relaxants. Oral steroids are often recommended when pain persists but should be avoided due to the significant side effects including destroying cartilage, depressing stem cell activity, and altering sugar levels.
To learn more about the adverse effects of steroids please click here.
Traditional ”Pain” Injections
When medication and conservative care fail, patients are often referred to a pain clinic for injections. These are STEROID injections and should be avoided.
Steroids are powerful anti-inflammatory agents with many side effects, as detailed above. Furthermore, they can accelerate the underlying problems. Steroids cannot heal an injured disc or facet joint. Steroids can only decrease the inflammation associated with the injury. Healing of a neck injury requires a regenerative option.
Regenerative Alternatives To Cervical Fusion
At the Centeno-Schultz Clinic we are experts in the treatment of neck pain. We are also experts in the use of PRP and bone marrow concentrate in the spine. In 2005, we became the first clinic in the world to inject bone marrow-derived stem cells into the disc.
We are also leaders in the field of regenerative medicine and interventional orthopedics. We have published extensively in recognized, peer-reviewed journals. Our list of publications is available here.
Our approach is very much different. Unlike the rushed, brief exam in most orthopedic offices, we spend a dedicated amount of time reviewing your chief complaint, its duration, aggravating and alleviating factors, treatment to date, past medical history, medications, and events that led to the injury. We also review detail all imaging in detail, including X-ray, MRI, and CT scans.
Our approach is comprehensive in nature, as we believe the body functions as a unit. For example, examination of the shoulders is critical when evaluating patients with neck pain. This is because many patients with low neck pain also have ongoing shoulder problems.
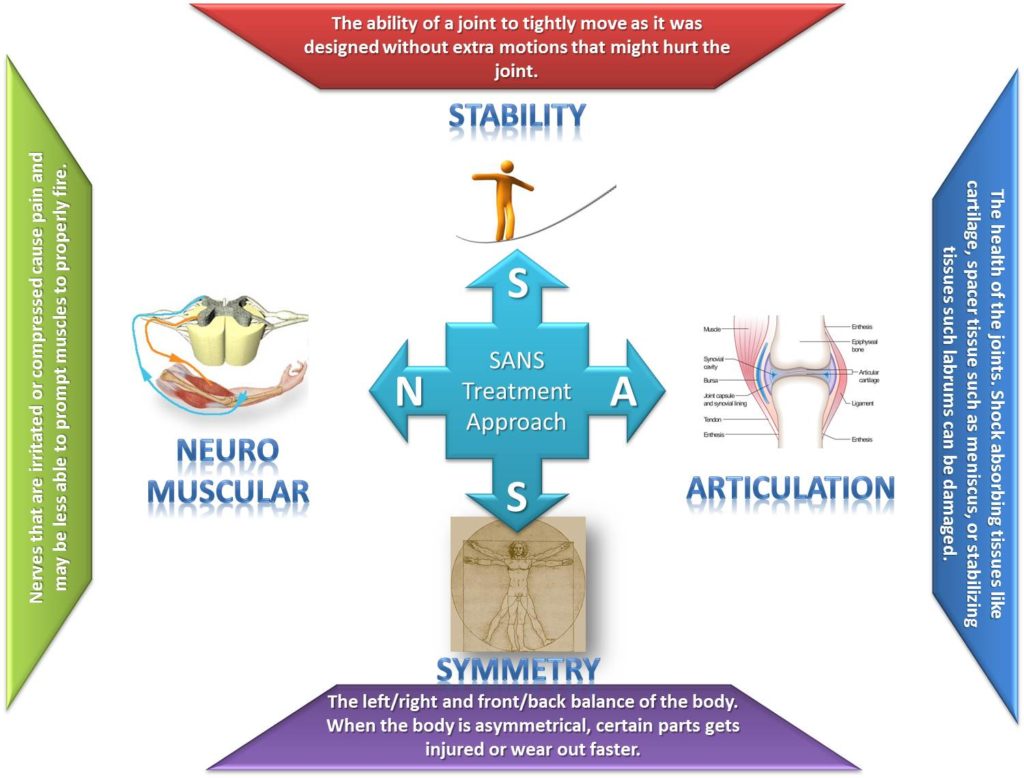
The approach is referred to as SANS which stands for Stability, Articulation, Neuro-Muscular, and Symmetry. To learn more about our SANS approach please click here.
At the Centeno Schultz Clinic, there is an extensive number of regenerative treatment options for patients with ongoing neck and or arm pain. The specific treatment for any patient will depend upon the underlying cause of the pain, its severity, and the patient’s symptoms.
Treatment options include both PRP and bone marrow concentrate, which contains stem cells. We utilize customized PRP injections to ensure the best clinical results. It is important, as middle-aged and older patients require higher concentrations of PRP than younger patients. To learn more about the importance of PRP concentration, please click here.
Both bone marrow concentrate and PRP are precisely injected into the neck using X-ray and ultrasound guidance. The injections are challenging and cannot be performed by your surgeon, chiropractor, or physician assistant. To watch a Centeno-Schulz Clinic injection click on the video below.
Get Expert Guidance For Your Cervical Spine
transformative journey with Centeno-Schultz Clinic. Beyond medical expertise, this clinic offers a guiding partnership on your path to well-being. With a commitment to personalized care, cutting-edge treatments, and a compassionate approach, Centeno-Schultz Clinic becomes your ally in navigating the complexities of cervical spine issues.
Trust in the expertise that goes beyond the procedural, extending to comprehensive support, empowering you to reclaim a life of comfort and vitality. Choose more than a clinic; choose a dedicated partner on your journey to a healthier and pain-free tomorrow.

Christopher J. Centeno, MD
Christopher J. Centeno, M.D. is an international expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate in orthopedics. He is board-certified in physical medicine and rehabilitation with a subspecialty of pain medicine through The American Board of Physical Medicine and Rehabilitation. Dr. Centeno is one of the few physicians in the world with extensive experience in the culture expansion of and clinical use of adult bone marrow concentrate to treat orthopedic injuries. His clinic incorporates a variety of revolutionary pain management techniques to bring its broad patient base relief and results. Dr. Centeno treats patients from all over the US who…
Read more
John Schultz, MD
John R. Schultz M.D. is a national expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate for orthopedic injuries. He is board certified in Anesthesiology and Pain Medicine and underwent fellowship training in both. Dr. Schultz has extensive experience with same day as well as culture expanded bone marrow concentrate and sees patients at the CSC Broomfield, Colorado Clinic, as well the Regenexx Clinic in Grand Cayman. Dr. Schultz emphasis is on the evaluation and treatment of thoracic and cervical disc, facet, nerve, and ligament injuries including the non-surgical treatment of Craniocervical instability (CCI). Dr. Schultz trained at George Washington School of…
Read more
John Pitts, M.D.
Dr. Pitts is originally from Chicago, IL but is a medical graduate of Vanderbilt School of Medicine in Nashville, TN. After Vanderbilt, he completed a residency in Physical Medicine and Rehabilitation (PM&R) at Emory University in Atlanta, GA. The focus of PM&R is the restoration of function and quality of life. In residency, he gained much experience in musculoskeletal medicine, rehabilitation, spine, and sports medicine along with some regenerative medicine. He also gained significant experience in fluoroscopically guided spinal procedures and peripheral injections. However, Dr. Pitts wanted to broaden his skills and treatment options beyond the current typical standards of care.
Read more
Jason Markle, D.O.
Post-residency, Dr. Markle was selected to the Interventional Orthopedic Fellowship program at the Centeno-Schultz Clinic. During his fellowship, he gained significant experience in the new field of Interventional Orthopedics and regenerative medicine, honing his skills in advanced injection techniques into the spine and joints treating patients with autologous, bone marrow concentrate and platelet solutions. Dr. Markle then accepted a full-time attending physician position at the Centeno-Schultz Clinic, where he both treats patients and trains Interventional Orthopedics fellows. Dr. Markle is an active member of the Interventional Orthopedic Foundation and serves as a course instructor, where he trains physicians from around the world.
Read more
Brandon T. Money, D.O., M.S.
Dr. Money is an Indiana native who now proudly calls Colorado home. He attended medical school at Kansas City University and then returned to Indiana to complete a Physical Medicine and Rehabilitation residency program at Indiana University, where he was trained on non-surgical methods to improve health and function as well as rehabilitative care following trauma, stroke, spinal cord injury, brain injury, etc. Dr. Money has been following the ideology behind Centeno-Schultz Clinic and Regenexx since he was in medical school, as he believed there had to be a better way to care for patients than the status quo. The human body has incredible healing capabilities…
Read moreAm I a Candidate?
To answer this question, fill out the candidate form below to request a new patient evaluation, and a patient advocate will reach out to you to determine your next steps. Your one-hour, in-office or telemedicine evaluation will be with one of the world’s experts in the field of Interventional Orthopedics.