Jugular Vein Compression Symptoms Due To The Neck And CCI
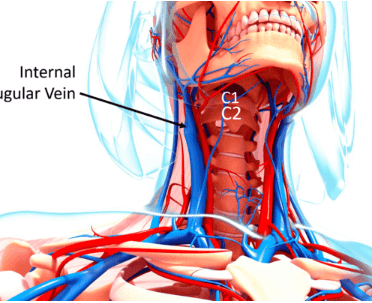
Get Help With Jugular Vein CompressionThe internal jugular vein is a major vein in the neck that carries deoxygenated blood from the head and face back to the heart. Due to its location, it is susceptible to compression from various structures in the neck, including muscles, bones, and ligaments.
One of the main causes of jugular vein compression is thought to be craniocervical instability (CCI), a condition caused by the misalignment of the upper neck bones C1 and C2 that can lead to symptoms such as dizziness, headaches, poor balance, fatigue, tinnitus, and more.
The following is an in-depth examination of jugular vein compression symptoms, how it is caused, and what you can do about it.
What Is The Jugular Vein?
The jugular veins are large veins located in the neck, usually near the carotid artery. There are two jugular veins that return blood from the head and neck back to the heart: the external jugular vein and the internal jugular vein.
The external jugular vein is visible on the surface of the neck and travels from behind the ear down to the base of the neck. The internal jugular vein is largely hidden from view. It runs from the brain through the jugular foramen (a small, natural opening in the skull) down to the subclavian vein, eventually emptying into the heart.
Jugular Vein Compression
Jugular vein compression causes the blood to run back towards the brain. This can cause various symptoms, the most common of which are insomnia and tinnitus as well as head noises, hearing impairment, headache, and neck pain.
Because the jugular vein is long, it can be compressed at any point from where it starts in the brain to its end near the heart. However, we are reviewing compression in the upper neck, where the bones C1 and C2 meet.
For example, if the C2 neck bone rotates, the jugular vein in the C1-C2 region can be compressed when one side of the C2 pivots forward.
Why Would The C2 Joint Rotate?
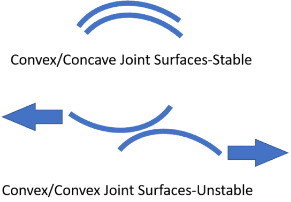
The C2 neck bone could rotate (leading to compression) because the C1-C2 joint is inherently unstable. Whereas most of the body’s joints are inherently stable because of their ball and socket configuration, the C1-C2 joint is different. It has a unique construction and relies on ligaments, joint capsules, and muscles to provide stability instead.
If the ligaments holding the head to the neck are loose, it can cause one joint surface to slide down the other. As a result, the C2 bone can move out of place and rotate on C1, potentially leading to jugular vein compression.
Jugular Vein Compression Due To CCI: A Patient Example
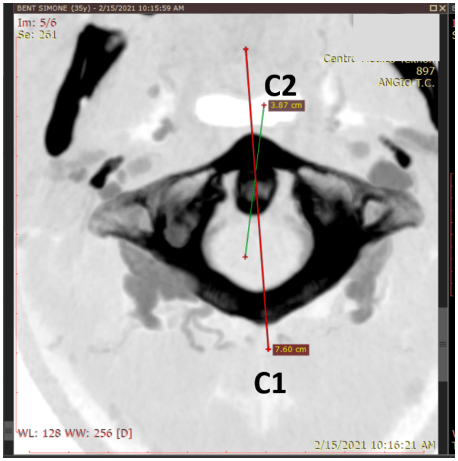
Let’s look at these patient images to better understand how jugular vein compression occurs. The first image is a top-down CT scan of the patient’s C1 bone, which is the black ring-shaped structure. The oval shape inside the front of the C1 bone is the dens of the C2 bone. The two lines drawn across the image marked C1 and C2 represent the front-back angle of each bone.
As you can see, the two lines are misaligned: the C1 line points to the left and the C2 line is turned to the right. This indicates that the bones are rotated against one another.. This is not how they should be positioned, which means that the ligaments holding the head could be too loose.
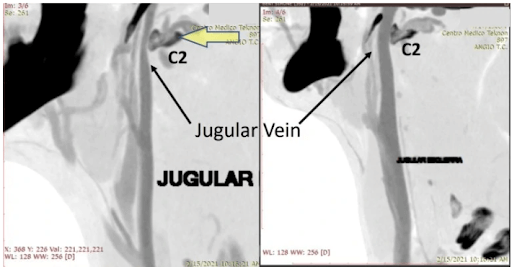
These two images above are are side views of the same patient and show the jugular vein of on this patient’s right and left. The veins are filled with radiographic contrast (which allows it to be seen on a CT scan). As you can see, the dark oblong-shaped structure is marked as C2.
The C2 bone in the left image is rotated forward and is an example of jugular vein compression. As you can see, the vein passing through this bone is much smaller due to the pressure placed on the jugular vein. Compare this to the vein in the image on the right side, which is normal-sized because it’s not being compressed.
Learn about Regenexx procedures for neck conditions.
What Are The Symptoms Of Jugular Vein Compression?
Jugular vein compression can cause a wide range of symptoms. However, because the symptoms of jugular vein compression sometimes overlap with other medical conditions, such as CCI, it is crucial to get a thorough diagnosis from a qualified healthcare professional.
The symptoms below are from a research study on patients who had confirmed jugular vein compression with the largest words being reported more commonly:
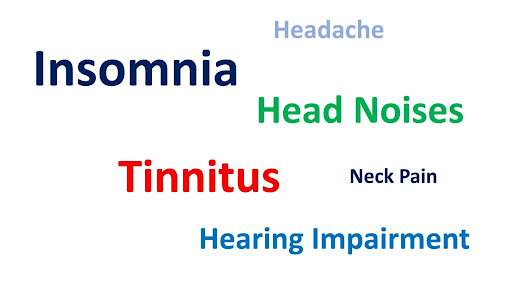
Basically, even if you have jugular vein compression, you may not have CCI, even if you’re exhibiting some of the symptoms of CCI. With that in mind, the following are some of the primary symptoms of jugular vein compression:
Headaches And Ringing In The Ears
Headaches are a common symptom of jugular vein compression, but, as you can see above, are less common than other symptoms. The intensity and location of the headache may vary from person to person, but it is typically located on the forehead, temples, or back of the head.
The decreased intracranial venous return caused by jugular vein compression can lead to increased intracranial pressure, a potential trigger for headaches. Having said that, realize that there are many problems in the neck that refer to the head.
Tinnitus, which is ringing in the ears, is the most common symptom of jugular vein compressionl. It can range from mild to severe and can be accompanied by various other symptoms, such as hearing loss or dizziness. Tinnitus results from increased intracranial pressure in the veins near the ear, leading to hearing changes.
Blurry Or Double Vision
Blurry or double vision can occur due to increased pressure in the veins near the eyes, but these symptoms are much less common. This pressure can cause swelling of the optic nerve, leading to vision changes. Other symptoms, such as eye pain, fatigue, and headaches, may accompany blurry or double vision.
Insomnia
Insomnia is a common problem that patients with internal jugular vein compression report and can manifest as difficulty falling asleep, difficulty staying asleep, or waking up too early. As a result of this lack of sleep, insomnia can lead to fatigue, concentration difficulties, and irritability.
Compression of the jugular vein could block the cerebrospinal fluid (which is responsible for regulating sleep cycles) from returning to the brain and cause increased intracranial pressure that can lead to decreased melatonin and circadian dysrhythmias.
Transient Amnesia
Transient amnesia is a sudden and temporary inability to remember newly learned information. This can manifest as difficulty recalling recently acquired memories, such as names and events.
Although the cause isn’t known, research has shown that it is associated with a prevalence of internal jugular valve insufficiency, which means there’s a potential that it could be triggered by jugular vein compression.
Eagle’s Syndrome And Jugular Vein Compression
Many of the symptoms caused by jugular vein compression are also caused by Eagle’s Syndrome. Eagle’s Syndrome occurs when the ligaments that extend down from the styloid process (a small bony projection extending from the base of the skull) become calcified, which can compress the internal jugular vein.
Diagnosing the underlying cause of the symptoms shared between both conditions can be challenging because many patients diagnosed with Eagle’s Syndrome also have CCI.
Additionally, other bones in the front of the neck, such as the hyoid, can compress the jugular vein. Finally, in many patients with jugular vein compression due to the syloid process and a calified ligament, the CCI causes the compression as decribed above.
How Is This Problem Treated?
Treatment for jugular vein compression depends on the underlying cause and severity. There are several ways that the condition can be treated, including conservative care and surgery. With that in mind, the following are the different ways that jugular vein compression can be treated:
Conservative Care
Conservative care includes rest, avoiding activities that aggravate symptoms, using over-the-counter pain relievers to reduce pain and inflammation, and upper cervical chiropractic treatment (a form of manual manipulation of the neck and upper spine).
However, conservative care is not always effective in relieving symptoms as the underlying cause of the compression must be addressed. As such, the condition generally doesn’t resolve with conservative care.
Additionally, there are inherent risks in relying on pain medications (such as potential side effects). It’s also important to note that most internal jugular vein compression is not symptomatic, hence getting an accurate diagnosis is key.
Decompression for Eagle’s Syndrome
In the case of Eagle’s Syndrome, styloidectomy surgery may be recommended. Styloidectomy is a surgical procedure in which the styloid process is removed or shortened to relieve pressure on the jugular vein. The procedure can be done in several different ways.
In some cases, it can be done through the mouth, although this will require the removal of the tonsils. It’s also much more difficult to reach the styloid process through the mouth.
In other cases, the procedure can be done through an incision in the neck, although this may involve a more extensive recovery period. More recently, endoscopic techniques have been developed that make it possible to perform the procedure without any incisions by using a tube with an attached camera to access the styloid process.
Upper Neck Fusion Surgery
Upper neck fusion surgery is the most invasive treatment option available for jugular vein compression. This surgery involves fusing two or more vertebrae in the neck together to reduce the pressure on the jugular vein. This is typically accomplished by placing screws across the C1-C2 joints, and permanently immobilizing them.
However, upper neck fusion surgery is usually only recommended when other treatments have failed to improve symptoms because of the high complication rates associated with the procedure.
Some complications that may arise from this invasive procedure include nerve damage, infection, dysphagia (difficulty swallowing), and adjacent segment disease (damage to the vertebrae above and below the fused joints). Not to mention, there’s no guarantee of pain relief.
Traditional Prolotherapy
Traditional prolotherapy is a form of injection therapy that involves injecting a solution containing dextrose, saline, and an anesthetic into the ligaments in the back of the neck. The solution is meant to cause inflammation and irritation in the ligaments, tightening those ligaments causing better stability which in turn will reduce the pressure on the jugular vein.
If the instability is due to laxity of the posterior ligaments, then posterior prolotherapy injections could be effective.
Percutaneous Implantation Of The CCJ Ligaments (PICL) Procedure
For many type sof instability, posterior injections can’t reach the interbal ligaments that cause CCI. Hence, the PICL procedure is the most likely to be effective. This non-surgical procedure involves using x-ray guidance to inject a bone marrow concentrate (taken from the patient) into the internal neck’s ligaments to help tighten them.
Tightening the ligaments helps prevent the C1 and C2 bones from rotating against each other, thereby preventing the compression of the jugular vein. The PICL procedure has shown to be much safer than cervical fusion .
Improve Your Quality Of Life. Consult With Us Today.
Jugular vein compression is a serious condition that can cause debilitating pain, fatigue, and dizziness. There are various treatment options available, ranging from conservative care to invasive surgeries. It’s essential to choose well for the best chance at relieving your symptoms while also minimizing the risk of complications.
At Centeno Schultz, we treat our patients with the PICL procedure or posterior injections. We specialize in this cutting-edge procedure and can help you get back to living a healthy, active life. If you are suffering from symptoms of jugular vein compression, don’t hesitate to contact us today and improve the quality of your life.
Want to know more about the PICL procedure?
References:
1.Offiah CE, Day E. The craniocervical junction: embryology, anatomy, biomechanics and imaging in blunt trauma. Insights Imaging. 2017;8(1):29-47. doi:10.1007/s13244-016-0530-5
2.Zdilla MJ, Russell ML, Bliss KN, Mangus KR, Koons AW. The size and shape of the foramen magnum in man. J Craniovertebr Junction Spine. 2017;8(3):205-221. doi:10.4103/jcvjs.JCVJS_62_17
3..Li M, Su C, Fan C, Chan CC, Bai C, Meng R. Internal jugular vein stenosis induced by tortuous internal carotid artery compression: two case reports and literature review. J Int Med Res. 2019;47(8):3926-3933. doi:10.1177/0300060519860678.
4.Zamboni P, Scerrati A, Menegatti E, Galeotti R, Lapparelli M, Traina L, Tessari M, Ciorba A, De Bonis P, Pelucchi S. The eagle jugular syndrome. BMC Neurol. 2019 Dec 21;19(1):333. doi: 10.1186/s12883-019-1572-3. PMID: 31864313; PMCID: PMC6925502.