PRP for Plantar Fasciitis
Am I a Candidate?Experiencing the continuous discomfort of plantar fasciitis can significantly hinder your day-to-day activities, affecting everything from a simple walk to standing for extended periods. Our clinic offers a cutting-edge approach to addressing this common, yet often stubborn, foot condition through the use of PRP (platelet-rich plasma) therapy.
This article will cover everything you need to know about PRP for plantar fasciitis, including what it is, how it works, and its benefits compared to other treatments.
What Is the Plantar Fascia?
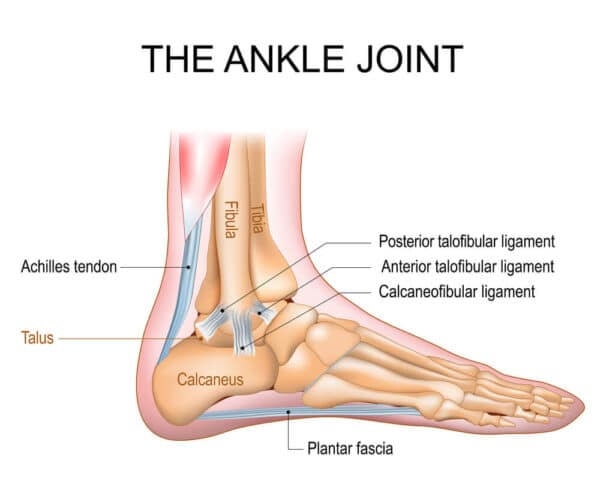
The plantar fascia is a thick band of tissue that runs across the bottom of your foot, connecting your heel bone to your toes. It functions like a bowstring, supporting the arch of your foot and helping you walk.
When you step, the plantar fascia helps absorb the impact and distribute pressure through your foot. The plantar fascia is crucial for balance, stability, and the overall mechanics of walking.
What Is Plantar Fasciitis?
Plantar fasciitis is a painful medical condition characterized by pain in the heel and bottom of the foot. It occurs when the plantar fascia, the band of tissue that supports the arch of the foot, becomes inflamed, irritated, or injured.
Plantar fasciitis is the most common cause of chronic pain in the heel. It occurs in about 10% of the general population with 83% of these patients between 25 and 65 years of age. The peak incidence is between 40 to 60 years (1). There is a higher prevalence of plantar fasciitis in women compared to men (2).
What Are the Symptoms of Plantar Fasciitis?
The most common symptoms of plantar fasciitis include:
- Heel pain: This is the most characteristic symptom, often described as a sharp, stabbing pain in the bottom of the heel, which may feel like a knife is digging into the foot.
- Pain with first steps: The pain is usually most intense with the first steps after waking in the morning, or after long periods of sitting or being off the feet.
- Stiffness and tenderness: The heel may be stiff or tender to the touch, which can make it difficult to walk properly.
- Swelling: Some patients notice swelling around the heel.
What Are the Major Causes of Plantar Fasciitis?
Plantar fasciitis is primarily an overuse injury caused by repeated strain and micro-tears to the plantar fascia, the thick connective tissue that runs from the heel to the front of the foot.
When examined under a microscope, the fascia in most cases is noted to have granulation tissue, microtears, and collagen disarray, consistent with a degenerative process as opposed to an inflammatory process (3).
Associated Risk Factors
The most common risk factors associated with plantar fasciitis include:
- Obesity: There is a strong association between increased body mass index (BMI) and plantar fasciitis. Obesity is present in up to 70% of patients with plantar fasciitis (4).
- Heel spurs: Heel spurs are common in patients with plantar fasciitis.
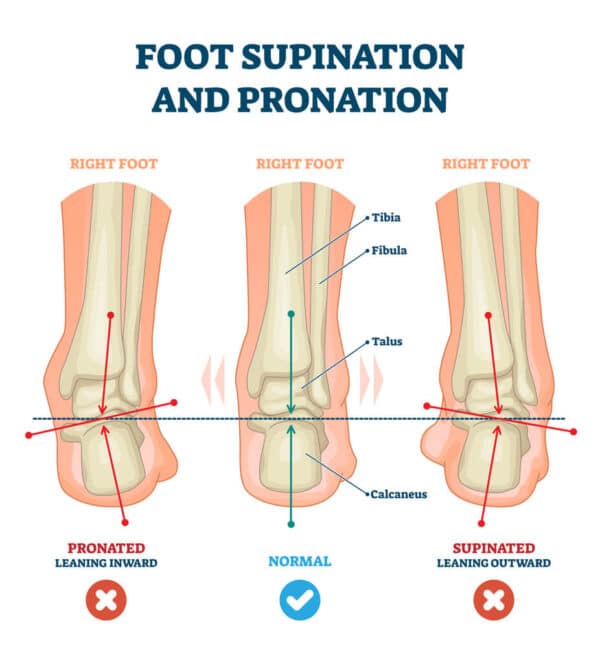
- Excessive pronation: Excessive pronation occurs in 81-86% of patients with plantar fasciitis (5). Foot pronation is a natural movement of the foot that occurs during walking or running. When you walk or run, your foot normally rolls inward slightly as it hits the ground. Excessive pronation occurs when the foot rolls inward too much during the walking or running cycle.
- Age: As we age, the plantar fascia loses its elasticity and the fat pad on the heel thins out, providing less cushioning.
- Low back nerve irritation: Irritation or compression of a lumbar nerve root can compromise the electrical signal to the muscles in the lower leg, leading to tightness and dysfunction.
What Is a Platelet-Rich Plasma Therapy Injection?
A PRP therapy injection involves using platelet-rich plasma (PRP), which is a concentration of platelets from your blood. These platelets are vital for wound healing because they are rich in growth factors. The most beneficial growth factors in PRP include:
- Platelet-derived growth factor (PDGF): PDGF stimulates cell replication, promotes new blood vessel formation, and aids in the regeneration of skin and connective tissue.
- Vascular endothelial growth factor ( VEGF): VEGF promotes the formation of new blood vessels, which are essential for bringing nutrients to damaged tissues to enhance healing.
- Transforming growth factor – beta (TGF-B): TGF-B is important for the growth of bone and cartilage and also helps in the regulation and development of the immune system.
The PRP is injected under ultrasound and X-ray guidance into the plantar fascia and other targeted structures. Examples include the lateral and medial ankle ligaments that may be injured or lax, leading to ankle instability, which can aggravate plantar fasciitis.
PRP Injections Versus Steroid Injections
Steroids are powerful anti-inflammatory agents that are often recommended when patients fail conservative care. Common examples include hydrocortisone, triamcinolone, and methylprednisolone.
When comparing PRP and steroid injections for treating plantar fasciitis, PRP is a superior option, particularly for long-term management. PRP involves using a concentration of the patient’s own platelets to stimulate healing in the damaged plantar fascia.
This method enhances the body’s natural healing processes, releasing growth factors that repair tissue and reduce inflammation over time. Unlike steroids, which offer quick, temporary relief by suppressing inflammation, PRP supports sustained healing, reducing the likelihood of symptom recurrence.
Studies suggest that while the initial pain relief with PRP may be slower, the long-term benefits in terms of functionality and pain reduction are more substantial and enduring.
In contrast, steroid injections, though less expensive, carry risks of weakening the plantar fascia with repeated use, potentially leading to rupture. Additionally, the relief provided by steroids is usually short-lived, and symptoms can return as the anti-inflammatory effects wear off.
Studies on PRP Treatments for Plantar Fasciitis
There are an increasing number of studies that examine the use of PRP in the treatment of plantar fasciitis. The major ones are listed and summarized below.
2015 Study
In 2015, 60 patients who had failed physical therapy and conservative care underwent either PRP or steroid injections. After three months, both groups had made some improvements. However, after about six months and 12 months, the improvements made by the steroid group had worn off.
PRP was demonstrated to be superior as it provided longer relief with no significant side effects. In contrast, steroids are short-lived and can damage the plantar fascia along with your local stem cells.
2017 Study
Another study, in 2017, was a meta-analysis of nine previous studies of a total of 430 patients being treated with either PRP or steroids. At six months and one year, the PRP was superior in reducing pain levels and improving function.
Other important studies that examined the use of PRP in the treatment of plantar fasciitis include:
- Monteagudo et al. (2018): This study reviewed current concepts around plantar fasciopathy, discussing the effectiveness of PRP as an alternative treatment to traditional methods like corticosteroids, and highlighting PRP’s potential to enhance healing through growth factors (6).
- Peerbooms et al. (2010): These researchers conducted a randomized controlled trial comparing PRP injections to corticosteroid injections in patients with chronic plantar fasciitis. The study found that PRP injections were more effective in reducing pain and improving function over a longer period compared to steroids (7).
- Ragab and Othman (2012): This study explored the efficacy of PRP versus corticosteroid injections in treating chronic plantar fasciitis. Results suggested that PRP might be more effective in the long term, reducing pain and increasing function (8).
- Aksahin et al. (2012): The researchers compared the effects of PRP injections to corticosteroids in patients with plantar fasciitis. The findings indicated that PRP injections provided longer-lasting relief from symptoms compared to corticosteroids (9).
- Shetty et al. (2014): This study examined the long-term results of PRP injections in treating plantar fasciitis and found that PRP could be a promising treatment option for providing sustained symptom relief (10).
- Martinelli et al. (2013): These researchers focused on the use of PRP injections for chronic plantar fasciitis, indicating that PRP treatment could significantly reduce pain and improve heel function, supporting its use as a viable treatment alternative (11).
A Study That Compares PRP to Dextrose Prolotherapy
Prolotherapy is a regenerative treatment that involves injecting a solution into the body to stimulate healing in injured joints and connective tissues. It aims to trigger the body’s own healing processes by causing a small, controlled inflammation at the injury site. The most common injected solution is hypertonic dextrose.
Another study compared PRP to just dextrose prolotherapy – it was a very small study that showed that PRP improved the function in that patient more so than prolotherapy, though prolotherapy did help him out with the pain. So that is another option.
A patient should take from this that they need to see a doctor who knows all the different treatment options because most doctors already know steroid injections or surgery when these things come as the last resort.
Most people want to avoid surgery, which they should because it has a higher risk and more complications. And steroid injections can provide some short-term benefits, but not long-term benefits and don’t actually fix the underlying problem.
How Does a PRP Injection for Plantar Fasciitis Work?
Platelet-rich plasma is an increasingly common regenerative treatment option utilized in the treatment of common musculoskeletal injuries, including plantar fasciitis.
Here is a step-by-step explanation of how PRP is created:
Blood collection: A small amount of blood is drawn from the patient’s arm, similar to a routine blood test.

Centrifugation: The collected blood is placed in a centrifuge, a machine that spins the blood at high speeds. This process separates the blood components based on their density.

Separation of blood components: After centrifugation, the blood separates into three layers:
- Plasma (top layer): This is the lightest component and contains a high concentration of platelets.
- Buffy coat (middle layer): This thin layer contains most of the white blood cells and a high concentration of platelets.
- Red blood cells (bottom layer): The heaviest component, consisting mostly of red blood cells.
Extraction of concentrated platelets: The buffy coat, which is rich in platelets, is extracted from the other layers.
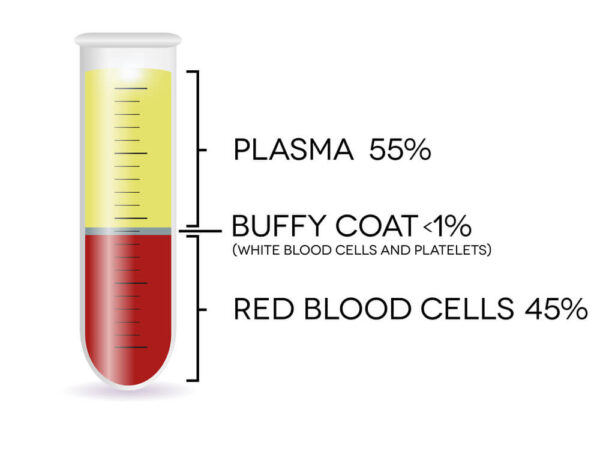
Platelets are rich in growth factors, as discussed in detail above. The growth factors promote tissue repair, improve blood flow, and reduce inflammation, which collectively can accelerate healing.
The PRP is then injected under ultrasound and X-ray guidance, which is essential for the following reasons:
- Accuracy: Ultrasound allows the clinician to visualize the exact placement of the needle in real-time. This precision is crucial for ensuring that the PRP is injected into the correct area, particularly in complex structures like the foot, where the plantar fascia is targeted in the treatment of plantar fasciitis.
- Safety: Ultrasound allows physicians to easily identify nerves, arteries, and other important structures that are avoided, thereby minimizing the risk of injury.
- Effectiveness: Accurate placement of the injection increases the effectiveness of the treatment. PRP needs to be delivered precisely into the area of tissue damage or inflammation for the best clinical results.
- Confirmation of delivery: Ultrasound and X-ray guide the injection process and confirm the accurate placement of the PRP.

What to Expect from PRP Injections for Plantar Fasciitis
Platelet-rich plasma (PRP) injections are an effective treatment option for patients who have failed conservative therapy for their plantar fasciitis.
Success Rates
- Effectiveness: PRP injections have been demonstrated to be effective in treating plantar fasciitis by promoting healing of the damaged fascia. The treatment involves injecting a concentration of the patient’s own platelets into the inflamed fascia area. Several studies have shown that PRP injections can reduce pain and improve function more effectively than steroid injections in the long term. For instance, a systematic review found PRP to be superior to corticosteroids in the medium-term to long-term management of symptoms.
- Longevity of results: Patients often experience a gradual improvement in symptoms, with significant relief typically noted several weeks after the injection. The benefits can last for up to a year or more, depending on individual healing processes and activity levels.
Side Effects
- Safety profile: PRP injections are generally safe, as they use the patient’s own blood, which minimizes the risk of allergic reactions or infections. However, as with any injection, there is a risk of infection, bleeding, nerve injury, or escalation in pain.
- Common side effects: The most common side effects include temporary increased pain at the injection site, swelling, and stiffness in the heel. These symptoms usually resolve within a few days.
Recovery – post-injection care
It’s often recommended to rest the foot and avoid high-impact activities for several weeks. Bracing is recommended when instability is present. Physical therapy is recommended to strengthen the foot muscles and improve flexibility, which can help in faster recovery and decrease the likelihood of recurrence.
Considerations
Response to PRP treatment can vary widely depending upon the severity of the plantar fasciitis, presence or absence of ankle/ foot instability, prior surgery, the patient’s overall health, medications, and adherence to post-injection care. Here are some important considerations to keep in mind:
- Pain management: Patients can expect a significant reduction in pain levels after receiving PRP injections. Initially, there might be a slight increase in discomfort due to the injection itself, but this typically subsides within a few days.
- Healing process: The PRP injections support and accelerate the body’s natural healing processes. Improvement in plantar fasciitis symptoms is often observed gradually over weeks to months as the damaged fascia begins to heal.
- Activity resumption: Post-PRP injection, patients are usually advised to gradually return to their normal activities. A specific timeline for this will depend on individual healing rates and the severity of the condition prior to treatment.
- Follow-up care: Follow-up visits may be necessary to monitor the healing progress and to determine if additional treatments are needed. The effectiveness of the PRP injection can vary, and in some cases, a series of injections may be recommended for optimal results.
- Lifestyle adjustments: To support the healing process and prevent future occurrences of plantar fasciitis, patients may need to make lifestyle and activity adjustments. This could include changes in footwear, incorporating foot exercises, and avoiding certain high-impact activities.
Get Effective, Targeted Treatment for Plantar Fasciitis
Plantar fasciitis is a painful medical condition characterized by pain in the heel and bottom of the foot. It occurs when the plantar fascia, the band of tissue that supports the arch of the foot, becomes inflamed, irritated, or injured. It is the most common cause of chronic heel pain affecting 10% of the population.
The most common symptoms include heel pain, pain with first steps, stiffness, and swelling. Plantar fasciitis is primarily an overuse injury. Risk factors for PF include obesity, heel spurs, excessive pronation, increasing age, and low back nerve irritation.
PRP involves the use of concentrated platelets, which contain important growth factors that can increase blood flow, reduce inflammation, and potentially accelerate healing.
Plantar fasciitis is a treatable condition. When conservative therapy fails to provide significant and sustained benefits, PRP is a viable treatment option allowing patients to use their own cells and avoid dependence on medications and the risks and complications associated with surgery.
Not all PRP injections are the same. At the Centeno-Schultz Clinic, board-certified, fellowship-trained physicians will review history, medications, and current imaging, along with a detailed physical examination and an ultrasound examination. A state-of-the-art cell laboratory at the Centeno-Schultz Clinic allows customized PRP for each patient, affording the best clinical results. All injections are performed under ultrasound and X-ray guidance, ensuring the PRP is delivered to the areas of injury.
Are you a Candidate?
John Schultz, MD
John R. Schultz M.D. is a national expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate and PRP for orthopedic injuries. He is board certified in Anesthesiology and Pain Medicine and underwent fellowship training. Dr. Schultz has extensive experience with same day as well as culture expanded bone marrow concentrate and sees patients at the CSC Broomfield, Colorado Clinic, as well the Regenexx Clinic in Grand Cayman. Dr. Schultz emphasis is on the evaluation and treatment of thoracic and cervical disc, facet, nerve, and ligament injuries including the non-surgical treatment of Craniocervical instability (CCI).
References
- Nahin RL. Prevalence and Pharmaceutical Treatment of Plantar Fasciitis in United States Adults. J Pain. 2018 Aug;19(8):885-896. doi: 10.1016/j.jpain.2018.03.003. Epub 2018 Mar 26. PMID: 29597082; PMCID: PMC6066406.
- LAPIDUS PW, GUIDOTTI FP. PAINFUL HEEL: REPORT OF 323 PATIENTS WITH 364 PAINFUL HEELS. Clin Orthop Relat Res. 1965 Mar-Apr;39:178-86. PMID: 14289759.
- Plantar fasciitis is primarily caused by repeated strain and micro-tears to the plantar fascia, the thick connective tissue that runs from the heel to the front of the foot
- Tahririan MA, Motififard M, Tahmasebi MN, Siavashi B. Plantar fasciitis. J Res Med Sci. 2012 Aug;17(8):799-804. PMID: 23798950; PMCID: PMC3687890.
- Cornwall MW, McPoil TG. Plantar fasciitis: etiology and treatment. J Orthop Sports Phys Ther. 1999 Dec;29(12):756-60. doi: 10.2519/jospt.1999.29.12.756. PMID: 10612073.
- Monteagudo M, de Albornoz PM, Gutierrez B, Tabuenca J, Álvarez I. Plantar fasciopathy: a current concepts review. EFORT Open Rev. 2018;3(8):485–93.
- Peerbooms JC, van Laar W, Faber F, Schuller HM, van der Hoeven H, Gosens T. Use of platelet-rich plasma to treat plantar fasciitis: design of a multi-centre randomized controlled trial. BMC Musculoskelet Disord. 2010;11:69.
- Ragab EM, Othman AM. Platelet-rich plasma for treatment of chronic plantar fasciitis. Arch Orthop Trauma Surg. 2012;132(8):1065–70.
- Aksahin E, Doğruyol D, Yüksel HY, Hapa O, Doğan O, Celebi L, Biçimoğlu A. The comparison of the effect of corticosteroids and platelet-rich plasma (PRP) for the treatment of plantar fasciitis. Arch Orthop Trauma Surg. 2012;132(6):781-785.
- Shetty VD, Dhillon M, Hegde C, Jagtap P, Shetty S. A study to compare the efficacy of corticosteroid therapy with platelet-rich plasma therapy in recalcitrant plantar fasciitis: a preliminary report. Foot Ankle Surg. 2014;20(1):10-13.
- Martinelli N, Marinozzi A, Carnì S, Trovato U, Bianchi A, Denaro V. Platelet-rich plasma injections for chronic plantar fasciitis. Int Orthop. 2013;37(5):839-842.
Am I a Candidate?
To answer this question, fill out the candidate form below to request a new patient evaluation, and a patient advocate will reach out to you to determine your next steps. Your one-hour, in-office or telemedicine evaluation will be with one of the world’s experts in the field of Interventional Orthopedics.