Sit Bone Pain / Ischial Tuberosity
Get Help With Sit Bone Pain / Ischial TuberosityLife can sometimes be a pain in the butt. Truly! What happens, however, when you actually have debilitating pain in the butt? What are your but bones – often called “sit bones” or simply butt bones – comprised of? And why do people call it Sitz bone?
What are the causes of sit bones pain? What are the treatment options? How do you know how to relieve sit bone pain? Let’s dig in.
What Are Your Sit Bones?
What Causes Pain in the Sit Bones?
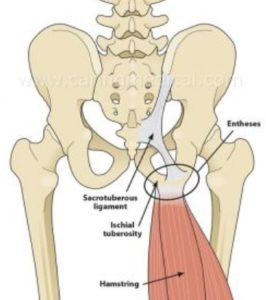
Sit bone pain can be caused by irritation or injury to the local structures or can be referred from other structures. Inflammation of the hamstring or adductor tendon can cause a tendonitis or if long-term tendinosis can cause pain in your sit bones (1). A bursa is a fluid-filled structure that allows tendons and muscles to slide freely. Irritation or inflammation of the ischial bursae can cause sit bone pain (2). The bone itself is also vulnerable to injury and fracture of the ischial tuberosity can cause significant sit bone pain (3).
Referred pain is important and must be evaluated. Common sources include:
- Sacroiliac Joint: Formed by the ilium and the sacrum bones, this joint is susceptible to injury. 94% of patients with documented SI joint injury have pain in the buttock (4).
- Sciatic nerve irritation: The largest and longest nerve in the body, the irritation of the sciatic nerve can result in buttock pain.
- Piriformis and glutenous maximums muscle dysfunction: Common referral patterns include pain in the lower buttock (5).
- Lumbar disc injury with nerve irritation: Disc bulges, disc herniation, facet joint overgrowth and narrowing of the bony doorway through which nerves exit can cause nerve irritation with resultant pain in the sit bone.
Gluteal Tendinopathy
Tendinopathy is a group of tendon disorders. The most common form of Tendinopathy is Tendinosis (1). Tendinosis is a degenerative condition that is characterized by collagen degeneration and micro-trauma in the tendon due to repetitive overloading. Gluteal Tendinopathy is a clinical condition in which there is moderate to severe debilitating pain due to injury of the Gluteal tendons. It is the most common Tendinopathy in the lower leg (2) and is more common in women (3). In most cases, physical examination alone is sufficient to diagnose Gluteal Tendinopathy. If symptoms continue despite conservative care, other studies may be warranted which include ultrasound and MRI.
Read More About Gluteal TendinopathyPinched Nerves in the Back
We talk a lot about leg pain stemming from a pinched or irritated nerve in the lower back. And, indeed, that’s what our physicians are traditionally taught in medical school—a pinched nerve in the lumbar spine typically presents as a symptom in the leg. However, what if you have some butt pain but no pain or other symptoms in the leg? Does this mean it couldn’t be a pinched nerve? Not so fast. Turns out a pinched low back nerve doesn’t always have to be accompanied by leg symptoms. Let’s start by taking a look at how the back is structured.
Read More About Pinched Nerves in the BackSciatica
Disc herniation, disc protrusion, overgrowth of the facet joint, and thickening of the ligaments can result in nerve root compression or irritation, causing symptoms of sciatic compression. Some causes of sciatic compression can be interrelated with the following conditions: Degenerative disc disease, Spinal stenosis, damage or injuries to the discs, spondylolisthesis, piriformis syndrome, osteoarthritis. The symptoms of sciatica include pain in the lower back, buttock, and down your leg, numbness and weakness in low back, buttock, leg, and/or feet, pain increase with movement, “Pins and needles” feeling in your legs, toes, or feet., loss of bowel control, and incontinence. Sciatica can be treated…
Read More About SciaticaSI Joint Syndrome
The sacroiliac joints reside between the sacrum (the tailbone segment of the spinal column) and the prominent wing-like iliac bones that form the pelvic girdle. There are two SI joints, one on the left and one on the right (highlighted in red in the image above), and along with the symphysis pubis joint at the front of the structure, they are critical for transferring forces and energy back and forth between the spine and the lower limbs. There are a number of reasons that an SI joint can become painful and inflamed, leading to SI joint syndrome. Trauma, such as a fall injury to the tail bone or a forced injury from a car accident for example, obviously can create problems in the SI joint…
Read More About SI Joint SyndromeTo learn more about the top three causes of butt pain please click on video below.
How do you Treat Sitz Bone Pain?
Appropriate treatment will depend upon the actual source of the pain. Activity modification, rest, healthy anti-inflammatory medications such as fish oil and curcumin can reduce the pain. Physical therapy and intra-muscular stimulation (IMS) can reduce the pain associated with ischial bursa and hamstring tendon inflammation. Steroid injections, while common, are quite toxic as they can compromise the tendons, muscles, and ligaments. Steroids have been demonstrated to deplete the number of stem cells and weaken tendons (6). PRP is an effective treatment option as it allows the growth factors associated with PRP to reduce inflammation, increase blood flow and promote healing. PRP has also been effective in the treatment of ischial tuberosity fractures (7).
Physical therapy can be effective in the management and treatment of sacroiliac joint injury and pain. When conservative therapy fails, x-ray guided injections of PRP into both the joint itself and supporting ligaments are effective.
The low back is often overlooked and missed as a source of referred butt pain. This is what happened to me in 2003 as I developed unrelenting right buttock pain. Everyone was focused on local structures such as adductor or hamstring tendons, and piriformis when in fact I had a large lumbar disc herniation. I had no leg pain and minimal back pain. Epidural steroid injections were recommended which I declined. Why?
Epidural steroid injections should be avoided as they are associated with a number of side effects which include increased risk of spinal fracture, suppression of the stress response, elevations in blood sugar, and compromise of the local muscles, tendons, and ligaments. PRP is an effective alternative to steroids (8). At the Centeno-Schultz Clinic, we have extensive experience in the treatment of sit bones pain with an x-ray guided and ultrasound-guided PRP injections.
To learn more about treatment options for disc injuries please click on the video below.
In Conclusion..
The ischial tuberosities, aka the butt bones, are paired bones in the pelvis that serve as important attachments for muscle and tendons. Sit bone pain can arise from injury or irritation of local structures which include the bursae, tendons, and ligaments. Sit bone pain can also be referred from other sources which include muscles, the sacroiliac joint, and low back injuries with nerve irritation. Physical therapy and activity modification are first-line treatments. Steroids should be avoided due to their significant side effects. PRP is an effective treatment for sit bone pain.
Our Doctors Who Treat Sitz Bone Pain

Christopher J. Centeno, MD
Christopher J. Centeno, M.D. is an international expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate in orthopedics. He is board-certified in physical medicine and rehabilitation with a subspecialty of pain medicine through The American Board of Physical Medicine and Rehabilitation. Dr. Centeno is one of the few physicians in the world with extensive experience in the culture expansion of and clinical use of adult bone marrow concentrate to treat orthopedic injuries. His clinic incorporates a variety of revolutionary pain management techniques to bring its broad patient base relief and results. Dr. Centeno treats patients from all over the US who…
Read more
John Schultz, MD
John R. Schultz M.D. is a national expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate for orthopedic injuries. He is board certified in Anesthesiology and Pain Medicine and underwent fellowship training in both. Dr. Schultz has extensive experience with same day as well as culture expanded bone marrow concentrate and sees patients at the CSC Broomfield, Colorado Clinic, as well the Regenexx Clinic in Grand Cayman. Dr. Schultz emphasis is on the evaluation and treatment of thoracic and cervical disc, facet, nerve, and ligament injuries including the non-surgical treatment of Craniocervical instability (CCI). Dr. Schultz trained at George Washington School of…
Read more
John Pitts, M.D.
Dr. Pitts is originally from Chicago, IL but is a medical graduate of Vanderbilt School of Medicine in Nashville, TN. After Vanderbilt, he completed a residency in Physical Medicine and Rehabilitation (PM&R) at Emory University in Atlanta, GA. The focus of PM&R is the restoration of function and quality of life. In residency, he gained much experience in musculoskeletal medicine, rehabilitation, spine, and sports medicine along with some regenerative medicine. He also gained significant experience in fluoroscopically guided spinal procedures and peripheral injections. However, Dr. Pitts wanted to broaden his skills and treatment options beyond the current typical standards of care.
Read more
Jason Markle, D.O.
Post-residency, Dr. Markle was selected to the Interventional Orthopedic Fellowship program at the Centeno-Schultz Clinic. During his fellowship, he gained significant experience in the new field of Interventional Orthopedics and regenerative medicine, honing his skills in advanced injection techniques into the spine and joints treating patients with autologous, bone marrow concentrate and platelet solutions. Dr. Markle then accepted a full-time attending physician position at the Centeno-Schultz Clinic, where he both treats patients and trains Interventional Orthopedics fellows. Dr. Markle is an active member of the Interventional Orthopedic Foundation and serves as a course instructor, where he trains physicians from around the world.
Read more
Brandon T. Money, D.O., M.S.
Dr. Money is an Indiana native who now proudly calls Colorado home. He attended medical school at Kansas City University and then returned to Indiana to complete a Physical Medicine and Rehabilitation residency program at Indiana University, where he was trained on non-surgical methods to improve health and function as well as rehabilitative care following trauma, stroke, spinal cord injury, brain injury, etc. Dr. Money has been following the ideology behind Centeno-Schultz Clinic and Regenexx since he was in medical school, as he believed there had to be a better way to care for patients than the status quo. The human body has incredible healing capabilities…
Read more_________________________________________________________________________________
1. Bass E. Tendinopathy: why the difference between tendinitis and tendinosis matters. Int J Ther Massage Bodywork. 2012;5(1):14-7.
2. Johnson DB, Varacallo M2. Ischial Bursitis. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019. Mar 19.
3. Spencer-Gardner L, Bedi A, Stuart MJ, Larson CM, Kelly BT, Krych AJ. Ischiofemoral impingement and hamstring dysfunction as a potential pain generator after ischial tuberosity apophyseal fracture non-union/malunion. Knee Surg Sports Traumatol Arthrosc. 2017;25(1):55-61.DOI: 10.1007/s00167-015-3812-4
4. Podschun L, Hanney WJ, Kolber MJ, Garcia A, Rothschild CE. Differential diagnosis of deep gluteal pain in a female runner with pelvic involvement: a case report. Int J Sports Phys Ther. 2013;8(4):462-71.
5. Orchard JW. Intrinsic and extrinsic risk factors for muscle strains in Australian football. Am J Sports Med. 2001;29(3):300-3.
6. Zhang J, Keenan C, Wang JH. The effects of dexamethasone on human patellar tendon stem cells: implications for dexamethasone treatment of tendon injury. J Orthop Res. 2013;31(1):105-10.DOI: 10.1002/jor.22193
7. Stafford CD, Colberg RE, Nourse AL. Chronic ischial tuberosity avulsion nonunion fracture treated with a platelet-rich plasma injection as a bone graft. Regen Med. 2019;14(5):353-8.DOI: 10.2217/rme-2018-0071
7. Slipman CW, Jackson HB, Lipetz JS, Chan KT, Lenrow D, Vresilovic EJ. Sacroiliac joint pain referral zones. Arch Phys Med Rehabil. 2000;81(3):334-8.DOI: 10.1016/s0003-9993(00)90080-7
8. Centeno C, Markle J, Dodson E, et al. The use of lumbar epidural injection of platelet lysate for treatment of radicular pain. J Exp Orthop. 2017;4(1):38. 29177632.DOI: 10.1186/s40634-017-0113-5