Many patients avoid shoulder replacement because they are concerned about shoulder replacement recovery. So what should you expect? How long does it take to recover from a shoulder replacement? Is shoulder replacement surgery successful? Let’s dig in.
What is Shoulder Replacement Surgery?
Shoulder replacement surgery, also known as shoulder arthroplasty, can be a transformative procedure for individuals suffering from severe shoulder pain and reduced mobility due to conditions like osteoarthritis, rheumatoid arthritis, or significant trauma.
While this surgery offers the promise of improved quality of life, patients often have legitimate concerns and uncertainties regarding the process of recovery. Understanding what to expect during the shoulder replacement recovery journey is crucial for both patients and their caregivers.
Shoulder replacement surgery is often recommended by doctors and surgeons for several compelling reasons, primarily when conservative treatments have proven ineffective in alleviating severe shoulder pain and dysfunction.
Conditions Treated by Shoulder Replacement Surgery
Shoulder arthroplasty is recommended to treat various conditions that cause significant pain, reduced mobility, and functional limitations in the shoulder joint. Here are some of the key conditions treated by shoulder replacement surgery:
- Osteoarthritis: Osteoarthritis is a degenerative joint disease that can affect the shoulder over time. It leads to the breakdown of the cartilage and causes pain, stiffness, and reduced range of motion in the shoulder joint. Shoulder replacement can be an effective way of alleviating the pain and restoring function in cases of advanced osteoarthritis.
- Rotator cuff tear arthropathy: Rotator cuff tear arthropathy is a condition characterized by a massive rotator cuff tear, leading to the deterioration of the shoulder joint. It can result in severe pain and limited shoulder function. Shoulder replacement may be recommended to provide stability and relieve pain in these cases.
- Avascular necrosis: Avascular necrosis, also known as osteonecrosis, is a condition in which the blood supply to the bone in the shoulder joint is disrupted, leading to bone death and subsequent joint damage. Shoulder replacement can be considered when conservative treatments fail to address the pain and loss of function associated with avascular necrosis.
- Rheumatoid arthritis: Rheumatoid arthritis is an autoimmune disease that can cause chronic inflammation and damage to the shoulder joint. Shoulder replacement can help relieve pain, improve mobility, and restore function in individuals with advanced rheumatoid arthritis.
- Post-traumatic arthritis: Traumatic injuries such as severe fractures or dislocations can result in post-traumatic arthritis. In cases where conservative treatments are inadequate, shoulder replacement surgery can be a valuable option to reduce pain and enhance shoulder function.
- Failed previous surgeries: In some cases, individuals who have undergone prior shoulder surgeries that were unsuccessful or led to complications may benefit from shoulder replacement to address ongoing pain and functional limitations.
How Does One Become a Candidate for Shoulder Replacement Surgery?
Here are some of the key factors that make an individual a candidate for this procedure:
- Severe pain: Candidates for shoulder replacement typically experience severe and persistent pain in the shoulder joint that significantly interferes with their everyday activities, such as reaching, lifting, and dressing, and may even affect their ability to sleep. The pain is often not adequately managed with pain relievers, and it substantially impairs the individual’s quality of life.
- Loss of motion: Reduced range of motion in the shoulder joint is a common indicator for surgery. Candidates may have difficulty raising their arms, rotating the shoulder, or performing basic movements due to joint stiffness and pain.
- Failed conservative treatments: Before considering surgery, candidates are often required to have attempted and exhausted non-surgical treatments, such as physical therapy, medications, corticosteroid injections, and lifestyle modifications. A lack of improvement or relief from these conservative treatments may make surgery a more viable option.
- Ineffectual prior surgeries: Some candidates may have previously undergone shoulder surgeries (e.g. rotator cuff repair) that were unsuccessful in relieving their symptoms or resulted in complications. In such cases, revision or replacement surgery may be considered.
- Overall health and lifestyle factors: The candidate’s overall health and lifestyle factors, such as age, general fitness, and the ability to participate in postoperative rehabilitation, are also taken into account. Patients should be in reasonable health to undergo the surgery and commit to the recovery process.
Diagnostic Procedures Prior to Surgery
Prior to shoulder replacement surgery, various diagnostic procedures and assessments are conducted to evaluate the extent of shoulder joint damage and ensure the procedure is appropriate for the patient. These diagnostic measures help the medical team plan the surgery and optimize the patient’s outcome.
In addition to a physical exam and X-ray, several other diagnostic procedures may be utilized, including:
- MRI (magnetic resonance imaging): MRI scans provide detailed images of the soft tissues within the shoulder joint, such as ligaments, tendons, and muscles. They are beneficial for assessing rotator cuff tears and other soft tissue injuries that may impact surgical planning.
- CT scan (computerized tomography): A CT scan can provide detailed cross-sectional images of the shoulder joint. It is often used to assess bone quality, especially when bone loss or deformities are suspected.
- Ultrasound: Ultrasound imaging can evaluate soft tissue structures within the shoulder joint, particularly the tendons and other dynamic components. It can identify rotator cuff tears.
- Arthrography: Arthrography involves injecting a contrast dye into the shoulder joint to enhance X-ray images. This procedure can help detect abnormalities in the joint, including labral tears and other structural issues.
- Bone scans: Bone scans use a radioactive tracer to identify areas of increased bone activity, which can indicate specific conditions such as infection or avascular necrosis.
- Blood tests: In some cases, blood tests may be performed to rule out or identify underlying systemic conditions like rheumatoid arthritis, which may be contributing to shoulder joint problems.
- Electromyography (EMG) and nerve conduction studies: These tests assess the electrical activity of the muscles and nerves in the shoulder and upper extremities. They can help diagnose nerve-related issues and guide surgical planning.
- Functional assessments: Depending on the patient’s symptoms and physical limitations, functional assessments and range of motion tests may be conducted to evaluate the extent of disability and guide surgical decision-making.
Types of Shoulder Replacement Surgeries
There are different types of shoulder replacement surgeries, which are explained in detail below:
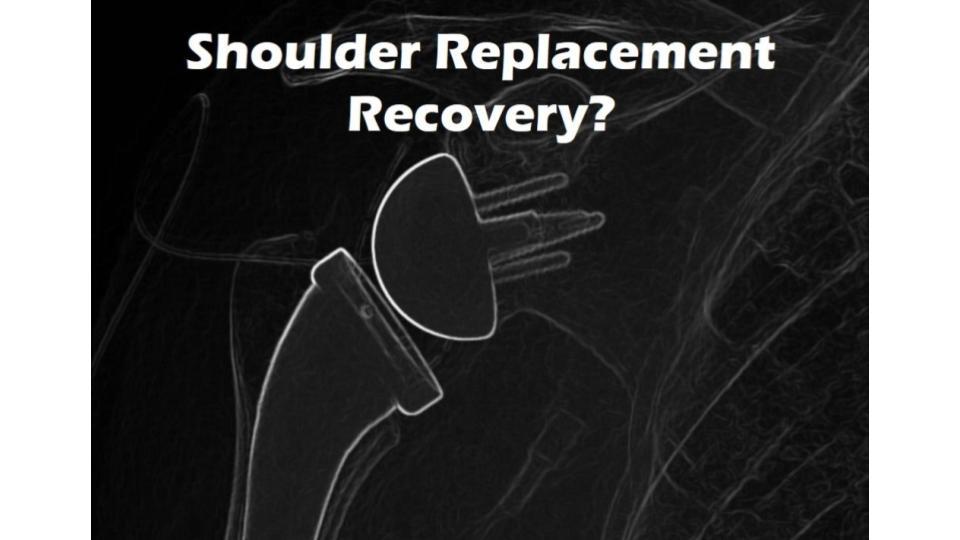
Total Shoulder Replacement (aka Total Shoulder Arthroplasty)
The whole shoulder joint is removed and then an anatomically similar ball and socket joint is installed. The surgeon removes the arthritic or damaged humeral head (the “ball” of the shoulder joint) and the glenoid (the “socket” of the shoulder joint). An artificial ball and socket joint, made of metal and plastic components, is implanted.
The metal ball is attached to the upper arm bone (humerus), and the plastic socket is secured in the shoulder blade (scapula). Total shoulder replacement is recommended for individuals with conditions like severe osteoarthritis, rheumatoid arthritis, or post-traumatic arthritis, where both the ball and socket components of the shoulder joint are significantly affected.
Reverse Shoulder Replacement
The whole shoulder joint is removed and a reverse configuration device is installed where a ball is placed where the socket used to be and a socket is placed where the ball used to be. Reverse shoulder replacement is a specialized type of shoulder replacement surgery designed for specific conditions, including massive rotator cuff tears or severe shoulder joint damage.
The procedure involves reversing the orientation of the ball and socket components in the shoulder joint.
Partial Shoulder Replacement (Hemiarthroplasty)
This involves replacing the arthritic humerus (the ball) while retaining the patient’s own shoulder socket. The damaged humeral head is removed, and an artificial ball component is implanted. Partial shoulder replacement is typically recommended for individuals who have a severely damaged humeral head but have an intact and functioning glenoid (shoulder socket).
This procedure is commonly used in cases of proximal humerus fractures or severe humeral head osteonecrosis.
How Dangerous Is a Shoulder Replacement?
Every surgery comes with risks. A shoulder replacement surgery is no different. However, the risks are not life-threatening. There are a few things to be aware of when undergoing this procedure, like complications. A longer shoulder replacement recovery will be needed if you happen to have a complication from the procedure. About 4% of shoulder replacement patients get an infection that will need to be treated with at least six weeks of IV antibiotics and possible additional surgery.
In fact, taking out the infected shoulder device and cutting out the infected tissue may be the most effective treatment in addition to antibiotics. Loosening of the implanted shoulder device (due to its failure to bond to the bone) happens in about 6% of cases. Nerve injury occurs in 1-4% of shoulder replacement patients.
What Is the Typical Shoulder Replacement Surgery Success Rate?
With all of this prolonged shoulder replacement recovery, it’s startling to consider that one study from 2015 showed that 22% of patients still had significant shoulder pain one to two years after shoulder replacement surgery. In fact, in that same study, 38% of patients still had pain that they rated as 4/10 or greater, and 10% of patients still had severe pain that they rated as 8-10.
That means that only six in 10 patients had mild pain or no pain after their shoulder replacement surgery. In a 2019 study, only 20% of patients had pain that was considered moderate or greater. Also concerning is a large UK study that showed that about one in four men aged 55-59 years needed a reoperation within five years. Finally, others have found that in the long term, in younger patients, many devices are failing.
For example, in one US study about four in 10 patients who were under 55 years of age had a failure of their shoulder device after 10 years.
Recovery Time for Shoulder Replacement
Shoulder replacement recovery typically begins in the hospital with a stay of about two or three days. A cryocuff icing device or ice packs are used immediately after the surgery and at home to help reduce swelling. The arm will be in a sling for four to six weeks after surgery, and during that time the patient needs to make sure their sleep position doesn’t permit the arm to go backward.
A gentle shoulder range of motion exercise program is usually started immediately. Physical therapy usually begins at two or three weeks post-surgery. Resumption of full shoulder range of motion and driving typically begins at around six weeks.
How Should I Plan for Recovery?
Planning for recovery after shoulder replacement surgery is essential to ensure a smooth and successful rehabilitation process. Anticipating and addressing limitations in motion are crucial for a safe and comfortable recovery. Here are some key points to consider and plan for:
- Place items within easy reach: Arrange your home environment to make daily essentials easily accessible. Store commonly used items like dishes, utensils, toiletries, and medications at waist or chest level so you don’t have to reach or stretch your affected arm.
- Wear clothing that’s easy to put on and take off: Prior to surgery, invest in or prepare a wardrobe of clothing that opens in the front (e.g. button-up shirts or zippered jackets) to avoid raising your arms above shoulder level. Slip-on shoes can also be convenient.
- Ask for help from someone you trust: It’s important to have a support system in place. Contact a trusted friend or family member who can assist you with daily tasks and provide emotional support during your recovery. They can help with activities like cooking, cleaning, and transportation.
What Should I Avoid after Shoulder Replacement Surgery?
After shoulder replacement surgery, it’s crucial to avoid certain activities and behaviors to promote healing and prevent complications. Here are specific limitations you should adhere to:
- Avoid lifting anything heavier than a glass of water for the first one to four weeks. In the initial weeks after surgery, avoid lifting any objects that weigh more than a glass of water (typically about 1-2 pounds). This precaution is crucial to prevent stress on the healing shoulder joint.
- Avoid lifting heavy objects for two months. Even after the initial phase, it’s essential to refrain from lifting heavy objects for an extended period (usually up to two months or as advised by your surgeon). This restriction is to protect the newly implanted joint and promote proper healing.
- Avoid using the operative arm to push yourself from your bed or chair. Avoid using your surgical arm to push yourself up from a bed, chair, or any surface for at least the first few weeks. Instead, rely on your non-operative arm and leg to reduce strain on the operated shoulder.
- Refrain from sports. For an extended period, refrain from participating in sports or activities that involve strenuous arm movements, heavy lifting, or significant physical contact. Consult with your surgeon to determine when it’s safe to resume such activities.
- Avoid extreme positions for the arm. Avoid putting your arm in extreme positions, especially those that involve overstretching, hyperextension, or extreme overhead movements. Follow your surgeon’s recommendations for safe ranges of motion during your recovery.
- Avoid excessive weight-bearing activities. Activities that put excessive weight on the shoulder, such as push-ups, pull-ups, or heavy resistance training, should be avoided during the early recovery period.
- Steer clear of high-impact activities. Steer clear of high-impact activities that could jar the shoulder, including running, jumping, or activities that may lead to falls.
- Don’t drive. Driving may be restricted for a period post-surgery. Consult with your surgeon regarding when it’s safe to resume driving.
- Minimize repetitive or prolonged arm movements. Prolonged or repetitive arm movements, especially when they involve lifting, should be minimized during the early stages of recovery.
How Soon Can I Come Back to Work?
For shoulder replacement recovery, expect to take a couple of weeks off work. In a 2020 study, 92% of patients were back to work within two months, but only about two-thirds of those patients returned to heavy work. If your job involves using your arms, then time off work will be longer.
It is important to note that for the long term, only about 5% of patients were still using narcotics one year after their shoulder replacement.
Will My Shoulder Rotator Cuff Muscles Work Normally?
The rotator cuff muscles move the shoulder joint and stabilize it. If you replace the joint and remove the bones, then these critical muscles can be damaged. Often, these muscles are also torn and frayed in shoulder arthritis patients who have shoulder replacement, so there is a debate as to whether the surgeon should also repair these muscles.
Other studies have found that the shoulder is weaker in internal and external rotation following replacement, again due to the fact that the rotator cuff muscles often can’t be preserved.
Non-Surgical Shoulder Treatments to Avoid Replacement
We have helped many patients avoid shoulder replacement recovery by using the PSA (percutaneous shoulder arthroplasty) procedure. This involves using the patient’s own concentrated bone marrow stem cells injected into the damaged rotator cuff, ligaments, bone, and joint.
The success rate is usually about 80% in the right patients. This procedure has a much quicker recovery time, without many of the same serious complications that accompany shoulder replacement. The rotator cuff muscles are preserved, so often these patients can keep their own anatomy.
Make a Wise Choice When It Comes to Shoulder Pain
In conclusion, shoulder replacement surgery can be a highly effective solution for relieving debilitating shoulder pain and improving joint function in many cases. However, it’s essential to recognize that it may not be the only option, and patients should carefully consider alternatives before committing to a treatment plan.
Not all conditions necessitate surgery, and certain issues like tendonitis, bursitis, or mild osteoarthritis may respond well to non-surgical treatments, including physical therapy, anti-inflammatory medications, and regenerative medicine procedures.
Regenerative medicine techniques, such as platelet-rich plasma (PRP) and stem cell therapy, offer non-surgical options for managing shoulder pain. These procedures aim to stimulate the body’s natural healing processes and can be effective for certain conditions.
Shoulder replacement is a big surgery. Regrettably, based on the research, about 20-40% of patients’ shoulder pain will still be moderate or greater, despite the surgery. Recovery times are long, and complication rates are similar to other large joint replacements.
Consider the alternatives to shoulder replacement surgery. Make an appointment today!