Want to Avoid Spinal Fusion?
If information about spinal fusion surgery has you concerned or reticent, you should know that there are alternatives to having major spinal fusion surgery. There is another way. Centeno-Schultz has been using this alternative to spinal fusion for the last decade with great success (1). This groundbreaking procedure is a fusion substitute pioneered by our team, called the Perc-FSU Procedure.
The Perc-FSU Procedure is an injection-based treatment that utilizes the patients’ own blood platelets to bring stability to the spine without the need for the rods, nuts, bolts, and hardware of fusion surgery. “Perc” stands for percutaneous, and “FSU” stands for “Functional Spinal Unit,” which means that the spine is treated as one functioning unit. Up and down the spine, the discs, facet joints, ligaments, and muscles that assist in stabilizing the spine are treated with image-guided injections of PRP and Platelet Lysate to help bring stability to the spine as a whole. It is the trusted alternative to spinal fusion.
Quick Links
FAQs
We are running a Clinical Trial for Degenerative Disc Disease.
Meet the Perc-FSU
Annular Tear
To understand annular tears, let us first review the anatomy of the spine. The lumbar spine is comprised of 5 boney building blocks called vertebral bodies. Sandwiched between the vertebral bodies are the lumbar discs. Each disc is comprised of an outer fibrous ring, the annulus fibrosis that surrounds the inner gelatinous center, which is called the nucleus. The disc absorbs the forces of daily living. The annulus has multiple layers of collagen that provide important support. The annulus is similar to the sidewall of a tire which provides important stability for the tire. Through trauma or degeneration, the outer annular fibers can become injured and or weakened.
Read More About Annular TearBulging Disc In Thoracic Spine
A bulging disc in the thoracic spine is a serious medical condition that occurs when the outer layer of the disc weakens, causing it to bulge outward and put pressure on nerves and the spinal cord. The disc has two components, a soft center and a thick outer layer, and weakening or tears in the outer layer can lead to a bulge. Symptoms include pain, numbness, and weakness in the affected area. The thoracic spine is that portion of the spine that resides below the neck and above the low back. It is commonly referred to as the mid-back. A bulging…
Read More About Bulging Disc In Thoracic SpineFacet Joint Syndrome
Injury or inflammation of the cervical facet can led to neck, shoulder and headache pain – called “cervical facet syndrome.” Cervical facet syndrome largely involves a joint in the posterior aspect of the cervical spine. It functions to provide stability and guide motion. cervical facet joint injection for cervical facet syndrome Cervical facet pain is common in patients who have sustained a whiplash injury, trauma to the neck or undergone cervical fusion. Physical examination is typically significant for restriction in range of motion along with pain. Each joint has a distinct referral pattern illustrated below. The Centeno-Schultz Clinic are experts at diagnosing and treating cervical facet dysfunction. Injury to the joint is not commonly detected by conventional radiographic studies.
Read More About Facet Joint SyndromeFacet Synovial Cyst
A facet cyst, also known as a synovial cyst, is a fluid-filled sac that forms in the facet joint of the spine. The facet joints are small joints located between the vertebrae of the spine that provide stability and enable movement. Facet cysts typically develop due to degeneration and wear and tear of the facet joint, which can cause the joint capsule to stretch and weaken. This weakened capsule can then allow synovial fluid, which normally lubricates and nourishes the joint, to leak out and form a cyst. Facet cysts can cause various symptoms such as back pain, leg pain…
Read More About Facet Synovial CystFailed Back Surgery Syndrome
Failed Back Surgery Syndrome also called failed back is a clinical condition in which patients who have undergone low back surgery continue to have pain and dysfunction. Said another way the surgery that was intended to reduce pain and increase function FAILED. That is right, the surgery failed. You had the surgery, struggled with the pain postoperatively, diligently participated in physical therapy and yet the pain and limitation are still there. Unfortunately, this occurs frequently. Estimates range from 20-40% of patients who undergo low back surgery will develop Failed Back Surgery Syndrome. Pain is the most common symptom of Failed Back Surgery Syndrome…
Read More About Failed Back Surgery SyndromeHerniated Thoracic Disc
A herniated thoracic disc is especially difficult because there are not as many treatments available as there are for disc herniations in other areas of the spine. To understand Thoracic Disc Herniations, though, we first need to cover thoracic spine anatomy and function. With disc herniation, the annulus fibrosus get small tears throughout the annulus. An annulus is a bunch of concentric fibers, so, as the fibers get damaged and cut, the pressure that is built up within the nucleus pushes the now weakened annulus outward, creating a bulge or herniation. The disc begins to weaken via mild degeneration/tearing of the annular fibers…
Read More About Herniated Thoracic DiscLesions on Thoracic Spine
The evaluation of the lesion in the thoracic spine involves many steps. The first step is a detailed medical history where the following is documented: onset of symptoms, duration, location, intensity, aggravating and alleviating factors, and treatment to date. Physical Examination: Evaluation of range of motion, area of tenderness, motor strength, sensation to pinprick, and detailed neurologic examination. Radiographic Studies: Radiographic tests are essential and may include:X-ray: Low-cost and readily available, X-rays provide an image of the bones and can reveal fractures, dislocation, osteoporosis, and deformities like scoliosis and kyphosis. It is often the first-line diagnostic tool used to evaluate spinal conditions. Low amount…
Read More About Lesions on Thoracic SpinePinched Nerves in the Back
We talk a lot about leg pain stemming from a pinched or irritated nerve in the lower back. And, indeed, that’s what our physicians are traditionally taught in medical school—a pinched nerve in the lumbar spine typically presents as a symptom in the leg. However, what if you have some butt pain but no pain or other symptoms in the leg? Does this mean it couldn’t be a pinched nerve? Not so fast. Turns out a pinched low back nerve doesn’t always have to be accompanied by leg symptoms. Let’s start by taking a look at how the back is structured.
Read More About Pinched Nerves in the BackSciatica
Disc herniation, disc protrusion, overgrowth of the facet joint, and thickening of the ligaments can result in nerve root compression or irritation, causing symptoms of sciatic compression. Some causes of sciatic compression can be interrelated with the following conditions: Degenerative disc disease, Spinal stenosis, damage or injuries to the discs, spondylolisthesis, piriformis syndrome, osteoarthritis. The symptoms of sciatica include pain in the lower back, buttock, and down your leg, numbness and weakness in low back, buttock, leg, and/or feet, pain increase with movement, “Pins and needles” feeling in your legs, toes, or feet., loss of bowel control, and incontinence. Sciatica can be treated…
Read More About SciaticaSpinal Instability
Spinal instability is a condition that occurs when the spinal column is not able to maintain its normal alignment and function under normal loads. It can be caused by various factors such as trauma, degenerative changes, infections, tumors, or congenital abnormalities. In a stable spine, the bones, discs, ligaments, and muscles work together to support and protect the spinal cord and nerve roots. However, in an unstable spine, the structures that support the spine may be damaged or weakened. This can lead to abnormal movement and excessive stress on the spinal cord and nerves. In most cases, bone and joint problems…
Read More About Spinal InstabilitySpinal Stenosis
Spinal stenosis is the narrowing of the central spinal canal and is a cause of significant pain and disability. Common causes of spinal stenosis include disc protrusion, facet overgrowth and ligamentum flavum thickening. Surgery is often chosen when conservative therapies fail despite the lack of convincing evidence that it is a superior treatment option. Are there alternatives to back surgery for spinal stenosis? Yes. Regenexx DDD utilizes precise platelet injections into the facets, muscles, and ligaments to treat the lumbar stenosis, treating all of the components of the issue, which is crucial. Spinal stenosis is often an age-related condition attributed…
Read More About Spinal StenosisSpondylolisthesis
Spondylolisthesis means that one vertebra is slipping forward or backwards on another. This causes the hole where the nerve exits (foramen) to get smaller (also called foraminal stenosis). It also causes more wear and tear on the facet joint which can lead to arthritis or what’s called “facet hypertrophy”. spondylolisthesis recovery The amount of slippage is graded 1-4, with grade 1 meaning that the one vertebra has slipped up to 25% on the other vertebra. Grade 2 means that one bone has slipped from 25-50% with higher grades indicating more slippage. The vast majority of patients are grade 1 to 2.
Read More About SpondylolisthesisThoracic Degenerative Disc Disease
Degenerative disc disease is a clinical condition that refers to the gradual deterioration of the discs located in the thoracic spine and the associated symptoms. Pain, weakness, muscle spasms, and restriction in range of motion are common. Degenerative disc disease can occur at each level of the spine: cervical, thoracic, and lumbar. Studies have demonstrated that degenerative disc disease in the thoracic spine most commonly occurs in the third to fourth decades (1) and occurs most frequently in the lower thoracic segments from T7-T12. Thoracic degenerative disc…
Read More About Thoracic Degenerative Disc DiseaseThoracic Radiculopathy
Thoracic radiculopathy is a painful medical condition that affects both men and women alike. Pain, paresthesia, decreased sensation, and weakness are the major symptoms. Radiculopathy refers to the whole complex of symptoms that can be caused by irritation or compression of a nerve root in the spine. Thoracic radiculopathy is irritation or compression of a thoracic spinal nerve. Causes of radiculopathy in the thoracic region are thoracic disc injuries, thoracic facet arthritis, ligament thickening, facet cyst, unstable rib attachments, and bone spurs. Diagnosis of thoracic radiculopathy can be difficult….
Read More About Thoracic RadiculopathyTorn Discs
The spinal discs are shock absorbers that live at each level between the vertebral bones (1). They have a tough outer annulus part and a soft inner gel part (nucleus pulposis). The outer covering can get damaged which can sometimes be seen on MRI and other times requires additional testing to identify. These tears are called: a torn disc, a disc tear, an annular tear, and when seen on MRI a “High-Intensity Zone” or HIZ. They can cause pain, mostly through ingrown nerves. There are torn disc findings that can be seen on MRI (HIZ) and these can be either asymptomatic (i.e. not painful) or…
Read More About Torn DiscsWhat Are the Complications Associated with Spinal Fusion?
An unfortunate and major complication of spinal fusion surgery is an overall failure of the procedure. Spinal fusion can fail, and there are a few main ways that happen, which include:
➜ Non-union: If the segment being fused with the bone fails to grow together, this is called “non-union.” The rate at which non-union occurs is highly dependent upon the type of spinal fusion surgery performed. If a procedure requires more bone, such as a posterior-lateral fusion, non-union rates can be as high as 26 – 36% (2,3)
➜ Hardware that loosens or breaks, or pain resulting from hardware used: These hardware-centric complications are a common reason that second surgeries need to be performed after the initial fusion. Overall, roughly 13% of patients undergoing fusion because of low-back problems require a second surgery (4).
RIP Back Fusion Surgery
➜ Adjacent segment disease (ASD): ASD is caused by excessive force on vertebral levels above or below the fusion area, causing them to be worn out because of the immobile fusion (5). It is estimated that as many as 12% of patients will develop ASD within two years of their spinal fusion procedure (16), and 2 – 4% of patients will develop this problem for every year post-fusion, for example, at 5 years from the fusion date, 20% of patients will have developed ASD (6).
Will the Perc-FSU help if I’ve Already Had Back Fusion?
- Fusion predictably breaks down the unfused vertebral segments below and above fusion site
- The solution is NOT more fusion
- The Perc-FSU can help by strengthening the ligaments, muscles, joint, and nerves below and above the site of the back fusion
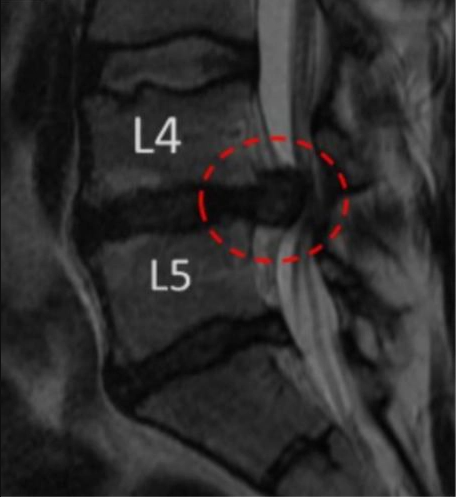
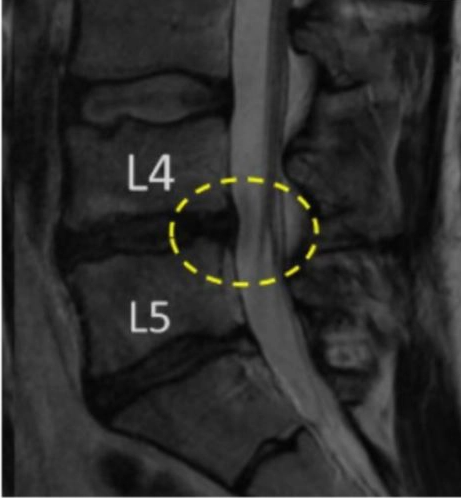
Before and After MRI of Perc-FSU Procedure
Patient 1
Before:
After:
Frequently Asked Questions
What is spinal fusion, anyway? Why would someone need their spine fused?
When patients go in for continual low back pain, they could be found to have chronic pain problems or degenerative disc disease — problems that won’t go away on their own. Instead of leaving them untreated and surely allowing the pain to get worse, spinal fusion surgery is often recommended. This surgery is done by fusing certain segments of the spine together, typically with bone and/or hardware, in order to prevent motion from that particular spinal segment. The idea is that, with little to no motion, further erosion and increased pain cannot occur.
How well does spinal fusion work? What is the success rate?
This answer is a bit more complicated because the research has shown that the success rate for spinal fusion is largely dependent on the reason someone needs surgery in the first place. In the largest published investigation to date, researchers looked at the results of 65 studies and more than 300,000 patients and found that the success rates were variable; there wasn’t, in this study, a definitive answer on the success rate of spinal fusion for surgical patients with low back pain, versus patients with low back pain who opted out of surgery (7). Furthermore, there was no difference in pain levels between those who underwent spinal fusion and those who did not. For patients who had a slipped vertebra (otherwise known as spondyloisthesis), the spinal fusion procedure did have greater success; however, most patients who pursue spinal surgery are not in that category, but instead have chronic low back pain. The research shows that, for these patients that make up the majority, the fusion surgery did not make any distinguishable improvements upon their way of life.
Is spinal fusion considered a major surgery?
In a word, yes. Because complications resulting from spinal fusion are common, this procedure is considered major surgery. Research demonstrates that surgeons can underestimate complications (9), and that the serious complication rate of spinal surgery is 10-24%, according to an analysis that reviewed five larger studies on the same subject (10). Even when minimally invasive fusions were used, which are comprised of smaller incisions, the reported complication rate was 19%, with some studies reporting fusion complication rates as high as 31% (11). Side effects from spinal fusion can also include nerve damage and infection, among other problems that can lead to a need for more surgery.
How long will I be in recovery after spinal fusion?
Depending upon the type of surgical method used, patients can expect to be prescribed narcotics for lingering pain for between two and nine weeks post-surgery (5-7). Recommended time away from work can vary from as little as seven weeks to more than six months, depending upon the patient, the surgical method, and any potential complications. Most surgeons tell their patients that they can expect to wait a year before full recovery has taken place.
What is failed back surgery syndrome?
There is no ambiguity in this phrase. This is the diagnosis you could receive if your back surgery failed to reduce pain and increase function. Unfortunately, this happens often, estimates ranging from 20 – 40% of patients that undergo low back surgery will develop failed back surgery syndrome (17).
Is the Perc-FSU an alternative for spondylolisthesis surgery?
Spondylolisthesis is a Latin term that basically translates to “slipped spine” – “spondy” translating to spine and “listhesis” to “slipped.”
There are two main categories of this condition:
1. Trauma induced – This is when the bone that separates the facet joints, the pars interarticularis, is broken, allowing the vertebral bodies to “slip” and move around. As you may have guessed, this can cause irritation (esp. to the nerves) and pain.
2. Degenerative spondylolisthesis – This means it is degenerative and a condition that a person can have from birth. When the facet joints of the spine get arthritic, they become deformed.
Treating spondylolisthesis involves treating the spine as a functional unit, thus stabilization of the spine here is like treating other spine conditions. Meaning, because we use platelet based procedures to tighten up and strengthen ligaments, epidural, facets, multifidus muscles, painful tendons, and sometimes discs.
References
(1) Centeno C, Markle J, Dodson E, et al. The use of lumbar epidural injections for treatment of radicular pain. J Exp Orthop. 2017;4(1):38. Published 2017 Nov 25. doi: 10.1186/s40634-017-0113-5
(2) Herkowitz HN, Kurz LT. Degenerative lumbar spondylolisthesis with spinal stenosis. A prospective study comparing decompression with decompression and intertransverse process arthrodesis. J Bone Joint Surg Am. 1991 Jul; 73(6):802-8.
(3) Tsutsumimoto T, Shimogata M, Yoshimura Y, Misawa H. Union versus nonunion after posterolateral lumbar fusion: a comparison of long-term surgical outcomes in patients with degenerative lumbar spondylolisthesis. Eur Spine J. 2008;17(8):1107–1112. doi: 10.1007/s00586-008-0695-9
(4) Greiner-Perth R, Boehm H, Allam Y, Elsaghir H, Franke J. Reoperation rate after instrumented posterior lumbar interbody fusion: a report on 1680 cases. Spine (Phila Pa 1976). 2004 Nov 15;29(22):2516-20. https://www.ncbi.nlm.nih.gov/pubmed/15543064
(5) Saavedra-Pozo FM, Deusdara RA, Benzel EC. Adjacent segment disease perspective and review of the literature. Ochsner J. 2014;14(1):78–83. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3963057/
(6) Tobert DG, Antoci V, Patel SP, Saadat E, Bono CM. Adjacent Segment Disease in the Cervical and Lumbar Spine. Clin Spine Surg. 2017 Apr;30(3):94-101.
(7) Yavin D1, Casha S1, Wiebe S, Feasby TE, Clark C, Isaacs A, Holroyd-Leduc J, Hurlbert RJ, Quan H, Nataraj A, Sutherland GR, Jette N. Lumbar Fusion for Degenerative Disease: A Systematic Review and Meta-Analysis. Neurosurgery. 2017 May 1;80(5):701-715. doi: 10.1093/neuros/nyw162.
(8) Wang X, Borgman B, Vertuani S, Nilsson J. A systematic literature review of time to return to work and narcotic use after lumbar spinal fusion using minimal invasive and open surgery techniques. BMC Health Serv Res. 2017;17(1):446. Published 2017 Jun 27. doi: 10.1186/s12913-017-2398-6
(9) Ratliff JK, Lebude B, Albert T, Anene-Maidoh T, Anderson G, Dagostino P, Maltenfort M, Hilibrand A, Sharan A, Vaccaro AR. Complications in spinal surgery: comparative survey of spine surgeons and patients who underwent spinal surgery. J Neurosurg Spine. 2009 Jun;10(6):578-84. doi: 10.3171/2009.2.SPINE0935.
(10) Zaina F, Tomkins-Lane C, Carragee E, Negrini S. Surgical versus non-surgical treatment for lumbar spinal stenosis. Cochrane Database Syst Rev. 2016;2016(1):CD010264. Published 2016 Jan 29. doi:10.1002/14651858.CD010264.pub2
(11) Joseph JR, Smith BW, La Marca F, Park P. Comparison of complication rates of minimally invasive transforaminal lumbar interbody fusion and lateral lumbar interbody fusion: a systematic review of the literature. Neurosurg Focus. 2015 Oct;39(4):E4. doi: 10.3171/2015.7.FOCUS15278.
(12) Adogwa O, Parker SL, Bydon A, Cheng J, McGirt MJ. Comparative effectiveness of minimally invasive versus open transforaminal lumbar interbody fusion: 2-year assessment of narcotic use, return to work, disability, and quality of life. J Spinal Disord Tech. 2011;24(8):479–484. https://www.ncbi.nlm.nih.gov/pubmed/21336176
(13) Parker SL, Adogwa O, Bydon A, Cheng J, McGirt MJ. Cost-effectiveness of minimally invasive versus open transforaminal lumbar interbody fusion for degenerative spondylolisthesis associated low-back and leg pain over two years. World Neurosurg. 2012 Jul;78(1-2):178-84. doi: 10.1016/j.wneu.2011.09.013.
(14) Parker SL, Mendenhall SK, Shau DN, Zuckerman SL, Godil SS, Cheng JS, et al. Minimally invasive versus open Transforaminal lumbar Interbody fusion for degenerative Spondylolisthesis: Comparative effectiveness and cost-utility analysis. World Neurosurg. 2013.
(15) MacDowall A, Canto Moreira N, Marques C, Skeppholm M, Lindhagen L, Robinson Y, Löfgren H, Michaëlsson K, Olerud C. Artificial disc replacement versus fusion in patients with cervical degenerative disc disease and radiculopathy: a randomized controlled trial with 5-year outcomes. J Neurosurg Spine. 2019 Jan 11;30(3):323-331. doi: 10.3171/2018.9.SPINE18659.
(16) Tobert DG, Antoci V, Patel SP, Saadat E, Bono CM. Adjacent Segment Disease in the Cervical and Lumbar Spine. Clin Spine Surg. 2017 Apr;30(3):94-101. doi: 10.1097/BSD.0000000000000442. [Google Scholar]
(17) Thomson S. Failed back surgery syndrome – definition, epidemiology and demographics. Br J Pain. 2013;7(1):56-59. doi:10.1177/2049463713479096.
THE BROADEST ARRAY OF NON-SURGICAL PROCEDURES FOR SPINE AND CERVICAL CONDITIONS IN COLORADO
Am I a Candidate?
To answer this question, fill out the candidate form below to request a new patient evaluation, and a patient advocate will reach out to you to determine your next steps. Your one-hour, in-office or telemedicine evaluation will be with one of the world’s experts in the field of Interventional Orthopedics.