Brachial Plexus Injury
The brachial plexus involves five nerve roots from C5 to T1. Brachial plexus injuries can vary greatly from mild to severe. They have multiple causes and often occur concurrently with other injuries; that makes their diagnosis complicated.
However, an injury to this plexus of nerves can affect the movement of the entire arm and forearm. Let’s discuss all the details of brachial plexus injury, including its symptoms, diagnosis, and how it’s treated.
What Are Brachial Plexus Injuries?
The brachial plexus is created from five nerves originating from the spinal cord in the neck. The plexus connects each of the nerves and is responsible for the movement and sensation in each hand. Every person has two brachial plexus that is in the underarm area of each side.
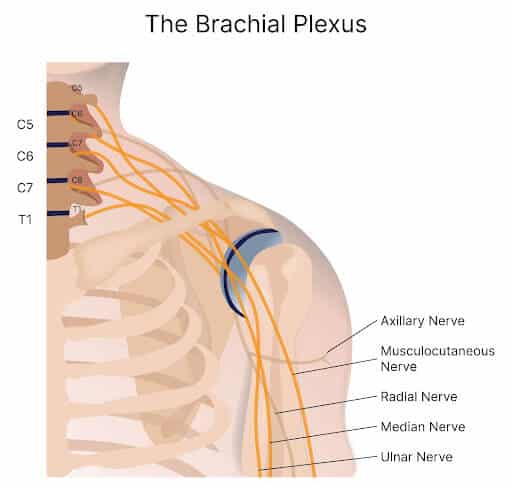
The plexus is divided based on its anatomy. The anterior branches from the spinal nerves C5 through T1 are called the roots of the brachial plexus. These roots join to form superior, inferior, and middle trunks.
The C5 and C6 roots form the superior trunk. The C8 and T1 roots become the inferior trunk. The C7 root becomes the middle trunk. The trunks bundle to form divisions. Each trunk has an anterior and a posterior division which form lateral, posterior, and medial cords. Finally, the brachial plexus has five terminal branches with contributions from the C5-T1 spinal levels.
Brachial plexus injuries can occur at any level. Based on the location of the injury, brachial plexus injuries are classified into the following categories:
- Based on Location: root injuries, cord injuries, trunk injuries or nerve level injuries.
- Based on location of brachial plexus: upple plexus injuries, lower pluexus injuries or global injuries.
- Based on their relation to the clavicle: supra clavicular, retro clavicular, or infra clavicular
Brachial Plexus injuries can be classified in various ways based on location, such as root injuries, cord injuries, trunk injuries or nerve level injuries. In most cases, the injuries are a mixture of all the above.
If they are root injuries, they can be upper plexus injuries that can affect the C5, C6 and may include C7. Lower plexus injuries involve C8 and T1. Gllobal injuries affect all the nerves. Brachial plexus injuries can be classified based on their relation to the clavicle into supra clavicular (above the clavicle), retro clavicular (behind the clavicle), or infra clavicular (below the clavicle).
Symptoms of Brachial Plexus Injuries
Symptoms caused by brachial plexus injuries vary depending on the cause and the location of the injury. Below are the symptoms commonly seen with injury to the brachial plexus.
Numbness Or Loss Of Feeling In Arms
Since the nerves are responsible for sensations in the arm and forearm, any injury to them can cause loss of sensation or numbness to the regions they supply. Damage to the ulnar nerve can cause numbness to the medial side of the forearm.
Inability To Control Movement Of The Shoulder, Arm, Wrist, Or Hand
The nerves of the brachial plexus also control movements of the shoulder, arm, wrist and hand. Any brachial plexus compression or injury can lead to an inability to control movements, like flexion and extension of the elbow and wrist, or fine movements like grasping or writing.
Arm Hanging Limply
The arm hangs limply because the muscles controlling the shoulder and the arm have lost nerve supply or the nerve supply is compromised. As a result, a person cannot hold up their arm, and it hangs flaccidly close to the body.
Severe Or Sudden Pain in Arm
When there is nerve damage, there can be shooting pain along the entire distribution of the nerve. This pain can be sharp and severe since the nerves have pain fibers and are sensitive to pain.
Deep Dive
Arm Pain at Night
Arm pain at night can be miserable. The pain can interrupt your sleep and erode your quality of life. Irritability becomes increasingly more common. What are the causes? When should I worry about it? What are the treatment options for arm pain at night? The neck is composed of 7 boney building blocks numbered 1- 7. Sandwiched between the bones is a disc that functions as an important shock absorber. The cervical discs are susceptible to injury due to trauma, degeneration, repetitive motion, and surgery. Common disc injuries include disc bulges, and herniations. The injured disc can compress or irritate one or more nerves resulting in arm pain at night. It can…
Read More About Arm Pain at NightArm Throbbing
In many patients, irritated neck nerves don’t present as a symptom in the neck. In fact, sometimes the only symptoms of irritated nerves in the neck occur in the arm muscles, as either tightness, throbbing, or both. While the arm throbbing might be frustrating as it’s happening, you might not think a whole lot about it, especially if it only happens on occasion. However, ignoring it is not a good idea since it is often a warning signal of a bigger problem in the neck. These body connections occur all the way back to when we were a fetus, like the neck, shoulder, and arm.
Read More About Arm ThrobbingLeft Arm Numbness
Treatment depends upon the underlying cause of the arm numbness. Left-arm numbness is a warning sign that requires attention. As noted above unexplained numbness requires immediate attention. At the Centeno-Schultz Clinic, we are experts in the treatment of left-arm numbness due to cervical nerve irritation, cervical stenosis, thoracic outlet syndrome, and peripheral nerve injuries. When appropriate first-line treatment should involve conservative care including physical therapy and stretching. Steroid injections should be avoided as they are toxic to orthopedic tissue and can accelerate damage. Surgery for Cervical Stenosis and Thoracic…
Read More About Left Arm NumbnessCommon Causes of Brachial Plexus Injuries
Common causes of brachial plexus injuries, especially in adults, include the following:
Forceful Pulling Of The Arm
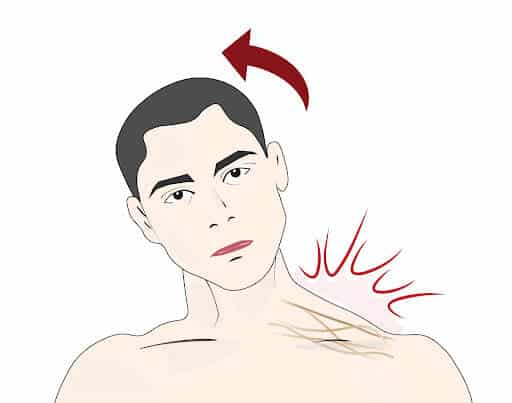
Brachial plexus injuries often occur when the arm is pulled downwards while the head stretches towards the opposite side. This causes the nerves to stretch and tear, especially in the paper trunk.
Blunt Trauma
Blunt trauma can often damage multiple nerves since it is usually seen in polytrauma. Blunt trauma can occur due to multiple injury types, including falls from heights, blows to the arm, or high-speed vehicle collision.
Medical Trauma
Medical trauma, such as difficult obstetric deliveries, can stretch the brachial plexus.
Cancer
Brachial plexus injuries can occur due to tumor infiltration. Lung and breast cancer are very commonly known to cause brachial plexopathy.
Other cancers including lymphoma, melanoma, squamous cell carcinomas from the head and neck, and malignant mesotheliomas often metastasize to the axillary nodes and cause brachial plexus injuries.
Radiation Therapy
Radiotherapy that is usually used to treat various cancers can directly affect the nerves of the brachial plexus.
Brachial plexus compression can also occur due to fibrosis around the nerve plexus after radiotherapy.
Types of Brachial Plexus Injuries
There are different types of brachial plexus injuries; these are explained in detail below.
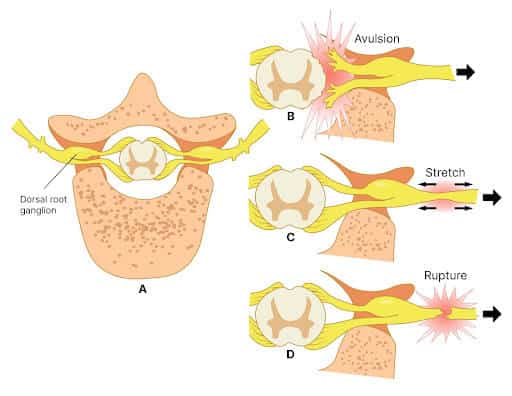
- Stretching (Brachial Plexus Neuropraxia): Neuropraxia simply is a stretching of the nerves. It is the mildest form of injury. Here, the nerve is damaged and the symptoms are due to a change in the signaling within the nerves.
- Avulsion is the most severe type of brachial injury. Here, the nerves are cut or torn from the spinal cord. In incomplete avulsion, the nerve is damaged but not completely torn, which allows the nerve to slowly heal.
- Rupture: A rupture is when the nerve is torn but not at the spinal cord level.
- Neuroma: In a neuroma or a benign nerve growth, the nerve gets torn. It does heal, but with scar tissue. This puts pressure on the already-injured nerve and affects the nerve signaling to the muscles.
- Neuritis: In neuritis, there is local inflammation of the nerve due to injury or infection that could be viral or bacterial.
When Should You Consult Your Doctor?
Since brachial plexus injuries involve the nerves, the presence of certain symptoms should prompt you to consult a doctor immediately. These symptoms may include:
- Numbness/loss of feeling in arm: If you have lost sensation or feeling in the arm for more than a few hours, you should consult a doctor to find out what is compressing or affecting the nerve.
- Inability to move or control shoulder/arm/hand: If you cannot flex your elbow or wrist, or carry out ordinary daily activities with your hand, consider seeing a doctor.
- Arm hangs limply: If your arm hangs loosely close to your body and you cannot abduct or adduct the arm, then you must seek consultation.
- Burning, stinging, or severe pain in arm: Any stinging or shooting pain that is severe and burns may be neuropathic and ought to to be investigated by a doctor.
Diagnostic Procedures Required
To diagnose brachial plexus, a physician may request the following diagnostic procedures:
- X-ray: Plain X-rays are done to identify any fractures of the bones in the arm that could compress the brachial plexus. They are also used to determine if there is an injury to the phrenic nerve, which causes the diaphragm to be raised.
- MRI: This is considered the most useful to visualize the brachial plexus and surrounding structures. It can pinpoint the location of the injury in great detail. They can also identify tumors, root avulsions, and hematomas at the site.
- Nerve Conduction Study: These tests are also known as nerve velocity tests and check how fast nerve impulses are being transmitted via the nerves. The sensory nerve action potential (SNAP) provides details about the sensory nerve axon and its pathway from the skin receptors to the dorsal root ganglia.
The compound muscle action potential (CMAP) investigates the motor nerve fibers from the anterior horn cell to their end in the muscles. The SNAP and CMAP waveforms also help determine the quantity of functioning nerve fibers and the conduction speed. - Electromyogram: Electromyograms are useful to differentiate pre- and postganglionic lesions. In this test, proximal muscles are stimulated via needles. This is done in muscles innervated by nerves branching off at the root level of the brachial plexus. The muscles innervated by the root include the paraspinal, rhomboid, and serratus anterior muscles.
- Diagnostic Ultrasound: Ultrasound allows the user to identify certain muscles, tendons, ligaments and nerves. Plus can trace along the pathway of the nerve looking for any signs of abnormalities such as fluid around the nerve or areas of compression, where the shape of the nerve changes.
Can A Brachial Plexus Injury Heal On Its Own?
The chances of having a mild brachial plexus injury that’s likely to heal on its own with minimal to no medical intervention depends on the kind of injury and the number of nerves that are compressed or injured.
The Likelihood Of A Self-Healing Injury
If you have had mild neuropraxia, the prognosis is excellent. It is not an axonal injury. Self-healing of the avulsion due to root injuries rarely occurs spontaneously. For neuroma and tears, intervention is required. For neuritis, antibiotics or other medication may be needed to treat the cause of the inflammation.
How Long Does It Take To Self-Heal?
In many patients with neuropraxis, recovery would take 2-3 months. In most other injuries, self-healing can take months or years.
What Patients Should Do To Encourage Recovery
Young people tend to have a better functional outcome. However, a home rehab program can facilitate recovery. The goal is to improve the function of the affected limb. This is done by targeted strengthening exercises and by using braces or special equipment.
A home program includes doing stretches or strengthening exercises several times a day. Start using adaptive equipment like large handle silverware, razors and pens. Try pain relieving techniques or desensitization techniques, like bathing with contrasting water temperatures or stroking the arm with different textures. This can help to reduce pain.
Common Treatment Options For Brachial Plexus Injuries
The most common treatment options for brachial plexus injuries are listed below. In most cases, the doctor may try a combination of these treatments for best results.
Physical Therapy
Physical therapy is the first line treatment for injuries of the brachial plexus. Low-energy mechanism injuries of the brachial plexus do very well with physical therapy, which allows for spontaneous recovery. This includes a home program with a therapist that does stretching and range of motion exercises of the upper limb joints.
After a brachial plexus injury, the shoulder joint is contracted. It rotates internally and is adducted. This limits the ability to harness muscle strength due to nerve recovery.
Steroid Injections
Steroid injections can delay degeneration of the nerve. They are injected into the compartment of the brachial plexus and can reduce inflammation and pain. They also improve the function of the muscles.
Assistive Devices
Assistive devices like myoelectric elbow flexion can help individuals with traumatic brachial plexus injuries. They increase independence while doing daily activities.
This is usually used after conservative therapy has failed. Contralaterally controlled functional electrical stimulation (CCFES) uses current from the contralateral side to regulate electrical stimulation delivered to the muscles of the affected upper limb and enable movement.
Medications
Medications like NSAIDs (Non-steroidal anti-inflammatory drugs) and opioids are given to reduce the pain. Neuropathic pain medications like gabapentin and pregabalin are also used to alleviate pain. In some, antidepressants and anticonvulsants are also given to alleviate pain.
Occupational Therapy
Occupational therapy can help individuals with brachial plexus injuries to maintain and restore range of movement during activities of daily living. The therapist will demonstrate how to adapt and learn skills to live normally through stretching and other exercises.
Surgery
Surgery must be considered if a person is still having symptoms even after 3 months of the injury and there has been no healing. This includes nerve repair, neurolysis, nerve grafting, nerve transfer, and tendon transfer.
Are you a Candidate?
When Surgery Is Not An Option
A patient may be discouraged from surgical procedures for their injuries in the following circumstances:
- Common pre-existing conditions: People with chronic pre-existing conditions, such as diabetes, are not suitable candidates for surgery as it slows down the healing and recovery. Individuals whose health prevents them from completing a physical therapy program are poor candidates for surgery.
- Joint stiffness and contractures: The presence of joint stiffness can make placing the hand in a certain position impossible and makes for a poor surgical candidate.
- Advanced age: The healing process of nerves is slow to begin with. In older individuals, this process is much slower and so surgery is not recommended.
- Additional injuries: In individuals where there is polytrauma, like fractures of the bones and other soft tissue injuries, brachial plexus injuries may heal extremely slowly as the body devotes more resources to heal other large surgeries.
- Brain injury: If there is brain injury, the individual who has lost the capacity to execute any movements are poor candidates for surgery.
- Spinal cord injury: If there is spinal cord injury, surgical repair of the nerves is not done because the nerves won;t receive any signal from the brain via a damaged spinal cord.
Risks with Surgery
There are many risks with surgical repair of brachial plexus injuries. They are explained below:
- Slow restoration of desired movement: There is no telling how slowly you will recover. Healing of nerve injuries takes time and so the movement is restored slowly as well.
- Chronic pain: Even after surgery, you may experience pain, discomfort, or numbness since the nerve damage may not heal completely.
- Blood clots: Surgery can cause blood clots, which make you susceptible to heart attacks and strokes.
- Heart attack and stroke: Heart attacks and strokes are a possibility due to the formation of thrombus or emboli during surgery.
When Surgery Is An Option
There are many types of surgical interventions for brachial plexus injuries. They are explained in detail below.
- Nerve Repair: Nerve repairs must be done within the first three months of injury. This is because there is a loss of neuromuscular end plates at around twenty months after denervation. This is done if there are sharp lacerations; the surgeon will simply sew and approximate the torn edges of the nerve together.
- Neurolysis: Neurolysis is a surgical procedure where the nerve is dissected and is freed up from the adhesions and growths that are restricting or compressing it.
- Nerve Graft: A nerve graft is when the nerve is taken from another location and transplanted to the site of the injury to connect a torn nerve. Sural nerves are most commonly used for nerve grafts. A nerve graft is always performed at the site of the injury and can be quite far from the muscle.
- Nerve Transfer: In a nerve transfer, nerves from other parts of the body are transferred closer to the muscle fiber. Therefore, the amount of regeneration is less since the distance is shorter.
- Tendon and Muscle Transfer: In a tendon and muscle transfer, a functioning tendon is attached to the paralyzed tendon affected by the brachial plexus injury. After the transfer, the tendon pulls on the paralyzed tendon to move.
Alternative Treatment Options
There are other treatment options available for brachial plexus injuries that don’t involve medication or surgery at Centeno-Schultz. These include regenerative medicine and cell therapy. These therapies require extensive neurorehabilitation and aid recovery through neurofacilitation.
They include the following:
- Regenerative Therapy: Platelet Rich Plasma and more importantly for nerve healing, Centeno-Schultz and Regenexx unique 4th generation platelet lysate (PL) concentrate. PL is a growth-factor rich injection that is guided under ultrasound guidance that will help stimulate regeneration and healing of the damaged nerve:(3)
- Platelet-derived growth factor (PDGF)
- acts on a number of receptor tyrosine kinases (RTKs) and the downstream PI3K and mitogen-activated protein (MAP) kinase signaling pathways leading to the regeneration of nerve axons
- Insulin-like growth factor-1 (IGF-1)
- IGF-1 induces Schwann cells to synthesize of two fatty acids that are the first step in the process of myelination
- Platelet-released IGF-1 also acts on sciatic nerve Schwann cells to promote their proliferation, synthesis and release of axon regeneration-promoting neurotrophic factors
- Matrix metalloproteinases (MMPs)
- inducing Schwann cells to synthesize and release neurotrophic factors that act directly on neurons to promote axon regeneration
- Epidermal growth factor (EGF)
- Its administration also leads to the development of larger diameter axons and enhanced neurological recovery
- Transforming growth factor-beta (TGF-beta)
- in vivo promotes peripheral axon regeneration by triggering the proliferation of sciatic nerve Schwann cells, as well as their differentiation and release of neurotrophic factors
- Cell Therapy: Cultured expanded stem cells from your own body. Process is not allowed in the US but our physicians travel monthly to Grand Cayman where they are allowed to perform the most advanced form of cellular therapy. Cultured expanded MSC (Mesenchymal stem cells) are used in combination with your own platelets. Our physicians will then hydrodissect the nerve under ultrasound guidance, placing the cells at the location of the nerve injury, allowing nerve regeneration to take place! (2)
- Find out more at http://regenexxcayman.com/
Recovery And Rehabilitation Of Brachial Plexus Injuries
The recovery process for brachial plexus injuries (regardless of whether or not the patient has had surgery) is slow. This is because nerves take time to heal. Here are some highlights about the recovery process:
- How long does it take to recover from an injury?: It can take anywhere between a few months to a year to recover, depending on the type of injury and how many nerves were affected.
- Therapy and Rehabilitation: The goal in brachial plexus injury rehab is to prevent muscle atrophy and secondary deformities, suppression of pain, and the recovery of somato-sensory deficits. Physical therapy and rehab should start almost immediately and must be performed several times a day. Extensive physical therapy is one of the first-line treatments.
- Medication: Medications like pain meds, anti-inflammatory drugs, or steroids can temporarily reduce the pain and inflammation. These are helpful in cases of neuritis and compression.
- Coping Skills: In patients with brachial plexus injuries, coping mechanisms employed include active coping, distraction, denial, behavioral disengagement, venting, planning, self-blame, and acceptance.
Recover From Brachial Plexus Injuries With The Right Treatment
It’s possible to heal from brachial plexus injuries with the right treatment options. However, it’s important to set realistic expectations for recovery. Diagnosing and treating brachial plexus injuries is a complicated process. It requires an interdisciplinary approach that involves the orthopedic doctor, neurologist, and physical therapist.
There are many new treatment options including regenerative medicine that have shown promise. You can schedule an appointment and find out if you are an eligible candidate.

Christopher J. Centeno, MD
Christopher J. Centeno, M.D. is an international expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate in orthopedics.
Dr. Centeno is one of the few physicians in the world with extensive experience in the culture expansion of and clinical use of adult bone marrow concentrate to treat orthopedic injuries. His clinic incorporates a variety of revolutionary pain management techniques to bring its broad patient base relief and results. Dr. Centeno treats patients from all over the US who travel to Colorado to undergo innovative, non-surgical treatments. Dr. Centeno has chaired multiple international research-based conferences. He also maintains an active research-based practice, with multiple publications listed in the US National Library of Medicine. Dr. Centeno has also served as editor-in-chief of a medical research journal dedicated to traumatic injury.
Dr. Centeno trained at the Baylor College of Medicine, Texas Medical Center, and the Institute for Rehabilitation Research. He hails from both Florida and New York and currently resides in Boulder, Colorado with his wife and three children.

John Schultz, MD
John R. Schultz M.D. is a national expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate for orthopedic injuries. He is board certified in Anesthesiology and Pain Medicine and underwent fellowship training in both. Dr. Schultz has extensive experience with same day as well as culture expanded bone marrow concentrate and sees patients at the CSC Broomfield, Colorado Clinic, as well the Regenexx Clinic in Grand Cayman. Dr. Schultz emphasis is on the evaluation and treatment of thoracic and cervical disc, facet, nerve, and ligament injuries including the non-surgical treatment of Craniocervical instability (CCI). Dr. Schultz trained at George Washington School of…
Read more
John Pitts, M.D.
Dr. Pitts is originally from Chicago, IL but is a medical graduate of Vanderbilt School of Medicine in Nashville, TN. After Vanderbilt, he completed a residency in Physical Medicine and Rehabilitation (PM&R) at Emory University in Atlanta, GA. The focus of PM&R is the restoration of function and quality of life. In residency, he gained much experience in musculoskeletal medicine, rehabilitation, spine, and sports medicine along with some regenerative medicine. He also gained significant experience in fluoroscopically guided spinal procedures and peripheral injections. However, Dr. Pitts wanted to broaden his skills and treatment options beyond the current typical standards of care.
Read more
Jason Markle, D.O.
Post-residency, Dr. Markle was selected to the Interventional Orthopedic Fellowship program at the Centeno-Schultz Clinic. During his fellowship, he gained significant experience in the new field of Interventional Orthopedics and regenerative medicine, honing his skills in advanced injection techniques into the spine and joints treating patients with autologous, bone marrow concentrate and platelet solutions. Dr. Markle then accepted a full-time attending physician position at the Centeno-Schultz Clinic, where he both treats patients and trains Interventional Orthopedics fellows. Dr. Markle is an active member of the Interventional Orthopedic Foundation and serves as a course instructor, where he trains physicians from around the world.
Read more
Brandon T. Money, D.O., M.S.
Dr. Money is an Indiana native who now proudly calls Colorado home. He attended medical school at Kansas City University and then returned to Indiana to complete a Physical Medicine and Rehabilitation residency program at Indiana University, where he was trained on non-surgical methods to improve health and function as well as rehabilitative care following trauma, stroke, spinal cord injury, brain injury, etc. Dr. Money has been following the ideology behind Centeno-Schultz Clinic and Regenexx since he was in medical school, as he believed there had to be a better way to care for patients than the status quo. The human body has incredible healing capabilities…
Read moreYour brachial plexus injury can be treatable with the right approach. Consult with us today!
Other Resources for Brachial Plexus Injury
-
Exploring the Anatomical Structures of an Ulnar Nerve
The human body is a marvel of intricate design, and its functioning relies on a network of complex systems. Among these, the nervous system serves as the communication highway, transmitting signals that enable us to move, feel, and interact with the world around us. One crucial component of this neural network is the ulnar nerve,…
-
What Are the Long Term Effects of Untreated Whiplash?
You were waiting for the red light to change when you heard the brakes screeching. Out of nowhere a large SUV rear ends you and pushes your vehicle into the intersection. Your neck and shoulder hurt and you’re not processing all the information. Your doctor thinks you have Whiplash. What is Whiplash? What are the…
-
Neck Fusion Problems Years Later – 10 Complications to Be Wary Of
Stabbing, persistent neck pain can be disabling. Patients often turn to neck fusion, a surgical procedure, in the hopes of eliminating the pain. While the procedure aims to address chronic neck pain, it is crucial to recognize potential complications that may arise even years after the surgery. Understanding these complications is essential for patients. Let’s…
-
Pain radiating down my arm after shoulder surgery
Specialized doctor discussed causes of radiating arm pain following shoulder surgery.