The fibula is a little bone that can cause quite a bit of trouble. Fibular head pain has many causes and we’ll review them here and also what can be done. Let’s dig in.
What is the Proximal Fibula?
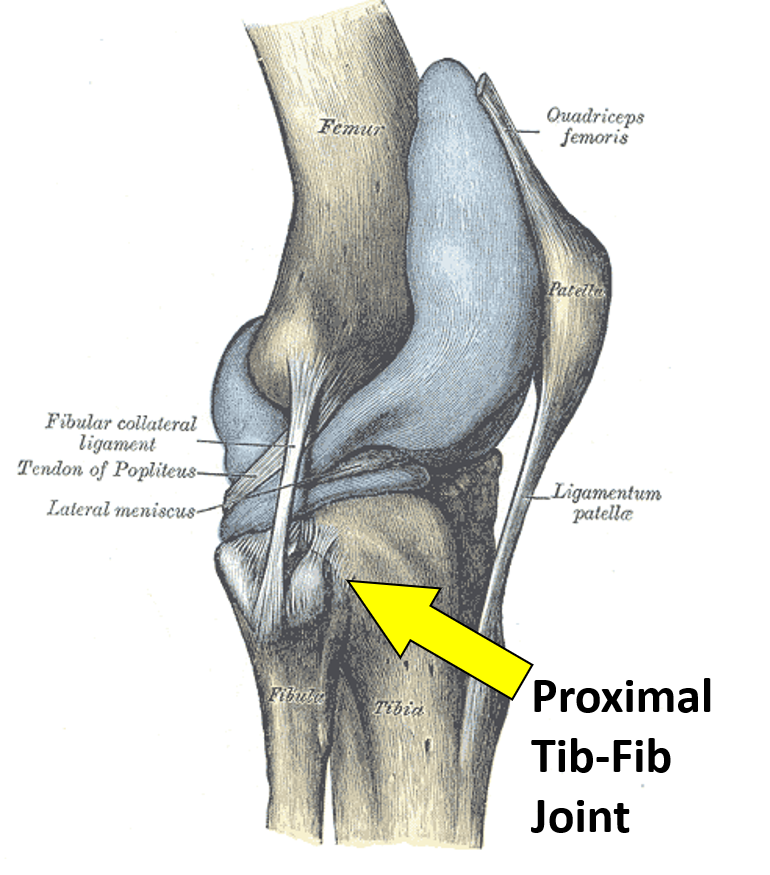
The proximal fibula is the part of the bone that lives just below the knee joint on the outside. It’s attached to the leg bone (tibia) via strong ligaments and there is a small joint here. There are many things that attach here, so it’s a critical point where pain can occur.
The Proximal Tibiofibular Joint
There is a small joint between the fibula and the tibia known as the proximal tibiofibular joint. This is a plane type joint which allows some sliding of the fibula on the tibia. It has cartilage just like the knee joint, so it can get arthritis which means worn down cartilage and bone spurs.
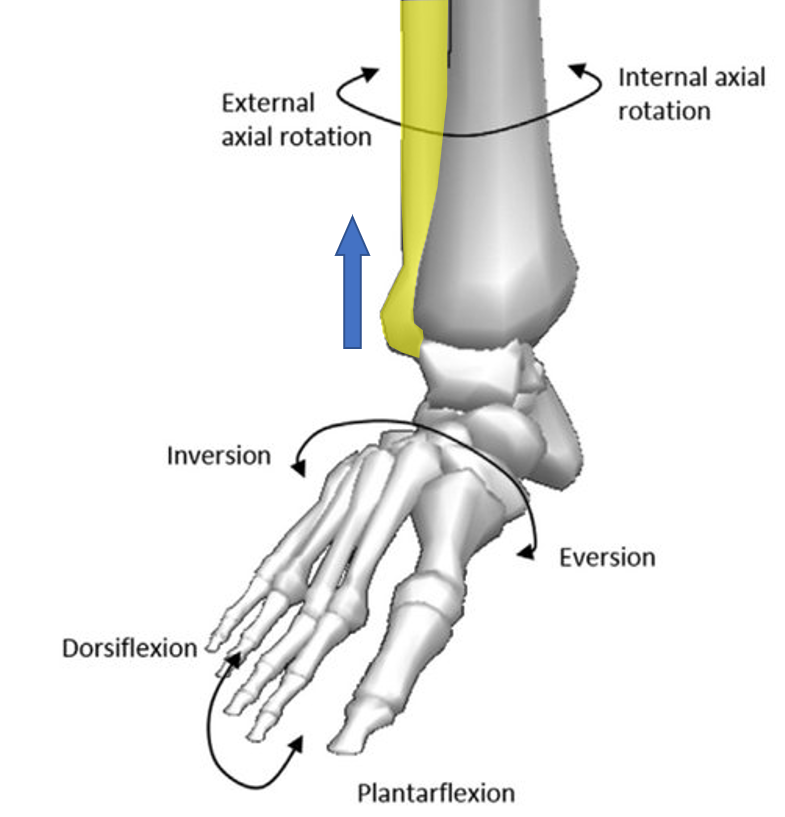
The job of this proximal “tib-fib” joint is to absorb the stresses from the rotation of the tibia that are transmitted up from the ankle during walking and running. In addition, since the fibula connects the ankle and the knee, an upward force is also apllied here when the foot everts (see image to the left with fibula highlighted in yellow) (1). Hence, if the ligaments that hold the fibula to the tibia are loose, this can have impacts that extend all the way down to the ankle.
What Attaches to the Fibular Head?
Lots of things that attach here can cause fibular head pain which include:
- Biceps femoris
- Lateral collateral ligament
- Popliteofibular ligament
- Tibiofibular ligaments
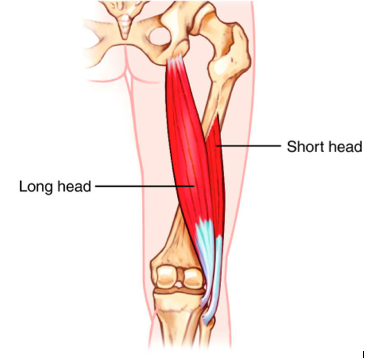
The biceps femoris is the outside hamstrings muscle (short head of the biceps femoris) that inserts here at the fibula (image here to the left). This tendon can cause fibular head pain when there are problems with the muscle and the tendon gets too much wear and tear. That can happen due to imbalances in the body or even if there are irritated nerves in the low back that impact the muscle and tendon.
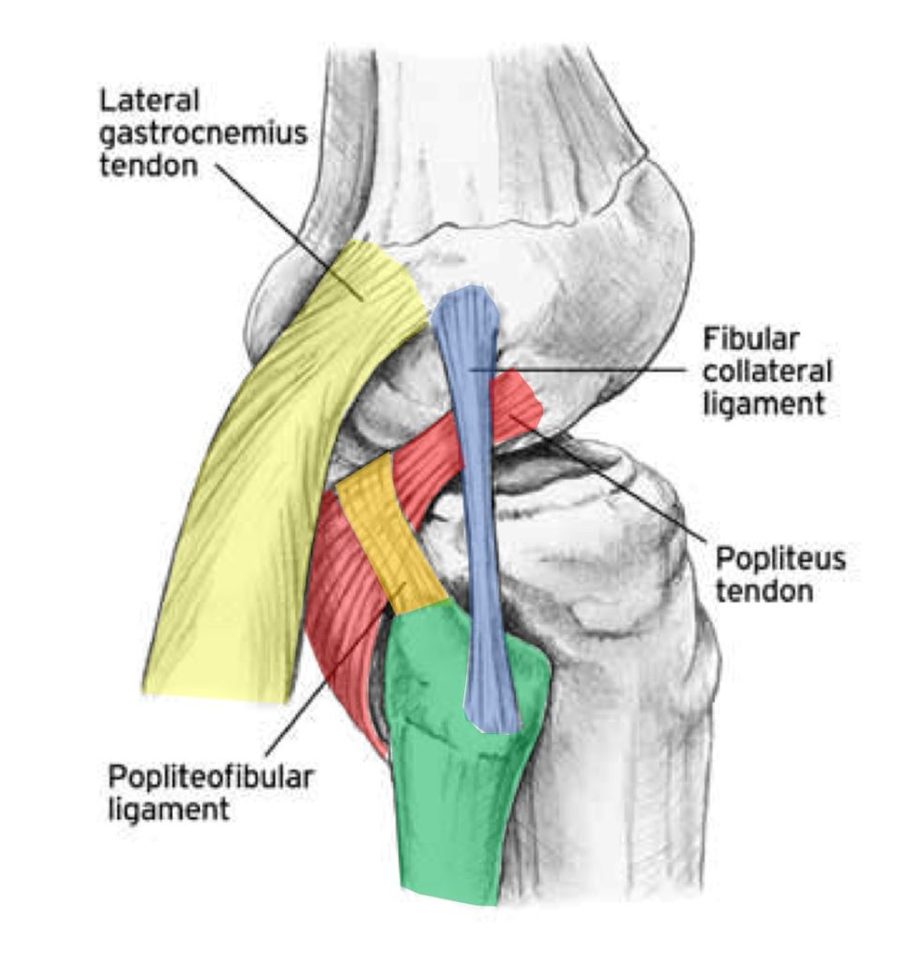
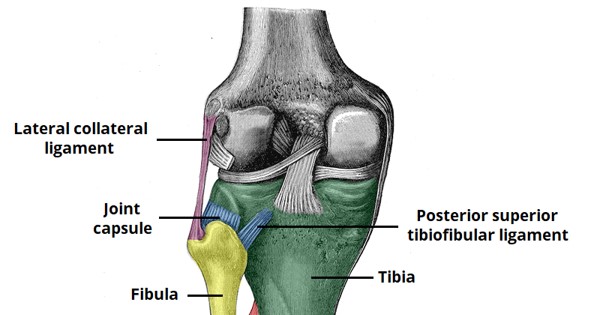
The lateral collateral ligament (LCL) is on the side of the knee and stabilizes the outside of that joint (blue in the diagram shown here). This ligament supports the knee when inward pressure is placed. It can become injured in sports or just wear and tear. When the ligament is loose, this can cause too much wear and tear in the joint and arthritis. This can also cause local pain where the ligament attaches. In addition, being loose means that the joint is unstable, injuring other structures over time like the cartilage, bone, and meniscus.
The popliteofibular ligament (orange in the image shown here) begins at the fibula and travels upward and over the popliteus tendon. It helps with the stability of the knee like the LCL and ACL. It can become injured, leaving the knee joint slightly unstable or it can be part of what’s called, posterior-lateral instability. It can also be painful when injured.
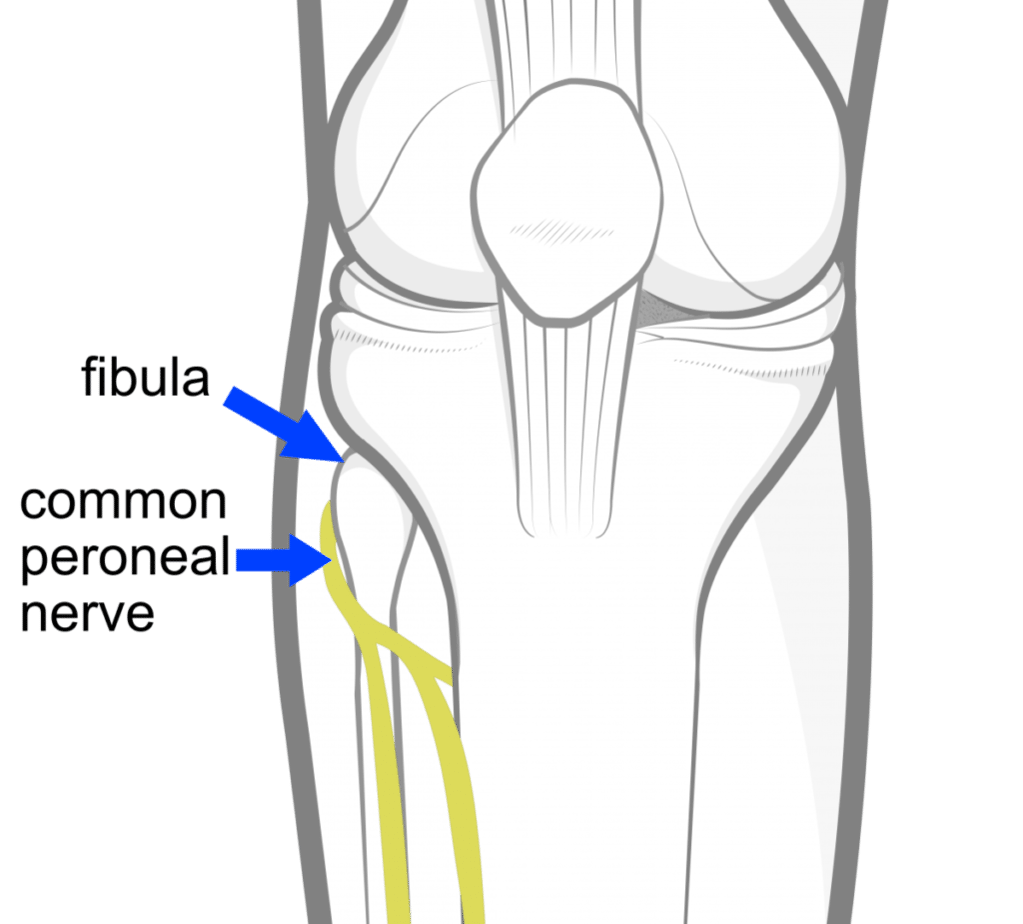
The tibiofibular ligaments attach the fibula to the tibia and help stabilize the posterior lateral corner of the knee (blue in the image here attaching the yellow fibula to the tibia). When these ligaments become too loose this can cause the fibula to become unstable and fibular head pain. Since there is a joint here between these two bones, if this bone moves too much the joint can be damaged and become arthritic. In addition, this excessive movement can cause the peroneal nerve that wraps around the fib head here to become irritated.
Why is My Fibula Hurting?
Fibular head pain primary causes can be broken down into a few categories:
- Unstable or damaged Joint
- Tight hamstrings
- Irritated nerves
Unstable or damaged joint
If the ligaments that hold the fibula to the tibia are loose or damaged, this causes too much motion or fibular head instability. The joint here between the two bones can become arthritic or swollen, which can cause pain. These ligaments include the tibiofibular and lateral collateral. Many people with the instability of the head of fibula don’t know it until an experienced manual physical therapist or physician tests the stability of the bone side to side, finding that one fibula moves dramatically more than the other. This is not usually part of the typical orthopedic exam.
Tight Hamstrings
The outside hamstrings muscle attaches to the fib head. When this muscle is chronically tight that can cause the tendon to get ripped up through wear and tear, a condition that’s known as tendinopathy. This can pain can be made worse when the hamstring muscle is used, for example in the gym when leg curls are performed.
Irritated Nerves
The peroneal nerve wraps around the fibular head (see image to the left). Hence, if the fibular head is unstable due to damaged ligaments, the nerve can get irritated. This can lead to numbness, tingling, burning, or just referred pain down the front of the leg and foot. Also, realize that the S1 nerve in the low back can also send pain signals to the outside of the knee, so an irritated nerve in the low back can cause fib head pain.
In addition to the above, the way the knee moves as you walk or run can cause issues. Watch my video below to understand that better:
Conditions That Can Cause Fibula Pain
Ehlers-Danlos Syndrome (EDS)
Disorders that affect and weaken the connective tissues such as tendons and ligaments. It is a hereditary disorder which means you are born with it. EDS has many different signs and symptoms which can vary significantly depending upon the type of EDS and its severity. It most commonly affects the skin, joints, and blood vessels. Joints are typically hypermobile with excessive joint range of motion because of a defect in collagen formation. In most cases Ehlers-Danlos syndrome is inherited. That is to say that you are born with it. The two main ways EDS is inherited are: autosomal dominant inheritance and autosomal recessive inheritance…
Read More About Ehlers-Danlos Syndrome (EDS)Hamstrings Tendinopathy
Hamstring tendinopathy, a condition that causes pain and tenderness in the hamstring tendons, represents a common but often misunderstood musculoskeletal issue. It typically occurs in athletes and individuals engaged in high-intensity activities but isn’t limited to them. This condition, including its more specific form, high hamstring tendinopathy, can significantly impact daily and athletic performance, making understanding its nuances critical.
Read More About Hamstrings TendinopathyKnee Arthritis
In the human body, a joint is simply where 2 ends of bone come together. At the ends of these bones, there is a thick substance called “Hyaline Cartilage” that lines the ends. Hyaline cartilage is extremely slippery which allows the two ends of the bone to slide on top of each other. Then there is a capsule that connects the two ends filled with “synovial fluid” that acts as a further lubricant to make it more slippery! Arthritis in the knee is defined by loss of the hyaline cartilage plus other changes that happen to the bone such as additional bone being laid down (bone spurs/osteophytes). The cartilage layer is worn down to the point of exposing the underlying bone they cover…
Read More About Knee ArthritisKnee Instability
Knee instability is a condition that results when the knee joint is unstable and does not move or function normally. This can cause the knee to feel like it is going to give out or buckle. Knee instability can be caused by a variety of factors, including trauma or injury to the knee, ligament injury, arthritis or other degenerative diseases of the knee, weakness or instability of the muscles around the knee, muscle atrophy, injury to another joint in the body creates an imbalance. Knee stability, and stability in general, is very important. Lack of knee stability can lead to more problems over time, such as pain and arthritis…
Read More About Knee InstabilityLCL Sprain
What is an LCL Sprain? A strain or tear to the lateral collateral ligament (LCL) is known as an LCL injury. The LCL is a band of tissue that runs along the outer side of your knee. It aids in keeping the bones together while you walk, ensuring that your knee joint remains stable. How you feel and what type of treatment you’ll require depends on how severely your LCL has been stretched or torn. If it’s only a minor sprain, self-care at home might help. However, if it’s a significant tear or sprain, you may need physical therapy, an injection-based procedure, or surgery….
Read More About LCL SprainLCL Tear
A strain or tear to the lateral collateral ligament (LCL) is known as an LCL injury. The LCL is a band of tissue that runs along the outer side of your knee. It aids in keeping the bones together while you walk, ensuring that your knee joint remains stable. How you feel and what type of treatment you’ll require depends on how severely your LCL has been stretched or torn. If it’s only a minor sprain, self-care at home might help. However, if it’s a significant tear, you may need physical therapy, an injection-based procedure, or surgery. Orthopedists categorize LCL tears into 3 grades…
Read More About LCL TearPeroneal Nerve Injury
The common peroneal nerve branches behind the knee and this could be irritated from any overuse activity, surgery, instability, or any compression on the outside of the knee. Typically, this will present as pain on the outside of the knee radiating towards the baby toe, the calf, and the lateral shin towards the lateral ankle. What Causes Peroneal Nerve Compression? There are many potential causes of peroneal nerve compression, such as overuse activities, surgery, instability, or any compression on the outside of the knee. Trauma and nerve compression, especially caused by a fractured or dislocated ankle, can all cause injury to the peroneal nerve. Causes include:
Read More About Peroneal Nerve InjuryHow Do You Fix Fibular Head Pain?
Treatment here depends on what’s causing the problem. For most acute pain that’s been present for only days to weeks, rest and/or physical therapy is usually the answer. For more chronic pain that’s been there longer, a diagnosis of which of the above problems is causing the pain is critical.
For example, if we take the above causes of pain, here are some things that can be done:
For an unstable or damaged joint, simple solutions that are commonly offered include a steroid injection into the area of joint. One problem here is that while this is a potent anti-inflammatory that can help reduce swelling and pain on a temporary basis, these steroid shots also kill cartilage (2). Newer orthobiologic injections like platelet-rich plasma (PRP) don’t have the same damaging effects on cartilage and have been shown to work well in larger joints like the knee (3-5). In addition, PRP and bone marrow concentrate (containing stem cells) have shown success in healing damaged ligaments, hence these injections might be used to help heal the loose ligaments and tighten down the instability (6-8). Other options include surgical repair of the tibiofibular ligaments, but the need for that surgery is rare (12).
The biceps tendinopathy described above again is often treated with a steroid injection, but such injections in other tendons have been shown to be inferior to PRP (9). Again, this likely stems from the fact that steroid medications can damage tendon cells while PRP can enhance tendon repair (10,11). Hence, PRP is your best bet here.
The treatment for irritated nerves like the common peroneal as it wraps around the fibular head is usually stabilizing the fibula through physical therapy or PRP injection. If there is still an issue after those treatments, then surgical release is possible, but again, the need for that procedure is rare (13). In addition, if the problem is an irritated spinal nerve in the low back, then an epidural injection can be used to treat that problem (14).
The upshot? A little bone at the side of your leg can cause big problems. Fibular bone pain is quite real and getting to a specific diagnosis of what’s causing the pain is key. Once you have that cause, then a treatment can be formulated to fix the problem.
References:
(1) Sarma A, Borgohain B, Saikia B. Proximal tibiofibular joint: Rendezvous with a forgotten articulation. Indian J Orthop. 2015;49(5):489–495. doi:10.4103/0019-5413.164041
(2) McAlindon TE, LaValley MP, Harvey WF, et al. Effect of Intra-articular Triamcinolone vs Saline on Knee Cartilage Volume and Pain in Patients With Knee Osteoarthritis: A Randomized Clinical Trial. JAMA.2017;317(19):1967–1975. doi: 10.1001/jama.2017.5283
(3) Xing D, Wang B, Zhang W, Yang Z, Hou Y1,2, Chen Y, Lin J. Intra-articular platelet-rich plasma injections for knee osteoarthritis: An overview of systematic reviews and risk of bias considerations. Int J Rheum Dis. 2017 Nov;20(11):1612-1630. doi: 10.1111/1756-185X.13233.
(4) Filardo G, Kon E, Buda R, Timoncini A, Di Martino A, Cenacchi A, Fornasari PM, Giannini S, Marcacci M. Platelet-rich plasma intra-articular knee injections for the treatment of degenerative cartilage lesions and osteoarthritis. Knee Surg Sports Traumatol Arthrosc. 2011 Apr;19(4):528-35. doi: 10.1007/s00167-010-1238-6.
(5) Southworth TM, Naveen NB, Tauro TM, Leong NL, Cole BJ. The Use of Platelet-Rich Plasma in Symptomatic Knee Osteoarthritis. J Knee Surg. 2019 Jan;32(1):37-45. doi: 10.1055/s-0038-1675170.
(6) Centeno CJ, Pitts J, Al-Sayegh H, Freeman MD. Anterior cruciate ligament tears treated with percutaneous injection of autologous bone marrow nucleated cells: a case series. J Pain Res. 2015;8:437–447.
(7) Centeno C, Markle J, Dodson E, et al. Symptomatic anterior cruciate ligament tears treated with percutaneous injection of autologous bone marrow concentrate and platelet products: a non-controlled registry study. J Transl Med. 2018;16(1):246.
(8) Koch M, Mayr F, Achenbach L, et al. Partial Anterior Cruciate Ligament Ruptures: Advantages by Intraligament Autologous Conditioned Plasma Injection and Healing Response Technique-Midterm Outcome Evaluation. Biomed Res Int. 2018;2018:3204869. https://www.ncbi.nlm.nih.gov/pubmed/30148163
(9) Xu Q, Chen J, Cheng L. Comparison of platelet rich plasma and corticosteroids in the management of lateral epicondylitis: A meta-analysis of randomized controlled trials. Int J Surg. 2019 Jul;67:37-46. doi: 10.1016/j.ijsu.2019.05.003.
(10) McQuillan, R., & Gregan, P. (2005). Tendon rupture as a complication of corticosteroid therapy. Palliative Medicine, 19(4), 352–353. https://doi.org/10.1177/026921630501900412
(11) Alsousou J, Thompson M, Harrison P, Willett K, Franklin S. Effect of platelet-rich plasma on healing tissues in acute ruptured Achilles tendon: a human immunohistochemistry study. Lancet. 2015 Feb 26;385 Suppl 1:S19. doi: 10.1016/S0140-6736(15)60334-8.
(12) Fanelli GC, Fanelli DG. Fibular head-based posterolateral reconstruction of the knee combined with capsular shift procedure. Sports Med Arthrosc Rev. 2015 Mar;23(1):33-43. doi: 10.1097/JSA.0000000000000042.
(13) Morimoto D, Isu T, Kim K, et al. Microsurgical Decompression for Peroneal Nerve Entrapment Neuropathy. Neurol Med Chir (Tokyo). 2015;55(8):669–673. doi:10.2176/nmc.oa.2014-0454
(14) Centeno C, Markle J, Dodson E, et al. The use of lumbar epidural injection of platelet lysate for treatment of radicular pain. J Exp Orthop. 2017;4(1):38. Published 2017 Nov 25. doi:10.1186/s40634-017-0113-5