Knee ligament surgeries have become quite common, ACL (anterior cruciate ligament) surgeries average 250,000+ surgeries alone every year (1)! These invasive surgeries have come under investigation in recent years, wondering the necessity, or need to be done. Today lets understand the knee a little better and take a look at the need for a knee ligament surgery, in addition, look into alternative treatments.
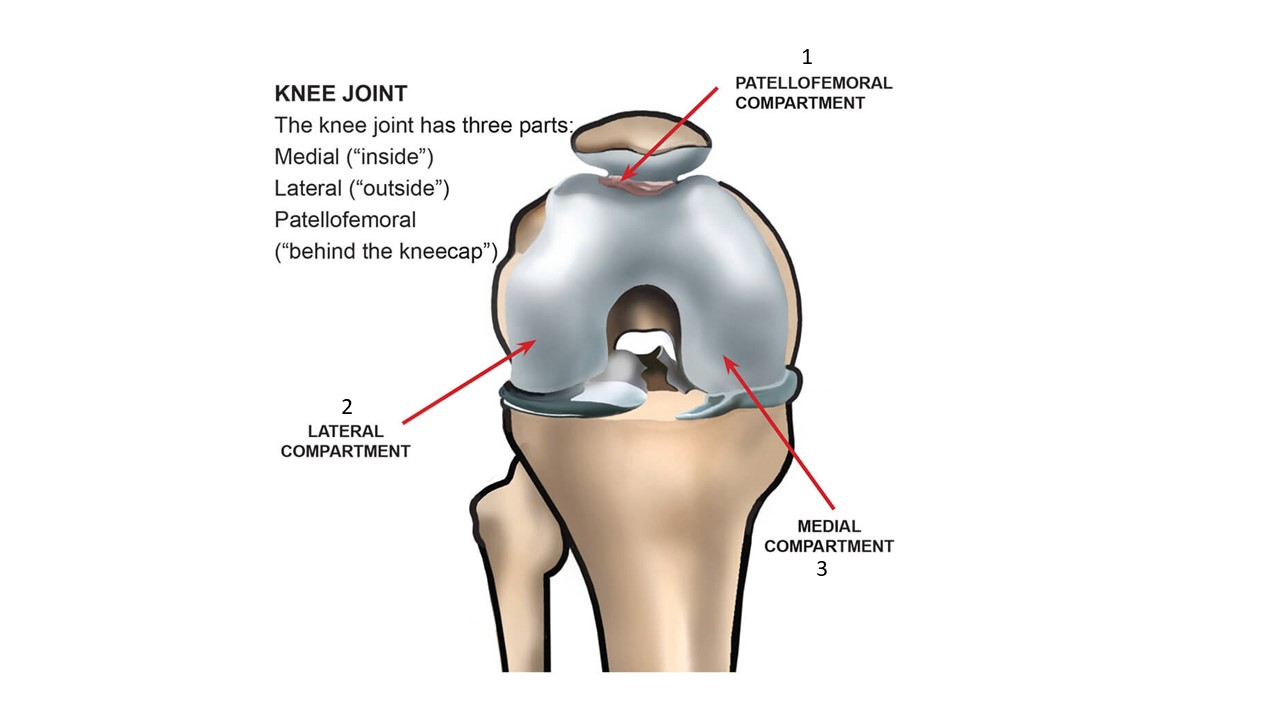
Your knee has 3 points of contact or compartments that house the cartilage of your knee:
- Patella Femoral Compartment
- Lateral (outside) Compartment
- Medial (Inside) Compartment
These compartments are held together by a network of ligaments that hold each bone together and allow the knee to move properly.
Four Principle Knee Ligaments
There are four principal ligaments (2):
- Anterior Cruciate Ligament (ACL),
- Posterior Cruciate Ligament (PCL),
- Medial (inside) Collateral Ligament (MCL), and
- Lateral (outside) Collateral Ligament (LCL).
The collateral ligaments provide stability (3). You can think of these ligaments as the glue that holds the knee together or even the lug nuts that keep your knee together! The 2 most commonly torn ligaments of these are the MCL and ACL (4).
The most important of these ligaments is your ACL. In addition to providing stability to the joint, your ACL acts as a ‘proprioceptive organ” (4). Meaning the ligament has a direct connection to your nervous system via sensory receptors that monitor your knee position. If these sensors sense that the knee is in a bad position, it will activate your nervous system to contract the muscle around the knee to protect the knee as a protective reflex.
Knee ligament surgery is often recommended for the following conditions:
ACL Tears
The Anterior Cruciate Ligament (ACL) is one of four major ligaments in the knee. It is an important stabilizer of the knee and prevents the shin bone (tibia) from sliding in front of the thigh bone (femur). The ACL is susceptible to injury. It is most likely to be injured during activity or by impact. A torn ACL is a common injury for athletes at all levels, but it is most common for people who are active or who experience impact injuries to the knee. ACL injuries can happen to anyone of any age, condition, or ability, and it can be injured in many ways. Examples include abruptly changing direction, slowing down while running, landing incorrectly, or getting struck by someone or some object.
Read More About ACL TearsLCL Sprain
What is an LCL Sprain? A strain or tear to the lateral collateral ligament (LCL) is known as an LCL injury. The LCL is a band of tissue that runs along the outer side of your knee. It aids in keeping the bones together while you walk, ensuring that your knee joint remains stable. How you feel and what type of treatment you’ll require depends on how severely your LCL has been stretched or torn. If it’s only a minor sprain, self-care at home might help. However, if it’s a significant tear or sprain, you may need physical therapy, an injection-based procedure, or surgery….
Read More About LCL SprainLCL Tear
A strain or tear to the lateral collateral ligament (LCL) is known as an LCL injury. The LCL is a band of tissue that runs along the outer side of your knee. It aids in keeping the bones together while you walk, ensuring that your knee joint remains stable. How you feel and what type of treatment you’ll require depends on how severely your LCL has been stretched or torn. If it’s only a minor sprain, self-care at home might help. However, if it’s a significant tear, you may need physical therapy, an injection-based procedure, or surgery. Orthopedists categorize LCL tears into 3 grades…
Read More About LCL TearMCL Sprain
The medial collateral ligament AKA MCL is a thick, strong band of connective tissue on the inside portion of your knee. It connects the top part of the tibia (shin) to the bottom part of the femur (thigh). This is a vital ligament that works along the lateral collateral ligament (LCL), anterior cruciate ligament (ACL), and posterior cruciate ligament (PCL) to bring stability, structure, and movement to the knee. The MCL provides support and stability for the inside (medial) aspect of the knee. MCL sprains are a common injury in sports such as football, hockey, and skiing. The ligament can…
Read More About MCL SprainMCL tear
The medial collateral ligament AKA MCL is a thick, strong band of connective tissue on the inside portion of your knee. It connects the top part of the tibia (shin) to the bottom part of the femur (thigh). This is a vital ligament that works along the lateral collateral ligament (LCL), anterior cruciate ligament (ACL), and posterior cruciate ligament (PCL) to bring stability, structure, and movement to the knee. The MCL provides support and stability for the inside (medial) aspect of the knee. MCL tears are a common injury in sports such as football, hockey, and skiing. The ligament can…
Read More About MCL tearPCL Sprain
The Posterior Cruciate Ligament is one of the paired ligaments in the middle of the knee. It is made up of 2 separate bundles: The two bundles of the PCL, and the ALB (anterior lateral bundle), and the PMB (posterior medial bundle), function synergistically to provide stability. The PCL functions as one of the main stabilizers of the knee joint and serves primarily to resist excessive posterior translation of the tibia relative to the femur. The PCL also acts as a secondary stabilizer of the knee preventing excessive rotation specifically between 90° and 120° of knee flexion. A PCL sprain happens when force is applied beyond…
Read More About PCL SprainPCL Tear
The Posterior Cruciate Ligament (PCL) is a paired ligament in the middle of the knee. It is made up of two separate bundles: ALB (anterior lateral bundle) and PMB (posterior medial bundle). These bundles work synergistically to provide stability. The PCL plays an important stabilizing role in the knee joint by resisting excessive posterior translation of the tibia relative to the femur. Between 90 and 120 degrees of knee flexion, it serves as secondary support for preventing excessive rotation. PCL tears happen when force is applied beyond what the PCL tensile strength is capable of resisting. The tensile strength of the PCL is well documented…
Read More About PCL TearCan a knee ligament heal without surgery?
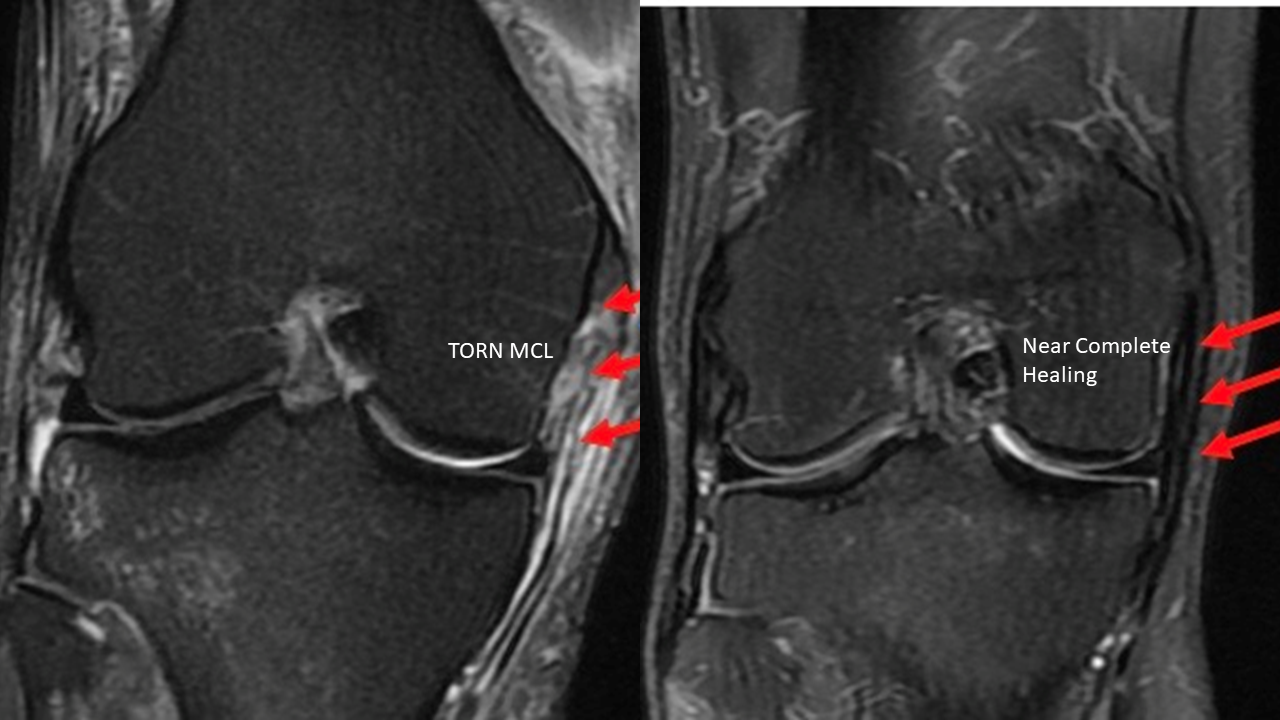
The MCL is the most injured ligament of the knee and the ACL is the most commonly injured ligament in conjunction with the MCL. Most MCL injuries can be treated non-operatively (9). Even though the MCL can spontaneously heal without any additional treatment, the healing that does take place is typically incomplete (11) which can increase the risk of re-injuring the ligament over time.
A precise concentration of bone marrow concentrate can be a better alternative to waiting for the body’s natural healing response to kick in. You can see in before and after treatment that there is near complete healing of the MCL.
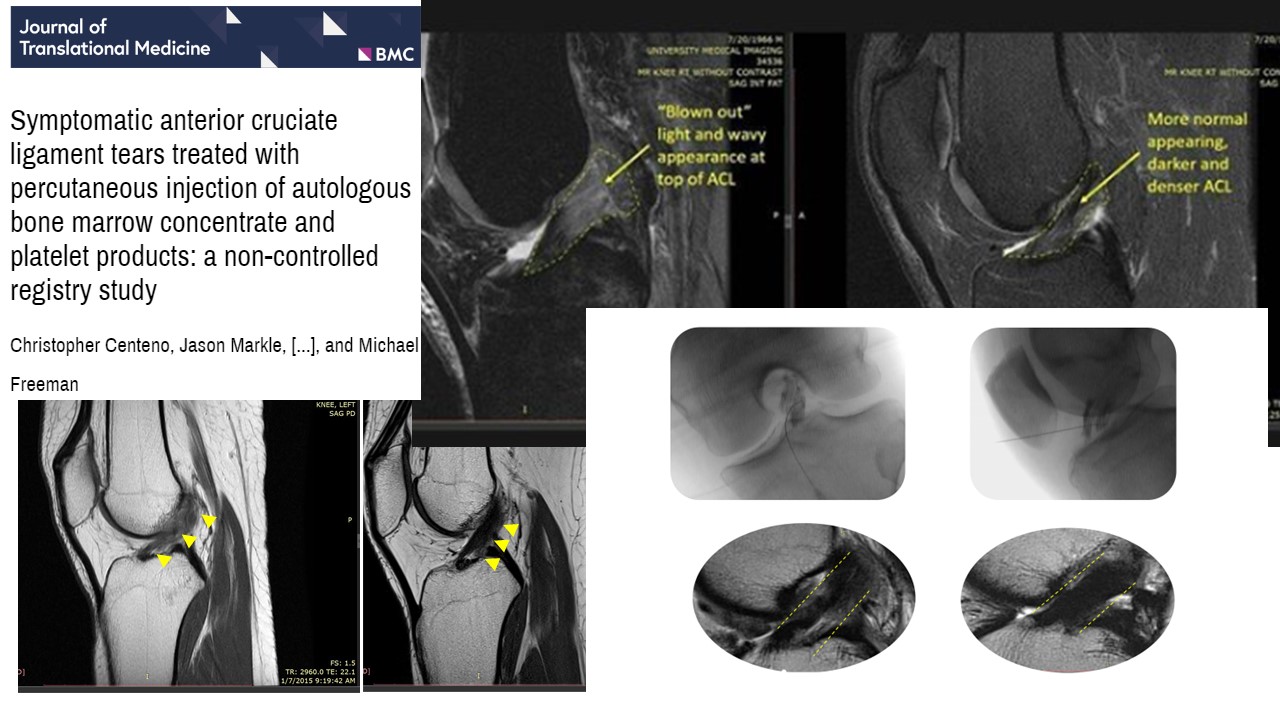
ACL reconstruction has become a standard of care for most ACL tears because the spontaneous healing rate of ACLs is less than 5% (10). But at The Centeno-Schultz Clinic we have created a novel treatment for ACL tears to prevent the need for a knee ligament surgery! Utilizing your own body’s bone marrow concentrate containing stem cells, we can harvest and concentrate the cells, then precisely inject them into the injured ligament. This injection of your own healing cells allows your body to regenerate the ligament and effectively preventing the need for knee ligament surgery! We have published multiple peer reviewed research papers demonstrating 7 to 8 out of 10 patients with an ACL tear can avoid the need for knee ligament surgery!
How long is recovery from knee ligament surgery
The main knee ligament surgery that is the most heavily researched is ACL reconstruction (5). Rehabilitation after reconstruction is key but the rehab course is extensive, taking 9-12 months to complete (5-8)! Postoperative rehabilitation should continue for 9-12 months. During the rehabilitation, there are notable complications and side effects that present. Re-injuries reduced strength in both quadriceps and hamstrings. Loss of proprioception and up to a quarter (1 out of 4) will lose range of motion in both flexion and extension.
Comparing the recovery from the invasive surgery, our novel treatment has seen rehabilitation and return to activity reduced by 50%!
Is ACL surgery a major surgery
While most patients do well in the short term with ACL reconstruction surgery, many orthopedic surgeons fail to discuss the long-term consequences of having knee ligament surgery.
- 60% of patients will develop meniscal damage
- Loss of proprioception
- Loss of knee range of motion 23% of the time
- Quadriceps atrophy in a third of patients
- Hamstring weakness
- Chronic front of the knee pain in 50% of patient who have patella tendon graft
The worst is that within 15 years from surgery you will develop progressive knee arthritis and eventually be a candidate for a knee replacement
Here is the latest video on the current treatment options for ACL tears:
Can you still walk with a torn ligament in your knee?
Yes, you can still walk with a torn ligament but without one (or even two) of your main knee ligaments, walking and simple activities can become difficult. This highlights the need for a good physical therapist that can help you activate the muscles around the knee to allow a more functional knee! Therapy is critical to help reduce the atrophy and help motor control. There are some individuals that are able to continue without the need of a knee ligament surgery or a PRP or bone marrow concentrate procedure where they can return to athletic activity, adapting without the ligament. We refer to these patients as “copers” (12). These are patients that can return to activity after a progressive rehabilitation with a physical therapist without pain or instability BUT research on biomechanics continues to show alterations in the normal mechanics of the knee. Meaning that these patients are still at risk for additional complications such as Meniscal tears and post-traumatic arthritis!
THE UPSIDE
Knee ligament surgeries are not simple and have long-term consequences. We have created treatment options for the majority of ACL and MCL tears to help our patients recover faster and get back to doing what they love sooner without the consequences of more invasive knee ligament surgeries! If you have had a knee ligament injury or other injury and would like to be evaluated, please contact the link below and our staff will be happy to get you set up to see if are a candidate for treatment.
References:
- Failla MJ, Arundale AJ, Logerstedt DS, Snyder-Mackler L. Controversies in knee rehabilitation: anterior cruciate ligament injury. Clin Sports Med. 2015;34(2):301‐ doi:10.1016/j.csm.2014.12.008
- Flandry F, Hommel G. Normal anatomy and biomechanics of the knee. Sports Med Arthrosc Rev. 2011;19(2):82‐92. doi:10.1097/JSA.0b013e318210c0aa
- Kazemi M, Dabiri Y, Li LP. Recent advances in computational mechanics of the human knee joint. Comput Math Methods Med. 2013;2013:718423. doi:10.1155/2013/718423
- Hopf T, Gleitz M, Hess T, Mielke U, Müller B. Propriozeptives Defizit nach Kreuzbandschädigung–afferente Störung oder kompensatorischer Mechanismus? [Proprioceptive deficit following cruciate lesions–afferent disorder or compensatory mechanism?]. Z Orthop Ihre Grenzgeb. 1995;133(4):347‐351. doi:10.1055/s-2008-1039806
- Yabroudi MA, Irrgang JJ. Rehabilitation and return to play after anatomic anterior cruciate ligament reconstruction. Clin Sports Med. 2013;32(1):165‐175. doi:10.1016/j.csm.2012.08.016
- Zult T, Gokeler A, van Raay JJAM, et al. Cross-education does not accelerate the rehabilitation of neuromuscular functions after ACL reconstruction: a randomized controlled clinical trial. Eur J Appl Physiol. 2018;118(8):1609‐1623. doi:10.1007/s00421-018-3892-1
- van Melick N, van Cingel RE, Brooijmans F, et al. Evidence-based clinical practice update: practice guidelines for anterior cruciate ligament rehabilitation based on a systematic review and multidisciplinary consensus. Br J Sports Med. 2016;50(24):1506‐1515. doi:10.1136/bjsports-2015-095898
- Thoma LM, Grindem H, Logerstedt D, et al. Coper Classification Early After Anterior Cruciate Ligament Rupture Changes With Progressive Neuromuscular and Strength Training and Is Associated With 2-Year Success: The Delaware-Oslo ACL Cohort Study. Am J Sports Med. 2019;47(4):807‐814. doi:10.1177/0363546519825500
- Shelbourne KD, Wilckens JH, Mollabashy A, DeCarlo M. Arthrofibrosis in acute anterior cruciate ligament reconstruction. The effect of timing of reconstruction and rehabilitation. Am J Sports Med. 1991;19(4):332‐336. doi:10.1177/036354659101900402
- Razi M, Soufali AP, Ziabari EZ, Dadgostar H, Askari A, Arasteh P. Treatment of Concomitant ACL and MCL Injuries: Spontaneous Healing of Complete ACL and MCL Tears [published online ahead of print, 2020 Apr 8]. J Knee Surg. 2020;10.1055/s-0040-1708858. doi:10.1055/s-0040-1708858
- Wan C, Hao Z, Wen S. The effect of healing in the medial collateral ligament of human knee joint: A three-dimensional finite element analysis. Proc Inst Mech Eng H. 2016;230(9):867‐875. doi:10.1177/0954411916656662
- Iliopoulos E, Galanis N, Iosifidis M, et al. Anterior cruciate ligament deficiency reduces walking economy in “copers” and “non-copers”. Knee Surg Sports Traumatol Arthrosc. 2017;25(5):1403‐1411. doi:10.1007/s00167-015-3709-2
Am I a Candidate?
To answer this question, fill out the candidate form below to request a new patient evaluation, and a patient advocate will reach out to you to determine your next steps. Your one-hour, in-office or telemedicine evaluation will be with one of the world’s experts in the field of Interventional Orthopedics.