Our preferred Treatment for Baker’s Cyst is PRP
Learn MoreBaker’s Cysts
Popliteal cysts, more commonly known as Baker’s cysts, were named after the British surgeon William Morant Baker who first described them. About 38% of Baker’s cysts are routinely discovered on MRI in people who complain of knee pain (1). Capsular openings in the semimembranosus-gastrocnemius bursa are thought to give rise to Baker’s cysts.
We discuss all the details of Baker’s cysts in this post, including the common causes, symptoms, diagnosis method, treatment options, and complications. Keep reading to learn more!
What Is A Baker’s Cyst?
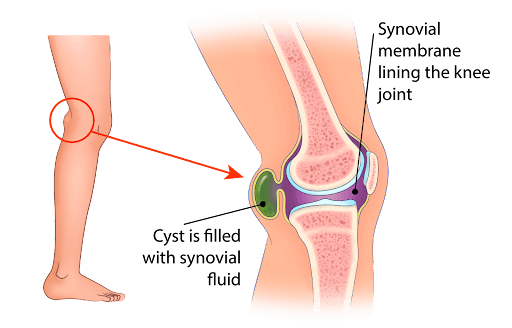
A Baker’s cyst, known medically as a popliteal or parameniscal cyst, is a painful or painless fluid-filled sac found in the posterior aspect of the knee. It is usually located between the semimembranosus tendon and the medial head of the gastrocnemius (back, inside part of the knee).
Symptoms Of A Baker’s Cyst
Here are some common symptoms that you may experience with a Baker’s cyst:
Swelling Behind The Knee
In 76% of patients with popliteal cysts, it is common to find swelling in the posterior aspect of the knee. This swelling may gradually increase in size, and the symptoms (and severity of symptoms) often increase in accordance with this change.
Swelling may decrease when the knee is flexed to 45 degrees, which is known as Foucher’s sign. This sign can also help differentiate popliteal cysts from other cysts in the knee.
Knee Pain
The pain from a Baker’s cyst can vary. However, larger cysts are usually accompanied by knee pain that worsens with activity. The pain is usually sharp and may be accompanied by a sensation of water running down the calf. If large enough can also cause numbness in your foot since your tibial nerve runs just lateral to this area.
An Inability To Fully Flex The Knee
The presence of a Baker’s cyst sometimes causes stiffness, preventing the full range of motion in the knee joint. As a result, a person with a popliteal cyst might be unable to fully flex or extend the knee. Too much fluid within the joint capsule can also cause knee stiffness and prevent movement.
Common Causes Of A Baker’s Cyst
In adults, Baker’s cysts can be caused by degenerative or acture conditions of the knee, such as degenerative meniscal tears. Here, the meniscus serves as a one-way valve that allows synovial fluid into but not out of the semimembranosus bursa as the injury progresses.
The synovial fluid localizes and consolidates into a viscous gel that leads to the formation of a Baker’s cyst.
Inflammatory conditions can also cause Baker’s cysts. These cysts can expand posteriorly due to the accumulation and extrusion of synovial fluid. They are usually located on the medial side of the popliteal fossa slightly below the crease of the posterior knee.
These cysts commonly arise in those with a history of trauma, degenerative joint disease like osteoarthritis, rheumatoid arthritis, infectious arthritis, or synovitis, or it may be an asymptomatic incidental finding on an MRI.
There are many other causes of Baker’s cysts. Some of the causes are listed below:
Osteoarthritis
In osteoarthritis, due to degeneration of the knee joint and the presence of inflammatory cells, the synovial lining produces excess joint fluid. Over time, this fluid can bulge into the popliteal space leading to the formation of a Baker’s cyst.
Rheumatoid Arthritis
Rheumatoid arthritis (RA) is a common chronic inflammatory autoimmune disease. It affects the knee joint in approximately 15% of RA patients (2).
In this condition, there is significant neutrophil (white cells) infiltration of the soft tissue along with hypertrophy of the joint capsule, synovium, tendon sheath, and bursa in the knee joint. This occurs due to chronic inflammation and can lead to a significant increase in the production of synovial fluid.
As the amount of synovial fluid increases, the joint capsule tightens. Over time, it localizes into a palpable mass behind the knee joint. This can expand between the semimembranosus and medial head of the gastrocnemius tendons, giving rise to a Baker’s cyst.
Knee Injury
Knee injuries, such as from an accident, a violent sporting tackle, or even a knee arthroplasty, can cause popliteal cyst formation. Depending on the type of injury, damage to the ligaments, menisci, or other structures in the knee may trigger the translocation of synovial cells or the extrusion of synovial fluid.
These collections of fluid may then accumulate, leading to the formation of a popliteal cyst.
Common Treatments For Baker’s Cysts
There are non-surgical (conservative), surgical, and regenerative therapies that can be used to treat popliteal cysts. However, Baker’s cysts are commonly first managed conservatively. Some of the common treatments for Baker’s cysts are listed below:
Pain Medications
Pain medications are a conservative, non-surgical treatment option for Baker’s cysts. Pain medications include non-steroidal anti-inflammatory medications (NSAIDs) like ibuprofen and celecoxib. There are also other types of pain medications such as opioids, but these have a high risk of drug dependence.
For mild pain, non-opioids like acetylsalicylic acid, paracetamol, and NSAIDs are commonly used. For mild to moderate pain, opioids like codeine, dihydrocodeine, tramadol, dextropropoxyphene are good options.
For those with moderate to severe pain, strong opioids like morphine, oxycodone, transdermal fentanyl, and transmucosal fentanyl are used. People with Baker’s cyst usually experience mild to moderate pain which can be effectively managed with NSAIDs.
Bandages
Bandages and wraps are another conservative, non-surgical treatment option for Baker’s cysts. Bandages and wraps can compress the swelling associated with Baker’s cysts. They can also prevent further worsening of the injury as the compression bandage encourages the fluid in the cyst to be reabsorbed more quickly.
Ice Packs
Cold therapy, or ice packs, is a conservative, non-surgical treatment for Baker’s cysts. They reduce the inflammation and fluid accumulation within the cyst. This decreases the size of the Baker’s cyst.
Draining The Cyst
Draining is a non-surgical treatment option for Baker’s cysts. Under ultrasound guidance, the physician can aspirate the fluid and drain the cyst with a needle. This is called needle aspiration. The procedure is done under local anesthesia. Once the Baker’s cyst is drained, the patient usually experiences immediate pain relief.
But if not addressing the underlying cause of the bakers cysts, it will likely return.
Surgery
Other surgical treatments for Baker’s cysts include debridement and excision surgeries.
In a debridement surgery, the cyst is opened and the cyst walls and septae are shaved down to allow the fluid to be reabsorbed. However, since there are vessels that could be injured during shaving, some surgeons prefer to excise or remove the cyst entirely.
This is done under general anesthesia via arthroscopy or open surgery. Arthroscopy is preferred as the bleeding and associated side effects are less when compared to open surgery. Once the cyst is removed, patients usually experience immediate relief from their symptoms.
Regenexx
Regenexx is a form of regenerative medicine therapy where we utilize your own body’s ortho-biologics to address not only the bakers cysts but also the underlying cause of the cyst – so it does not return.
In Regenexx, blood and/or bone marrow are taken from a person, we have a state of the art laboratory where these samples are processed. PRP (platelet-rich plasma) and BMC (bone marrow concentrate) are sent back to the physician who then injected into the damaged area via ultrasound and fluoroscopic guidance. To learn more about how we are different.
When To Seek Medical Help For Complications
While a Baker’s cyst can be managed conservatively, you must watch out for complications that point to an infection or escalation of the problem. If you see any of the following, then you must see a doctor immediately:
- Knee joint is warm to touch
- Chills or fever develop
- Redness or inflammation around the joint
- Severe calf pain
- Weakness of the ankle and foot
- Loss of sensation along the knee
- Weakness in the toes
Diagnostic Tests
To confirm the presence of a Baker’s cyst (and to ensure it is not getting worse), doctors may do the following tests:
- X-rays: To visualize a Baker’s cyst, the posteroanterior, lateral, and patellofemoral axial views are used. An x-ray is also useful to see loose bodies and highlight inflammatory and degenerative changes within the joint.
- Ultrasound: Ultrasound is now the go-to test for the initial assessment of a Baker’s cyst. It costs less, is non-invasive, and there is no radiation involved. The only disadvantage is that the accuracy depends on the skill of the operator.
Additionally, an ultrasound may not be able to differentiate between a Baker’s cyst and a meniscal cyst or myxoid tumor. An ultrasound may also not be able to identify what is causing the cyst. - MRI: MRI is the gold standard for the diagnosis of a Baker’s cyst. It also helps differentiate popliteal cysts from other conditions, such as meniscal tears, chondral defects, loose bodies, synovitis, osteoarthritis, and ligament tears if present.
The only disadvantage is the cost, which means ultrasound is the preferred screening modality for Baker’s cysts. - Arthrography: Direct arthrography was widely used to detect Baker’s popliteal cysts before the age of MRIs. In this imaging test, the doctor injects gas or an iodinated contrast medium into the intra-articular space of the knee.
The doctor then mobilizes the joint to force the contrast (or gas) into the cyst. After this, spot radiographs or fluoroscopy are used to detect the presence of contrast (or gas) in the popliteal cysts.
However, there are several disadvantages to arthrography. Namely, the use of ionizing radiation and contrast-related reactions. Radiation can increase the risk of cancer, and contrast-related reactions can damage the kidneys.
Moreover, it is classified as an invasive procedure because the contrast is injected into the joint, which can lead to complications like infections and bleeding. These are some of the reasons MRI is the preferred option nowadays.
The Prognosis For A Baker’s Cyst Is Good
Baker’s cysts have an incredibly good prognosis with timely management. They are mostly commonly treated conservatively with pain medications and arthroscopy.
However, regenerative medicine is another good option to treat any intra-articular pathology causing the cyst. If the cyst does not improve over time, then it may have to be surgically excised.
If you have a Baker’s cyst, talk to our board-certified doctors about the best treatments for your situation and if you are a good candidate for regenerative medicine.

Christopher J. Centeno, MD
Christopher J. Centeno, M.D. is an international expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate in orthopedics. He is board-certified in physical medicine and rehabilitation with a subspecialty of pain medicine through The American Board of Physical Medicine and Rehabilitation. Dr. Centeno is one of the few physicians in the world with extensive experience in the culture expansion of and clinical use of adult bone marrow concentrate to treat orthopedic injuries. His clinic incorporates a variety of revolutionary pain management techniques to bring its broad patient base relief and results. Dr. Centeno treats patients from all over the US who…
Read more
John Schultz, MD
John R. Schultz M.D. is a national expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate for orthopedic injuries. He is board certified in Anesthesiology and Pain Medicine and underwent fellowship training in both. Dr. Schultz has extensive experience with same day as well as culture expanded bone marrow concentrate and sees patients at the CSC Broomfield, Colorado Clinic, as well the Regenexx Clinic in Grand Cayman. Dr. Schultz emphasis is on the evaluation and treatment of thoracic and cervical disc, facet, nerve, and ligament injuries including the non-surgical treatment of Craniocervical instability (CCI). Dr. Schultz trained at George Washington School of…
Read more
John Pitts, M.D.
Dr. Pitts is originally from Chicago, IL but is a medical graduate of Vanderbilt School of Medicine in Nashville, TN. After Vanderbilt, he completed a residency in Physical Medicine and Rehabilitation (PM&R) at Emory University in Atlanta, GA. The focus of PM&R is the restoration of function and quality of life. In residency, he gained much experience in musculoskeletal medicine, rehabilitation, spine, and sports medicine along with some regenerative medicine. He also gained significant experience in fluoroscopically guided spinal procedures and peripheral injections. However, Dr. Pitts wanted to broaden his skills and treatment options beyond the current typical standards of care.
Read more
Jason Markle, D.O.
Post-residency, Dr. Markle was selected to the Interventional Orthopedic Fellowship program at the Centeno-Schultz Clinic. During his fellowship, he gained significant experience in the new field of Interventional Orthopedics and regenerative medicine, honing his skills in advanced injection techniques into the spine and joints treating patients with autologous, bone marrow concentrate and platelet solutions. Dr. Markle then accepted a full-time attending physician position at the Centeno-Schultz Clinic, where he both treats patients and trains Interventional Orthopedics fellows. Dr. Markle is an active member of the Interventional Orthopedic Foundation and serves as a course instructor, where he trains physicians from around the world.
Read more
Brandon T. Money, D.O., M.S.
Dr. Money is an Indiana native who now proudly calls Colorado home. He attended medical school at Kansas City University and then returned to Indiana to complete a Physical Medicine and Rehabilitation residency program at Indiana University, where he was trained on non-surgical methods to improve health and function as well as rehabilitative care following trauma, stroke, spinal cord injury, brain injury, etc. Dr. Money has been following the ideology behind Centeno-Schultz Clinic and Regenexx since he was in medical school, as he believed there had to be a better way to care for patients than the status quo. The human body has incredible healing capabilities…
Read moreAre you a Candidate?
More Resources for Baker’s Cysts
-
Partial ACL Tear
A partial ACL (anterior cruciate ligament) tear occurs when the ligament in the knee is partially damaged, often leading to instability, pain, and limited range of motion. This injury typically results from sudden stops, pivots, or direct impacts, commonly seen in athletes. Early diagnosis and appropriate management are crucial to preventing further damage and ensuring…
-
Degenerating Meniscus
Degenerating meniscus is a common issue, particularly in aging populations, that can lead to significant knee pain and impaired mobility. This condition often arises from wear and tear over time, resulting in the breakdown of the meniscal cartilage, which is crucial in cushioning and stabilizing the knee joint. Early detection and appropriate management are key…
-
Spinal Fusion Recovery: What to Expect
Navigating spinal fusion recovery can be a daunting prospect, given its impact on daily life and mobility. Understanding what to expect during this process is crucial for individuals undergoing this procedure. In this article, we’ll explore the typical timeline, challenges, and strategies for managing recovery after spinal fusion surgery, providing insights to help individuals prepare…
-
8 Golfer’s Elbow Exercises That Can Ease Your Symptoms
One of the main treatment options for a golfer’s elbow is physical therapy combined with a home exercise program. It involves specific golfer’s elbow exercises that will ease the symptoms of pain, weakness, and stiffness of the elbow. You can read more about what causes Medial Epicondylitis, aka golfer’s elbow or common flexor tendinosis, and…
-
What Is Golfer’s Knee, And What Can I Do About It?
The nature of golf is such that both the backswing and downswing affect the knee. The entire swing takes a little over one second. However, it can exert a force of 4 times the body weight on the front knee and 3 times the weight on the back knee (1). This makes knee injuries just as…
-
10 Best Shoulder Physical Therapy Exercises to Ease the Pain
Physical therapists often recommend specific exercises to alleviate shoulder pain, recognizing their effectiveness in both treating and preventing shoulder issues. These exercises, designed to enhance strength, flexibility, and mobility, can be a key component of a pain management strategy. Moreover, the ability to perform these exercises at home makes them a convenient option for patients…
References
- Sansone V, De Ponti A, Minio Paluello G, Del Maschio A. Popliteal cysts, and associated disorders of the knee: critical review with MR imaging. Int Orthop. 1995; 19:275-279.
- Chalmers P. N., Sherman S. L., Raphael B. S., Su E. P. Rheumatoid synovectomy: does the surgical approach matter? Clinical Orthopaedics and Related Research. 2011;469(7):2062–2071. doi: 10.1007/s11999-010-1744-3