Costochondritis of the Thoracic Spine
Costochondritis is a medical condition that causes inflammation of the cartilage that connects a rib to the sternum (or breastbone). The term “costo” refers to the ribs, “chondro” refers to cartilage, and “itis” refers to inflammation. Costochondritis typically presents as chest pain and discomfort. It can be sharp in character and may mimic the pain associated with angina or heart attack.
What Is Costochondritis?
The ribs connect to the sternum through a combination of cartilage and joints that form the thoracic cage. The thoracic cage protects vital organs such as the heart and lungs.
The end of the rib connects with the costal cartilage, which in turn connects with the sternum. There are two important joints formed.
The costochondral joints are the joints formed between the ends of the ribs and the costal cartilage. They are lined with cartilage and surrounded by a fibrous capsule similar to the knee joint.
Sternochondral joints are the joints formed by the union of the costal cartilage and the sternum. They are synovial joints, which have a lubricant that allows them to move effortlessly.
Costochondritis is the inflammation of the cartilage that connects the ends of the ribs to the sternum. (1)
The most common age for costochondritis is middle age (between 40 and 50 years of age) with a slight predominance in women (69%) vs. men (56%). (2)
- Why is costochondritis so painful?
The cartilage connecting the ribs to the sternum allows for movement during breathing. With inhalation, the ribcage expands as the ribs move upward and outward. This draws fresh air into the lungs.
With exhalation, the ribcage contracts, and the ribs move down into their resting position. The flexible cartilage that connects the ribs to the breastbone allows for this movement. When the cartilage is inflamed it can become swollen and tender to the touch. This becomes quite painful as the cartilage moves up and back down with each breath. Ouch.
Nerves that course along the cartilage and ribs can also be inflamed, causing additional pain and dysfunction with each breath.
Many physicians will run tests, such as blood tests, X-rays, and ECG (electrocardiograms) to rule out more serious conditions. (3)
Is Costochondritis Serious?
Costochondritis is not considered a serious or life-threatening condition. It is an inflammation of the cartilage that connects your ribs to your breastbone and the joints therein and can cause moderate to severe chest pain and discomfort.
It is often mistaken for more serious conditions such as a heart attack or pulmonary embolism, which is why it is important to seek medical evaluation if you have chest pain.
- How long does it take for it to go away?
The duration of costochondritis can vary from patient to patient. In most cases, costochondritis is a self-limiting condition, meaning it tends to improve and resolve in its own time. The pain and discomfort associated with costochondritis typically lessen over several weeks to a few months.
Duration of symptoms can be influenced by several factors:
- Individual variation: Some patients may experience relief in a matter of weeks, whereas others have symptoms that persist for a few months.
- Treatment: Once the diagnosis is confirmed, proper treatment can help alleviate symptoms more quickly. Ice, rest, and NSAIDs such as Motrin can help reduce inflammation and discomfort.
- Lifestyle: Avoiding activities that exacerbate symptoms can help with recovery.
Symptoms of Costochondritis
Costochondritis is the inflammation of the cartilage and the joints that connect the ribs to the breastbone (sternum). Symptoms can vary from patient to patient. The most common symptoms include:
Chest Pain on Either Side of the Sternum
The hallmark symptom of costochondritis is chest pain, which can vary in intensity and location. It is often described as sharp, stabbing or aching pain that is located on one side of the chest.
Tenderness
Costochondritis commonly causes tenderness at the junction of the ribs and sternum.
Nausea
In severe cases of costochondritis, the pain and discomfort can lead to nausea.
Pain with Breathing
With inhalation and exhalation, there is movement of the chest wall and costocartilage, which can cause significant pain.
Increased Pain with Movement
Activities that involve chest wall movements, such as coughing, sneezing, or exertion can worsen the pain of costochondritis.
Swelling
In severe cases of costochondritis, patients may note mild swelling or inflammation of the costochondral cartilage or costochondral joints.
Common Causes of Costochondritis
Costochondritis typically has no clear cause and it can develop spontaneously without an apparent cause. Several factors have been associated with the development of costochondritis:
Overuse or Repetitive Strain
Activities or movements that repeatedly stress the chest area, such as heavy lifting, strenuous exercise, or frequent coughing, can potentially contribute to the development of costochondritis.
Trauma to the Chest Wall
A direct blow to the chest, such as a fall or car accident can sometimes lead to inflammation of the cartilage in the rib cage, resulting in costochondritis.
Inflammation of the Joints
Osteoarthritis, rheumatoid arthritis, ankylosing spondylitis, and other cartilage-related disorders can occasionally lead to costochondritis.
Infections
Viral respiratory infections, such as the common cold or flu, as well as bacterial infections, can potentially lead to costochondritis.
Common Treatments for Costochondritis
Costochondritis is a self-limiting medical condition characterized by inflammation of the costochondral cartilage and its joints. Treatment varies depending on the patient, the pain level, and dysfunction.
Prescribed Medication
- NSAIDs (Nonsteroidal anti-inflammatory drugs): These are powerful anti-inflammatory agents that can reduce inflammation, swelling, and discomfort. Common examples include ibuprofen, Naproxen, and Voltaren.
- Acetaminophen: This medication is NOT an anti-inflammatory agent but is effective in reducing mild to moderate pain.
- Oral narcotics: In severe cases, oral narcotics may be prescribed. Common examples include Percocet and Vicodin. Narcotics have significant side effects, including addiction and should be limited.
- Corticosteroids: Steroids are powerful anti-inflammatory agents that can reduce inflammation, swelling, and pain. Examples include prednisone, dexamethasone, and hydrocortisone. There are significant side effects, and for this reason, these medications should be avoided.
- Tricyclic antidepressants: These medications are often used to control pain, especially if the pain interferes with sleep. Examples include Amitriptyline and Imipramine.
- Antiseizure drugs: Epilepsy medications such as gabapentin (Neurontin) have been effective in controlling the chronic pain associated with costochondritis.
- Antibiotics for infections: Antibiotics can be used to combat underlying bacterial or fungal infections contributing to the condition. It is important to consult with your doctor to determine the appropriate antibiotic treatment for costochondritis.
PRP Treatment for Costochondritis
Costochondritis is a medical condition characterized by the inflammation of the costochondral cartilage and its joints. Traditional treatment involves the use of supportive therapy, which decreases the symptoms. Common examples include NSAIDs, ice, and rest.
Clinical outcomes improve when you directly treat the underlying condition as opposed to the symptoms. Medications like NSAID and oral steroids have significant side effects and should be avoided.
PRP is a new treatment option for costochondritis. PRP stands for platelet-rich plasma and is currently used in the treatment of many musculoskeletal injuries. PRP treatment involves the use of a patient’s own blood to promote healing and reduce pain. Basic steps include:
- Collection: Blood is drawn from a patient’s arm, much like a standard blood test.
- Centrifugation: The blood is placed in a centrifuge that spins at high speeds to separate it into three components: plasma, buffy coat, and red blood cells.
- Concentration: The platelets are isolated and concentrated.
- Injection: The concentrated pellet of platelets is then injected into the damaged area.
PRP is rich in growth factors that can accelerate healing. One of the main growth factors is VEGF, which can increase blood flow and promote healing. The rationale for the use and therapeutic potential of a high concentration of platelets is based on their capacity to supply supraphysiologic amounts of essential growth factors to provide a regenerative stimulus that promotes repair in tissues with low healing potential. (4)
With costochondritis, the goal is to reduce inflammation of the costochondral cartilage and enhance the stabilization of the rib connection to the sternum.
Here is a short video on what PRP does:
Are There Different Kinds of PRP?
Yes! Not all PRP is the same and this can make a significant difference in clinical outcomes. Please watch the video below on how to differentiate between good and poor PRP.
An important factor in the use and success of PRP in the treatment of musculoskeletal injuries and costochondritis is the actual PRP dose. The higher the PRP concentration, the larger the number of growth factors that are available to promote healing. This is a critical factor in the treatment of patients over 30 years of age.
Unfortunately, most clinics cannot super concentrate PRP, as their bedside centrifuges have very limited capability. At the Centeno-Schultz Clinic, we acknowledge the importance of customizing PRP treatments for each patient. We have a state-of-the-art university stem cell and cell laboratory that allows us to superconcentrate PRP treatment to the needs of each patient.
There are different types of PRP, which include:
- Red or leukocyte-rich PRP: leukocytes are white blood cells (WBC). Leukocyte-rich PRP refers to a type of PRP that contains a higher concentration of white blood cells compared to other PRP formulations.
- Amber or leukocyte-poor PRP: This type of PRP contains small amounts of white blood cells.
- Autologous conditioned serum: Also known as “Othrokine” or “Regenokine,” this is a specific blood product in which anti-inflammatory factors are removed from a patient’s blood and injected into painful areas. The principal anti-inflammatory factor is called IRAP, which stands for interleukin receptor antagonist therapy.(3) It is obtained by taking the serum from blood and incubating it with zinc-etched glass beads. Interleukin-1 is a powerful protein that causes inflammation. An antagonist is an agent that blocks the effect of another substance. So, IRAP is simply a powerful protein that blocks inflammation.
- Platelet lysate: A specialized PRP in which the envelope that contains the growth factors is opened up and is immediately available for healing.
To learn more about platelet lysate please link to the video below.
Are There Dangers with PRP Injections for Costochondritis?
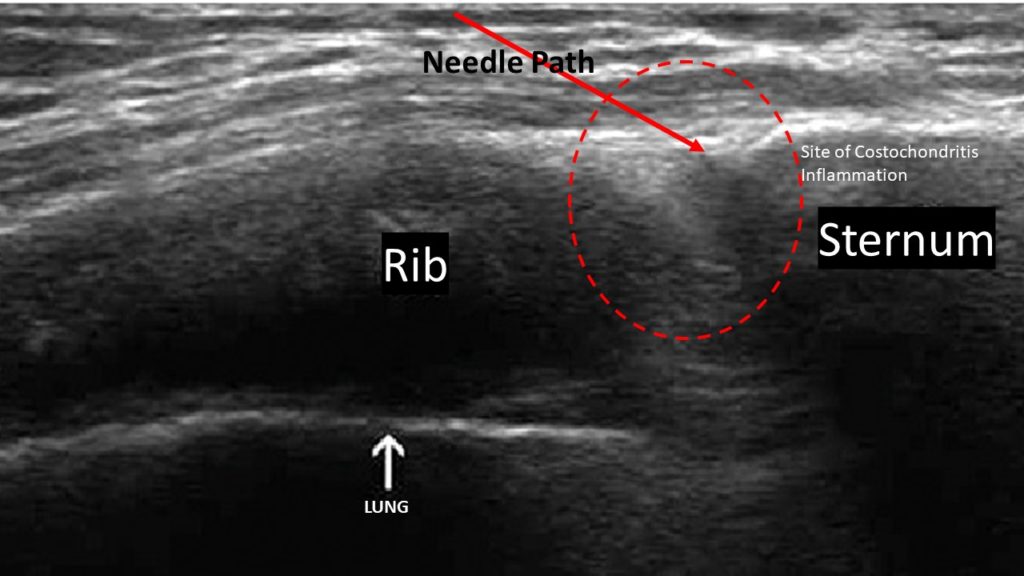
PRP injections for costochondritis are not injections that your PCP or orthopedic surgeon can perform. Why?
The anatomy is complex and the lungs are immediately underneath the costocartilage and rib. If the needle is aimed incorrectly or advanced too far, it can injure and collapse the lung, which may cause significant cardiovascular complications.
A thorough understanding of the anatomy and expertise in ultrasound are essential. In addition, physicians must be able to accurately advance the needle under ultrasound guidance.
At the Centeno-Schultz Clinic, all physicians are board-certified, fellowship-trained, and have expertise in the use of X-ray and ultrasound-guided procedures. It takes years of dedicated study to achieve this level of expertise.
Treat Costochondritis the Centeno-Schultz Clinic Way
Costochondritis is the inflammation of the costochondral cartilage and the costochondral and sternochondral joints. It is a painful medical condition because the ribs and associated cartilage move with each breath. It is not a serious or life-threatening condition; however, it can mimic more serious conditions such as a heart attack or pulmonary embolism. Hence, it should be evaluated by a medical professional.
Symptoms include chest pain, point tenderness, nausea, and pain with breathing. While there is no clear cause of costochondritis, it is associated with repetitive strains, trauma to the chest wall, inflammation of the chest wall secondary to arthritis, and infections.
Treatments are supportive and aimed at decreasing symptoms. Common medications include NSAIDs, acetaminophen, oral narcotics, and steroids.
PRP is rich in growth factors that can increase blood flow and reduce inflammation. PRP can be effective in the treatment of costochondritis. It is an advanced procedure, given the proximity of the lungs and the potential complication of lung puncture.
At the Centeno-Schultz Clinic, we are experts in the evaluation and treatment of thoracic pain, including costochondritis. Not all PRP or regenerative clinics are the same. Years of expertise and fellowship training make a big difference. If you are sidelined by costochondritis, consider an in-office or online consultation.
Are you a Candidate?
John Schultz, MD
John R. Schultz M.D. is a national expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate and PRP for orthopedic injuries. He is board certified in Anesthesiology and Pain Medicine and underwent fellowship training. Dr. Schultz has extensive experience with same day as well as culture expanded bone marrow concentrate and sees patients at the CSC Broomfield, Colorado Clinic, as well the Regenexx Clinic in Grand Cayman. Dr. Schultz emphasis is on the evaluation and treatment of thoracic and cervical disc, facet, nerve, and ligament injuries including the non-surgical treatment of Craniocervical instability (CCI).
Other Resources for Costochondritis of the Thoracic Spine
References:
- Schumann JA, Parente JJ. Costochondritis. [Updated 2019 Jun 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan. Available from this page.
- Disla E, Rhim HR, Reddy A, Karten I, Taranta A. Costochondritis. A prospective analysis in an emergency department setting. Arch Intern Med. 1994 Nov 14;154(21):2466-9. doi: 10.1001/archinte.154.21.2466. PMID: 7979843.
- ANNE M. PROULX, DO, and TERESA W. ZRYD, MD, MSPH Costochondritis: Diagnosis and Treatment, Wright State University Boonshoft School of Medicine, Dayton, Ohio; Available from this page.
- Wu PI, Diaz R, Borg-Stein J. Platelet-Rich Plasma. Phys Med Rehabil Clin N Am. 2016;27(4):825-53.