What Is the Cubital Tunnel Syndrome?
Cubital Tunnel Syndrome, a compressive neuropathy of the ulnar nerve at the elbow, is the second most common compressive neuropathy in upper extremities (1st = carpal tunnel syndrome). To understand how peripheral nerves get injured, read this blog: https://centenoschultz.com/nerve-hydrodissection/
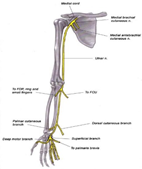
The Ulnar nerve is a continuation of nerve roots from your middle and lower neck (cervical spine) that get combined in the upper arm and then travel down the inside of your arm. It enters the cubital tunnel on the inside of your elbow and then travels to your hand.
How Successful Is Cubital Tunnel Surgery?
In recent years, physicians have been favoring surgery. In a study by Osei et al., 41.3% of patients diagnosed with cubital tunnel syndrome were eventually treated surgically in their study period of 6 years. BUT does the level of evidence favor the need for such high surgical conversion rates? (Osei)
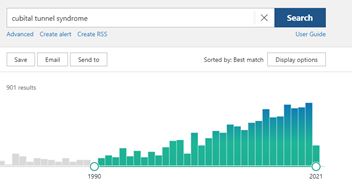
The amount of Cubital Tunnel Surgery research has increased but very few high-level studies even exist to confirm the safety and efficacy of surgery. A 2019 meta-analysis demonstrated that “[t]he current body of evidence regarding Cubital Tunnel Syndrome lacks prospective, randomized, controlled trials, uniform reporting of indications, and standardized outcome scoring” (Said).
Revision rates for persistent or recurrent Cubital Tunnel Syndrome are at around 19% (almost 2 out of 10 patients need another surgery!). Common causes for failure include the incomplete release of the entrapment and postoperative perineural scarring (avache). The most common finding in revision surgery was perineural scarring (79%), with the most frequent entrapment site being the medial intermuscular septum (33%) (kho). Studies also show that the outcome of revision surgery is less favorable than after primary surgery and complete resolution of symptoms is unlikely.
To get surgery or not? Functional outcomes were averagely reported and varied widely. A consensus regarding the functional outcome parameters after surgery for Cubital Tunnel Syndrome is urgently needed.
The Future: Non-Surgical Alternatives
We continue to push the boundaries of interventional procedures utilizing the most advanced regenerative ortho-biologics to allow natural healing of the nerve while hydrodissecting, percutaneously decompressing without the need for surgery! If you’d like to find out if you’re a candidate for our advanced peripheral nerve injury treatment, feel free to contact us today for a full evaluation.
Doctors Who Help Patients Avoid Cubital Tunnel Syndrome Surgery
Also Known as Cubital Tunnel Release Procedure

Christopher J. Centeno, MD
Christopher J. Centeno, M.D. is an international expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate in orthopedics. He is board-certified in physical medicine and rehabilitation with a subspecialty of pain medicine through The American Board of Physical Medicine and Rehabilitation. Dr. Centeno is one of the few physicians in the world with extensive experience in the culture expansion of and clinical use of adult bone marrow concentrate to treat orthopedic injuries. His clinic incorporates a variety of revolutionary pain management techniques to bring its broad patient base relief and results. Dr. Centeno treats patients from all over the US who…
Read more
John Schultz, MD
John R. Schultz M.D. is a national expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate for orthopedic injuries. He is board certified in Anesthesiology and Pain Medicine and underwent fellowship training in both. Dr. Schultz has extensive experience with same day as well as culture expanded bone marrow concentrate and sees patients at the CSC Broomfield, Colorado Clinic, as well the Regenexx Clinic in Grand Cayman. Dr. Schultz emphasis is on the evaluation and treatment of thoracic and cervical disc, facet, nerve, and ligament injuries including the non-surgical treatment of Craniocervical instability (CCI). Dr. Schultz trained at George Washington School of…
Read more
John Pitts, M.D.
Dr. Pitts is originally from Chicago, IL but is a medical graduate of Vanderbilt School of Medicine in Nashville, TN. After Vanderbilt, he completed a residency in Physical Medicine and Rehabilitation (PM&R) at Emory University in Atlanta, GA. The focus of PM&R is the restoration of function and quality of life. In residency, he gained much experience in musculoskeletal medicine, rehabilitation, spine, and sports medicine along with some regenerative medicine. He also gained significant experience in fluoroscopically guided spinal procedures and peripheral injections. However, Dr. Pitts wanted to broaden his skills and treatment options beyond the current typical standards of care.
Read more
Jason Markle, D.O.
Post-residency, Dr. Markle was selected to the Interventional Orthopedic Fellowship program at the Centeno-Schultz Clinic. During his fellowship, he gained significant experience in the new field of Interventional Orthopedics and regenerative medicine, honing his skills in advanced injection techniques into the spine and joints treating patients with autologous, bone marrow concentrate and platelet solutions. Dr. Markle then accepted a full-time attending physician position at the Centeno-Schultz Clinic, where he both treats patients and trains Interventional Orthopedics fellows. Dr. Markle is an active member of the Interventional Orthopedic Foundation and serves as a course instructor, where he trains physicians from around the world.
Read more
Brandon T. Money, D.O., M.S.
Dr. Money is an Indiana native who now proudly calls Colorado home. He attended medical school at Kansas City University and then returned to Indiana to complete a Physical Medicine and Rehabilitation residency program at Indiana University, where he was trained on non-surgical methods to improve health and function as well as rehabilitative care following trauma, stroke, spinal cord injury, brain injury, etc. Dr. Money has been following the ideology behind Centeno-Schultz Clinic and Regenexx since he was in medical school, as he believed there had to be a better way to care for patients than the status quo. The human body has incredible healing capabilities…
Read moreAm I a Candidate?
To answer this question, fill out the candidate form below to request a new patient evaluation, and a patient advocate will reach out to you to determine your next steps. Your one-hour, in-office or telemedicine evaluation will be with one of the world’s experts in the field of Interventional Orthopedics.