MCL Sprain: Causes, Symptoms, Treatments, & Other Resources
An MCL (medial collateral ligament) sprain is a common knee injury that often affects athletes and other active individuals. It occurs when the ligament on the inner part of the knee is overstretched or torn, leading to pain, swelling, and difficulty in moving.
This guide aims to provide comprehensive information on the causes, symptoms, and effective treatments for MCL sprains.
What Is the MCL?
Ligaments are thick pieces of connective tissue that connect bone to bone.
The medial collateral ligament (MCL) is a thick, powerful band of connective tissue on the inside portion of your knee. It connects the thigh bone (femur) to the shin bone (tibia).
The MCL provides support and stability for the inside (medial) aspect of the knee. It is essential for stabilizing the knee against lateral forces that can push the knee inward, which is particularly important during activities involving twisting, turning, or direct impact.
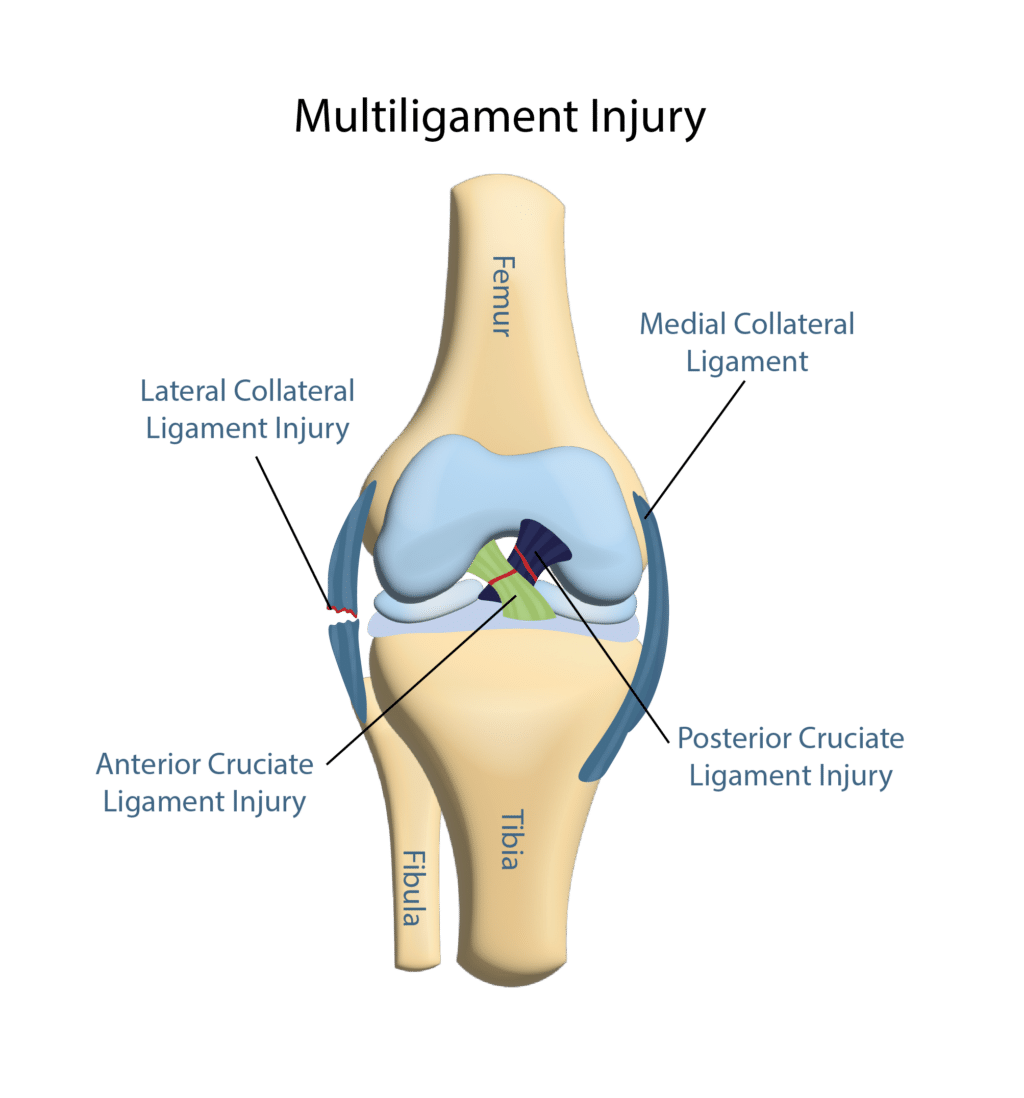
It works along the lateral collateral ligament (LCL), anterior cruciate ligament (ACL), and posterior cruciate ligament (PCL) to bring stability, structure, and movement to the knee.
What Is an MCL Sprain?
The medial collateral ligament is the most common knee ligament to be injured during knee trauma (3). The annual incidence of MCL injury has been reported as 0.24-7.3 per 1,000 people with a male to female ratio of 2:1 (4).
An MCL sprain is an injury to the medial collateral ligament. It occurs when the ligament is stretched or torn, which can happen due to a forceful blow to the outside of the knee or through twisting, bending, or a quick change in direction. The severity of an MCL sprain can vary and is typically classified into three grades, which are discussed below.
Grade Categorization of MCL Sprains
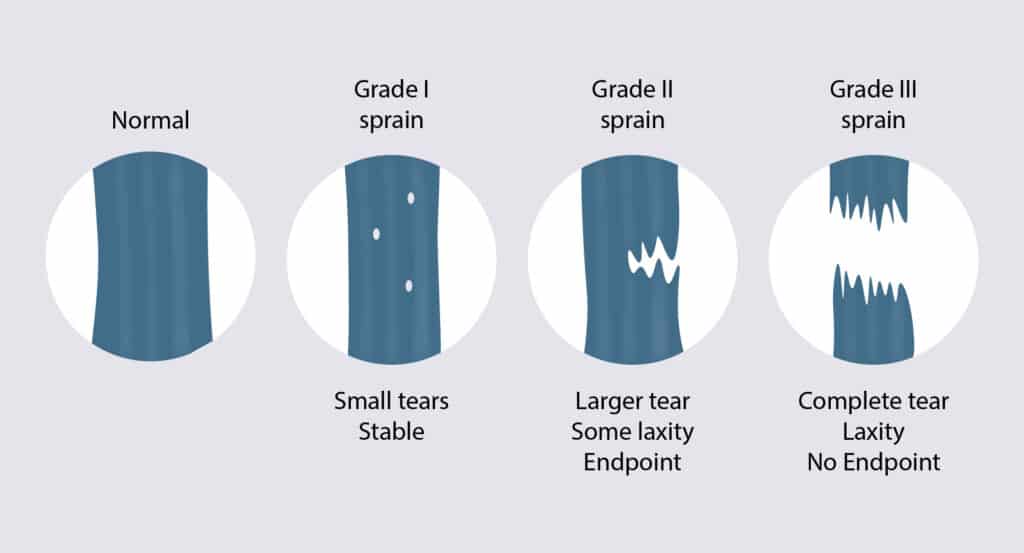
MCL sprains are categorized into three grades based on their severity, each reflecting the extent of damage to the medial collateral ligament in the knee (5).
Grade 1 Sprains
A grade 1 sprain involves injury to a few fibers, with local tenderness but without knee instability. On ultrasound or MRI, a portion of the MCL would be injured, but the remaining fibers would be normal.
Grade 2 Sprain
A grade 2 MCL sprain is a more significant injury as it involves partial tearing of the MCL. The tear may be partial thickness or near complete. Mild knee instability is common. These types of tears can typically be treated with ultrasound-guided platelet-rich plasma (PRP) or bone marrow concentrate.
Grade 3 Tears
A grade 3 MCL tear is the most severe form of medial collateral ligament injury, characterized by a complete rupture of the ligament. This level of injury results in significant instability in the knee, often accompanied by intense pain and swelling, and requires surgery.
Symptoms of MCL Sprains
Symptoms of MCL sprains can vary depending on the severity of the injury. The most common symptoms include:
Knee Pain
The MCL provides support and stability for the inside (medial) aspect of the knee. Injuries to the MCL can lead to a range of pain symptoms affecting various aspects of knee function and stability. The most common pain patterns are described below.
Medial Knee Pain
The most common site of knee pain in patients with MCL tears is the inside of the knee, directly over the medial collateral ligament. This area may feel tender to the touch and typically exhibits pain due to the MCL’s location and function in stabilizing the inner aspect of the knee.
Pain Behind Knee
Pain behind the knee from an MCL sprain can occur because the injury affects how you move, putting extra strain on other parts of the knee. When the MCL is injured, other areas of the knee might have to work harder to keep you stable, which can cause pain in the back of the knee.
- Back of knee swollen: Swelling at the back of the knee from an MCL injury can occur because the injury disrupts the normal balance and function of the knee, causing fluid to build up in response. This swelling is often your body’s way of reacting to the injury.
- Back of knee tight: Tightness at the back of the knee from an MCL injury can happen because the knee isn’t moving as smoothly as it should. When the MCL is injured, it can cause the whole knee to work differently to try to protect the injured area, leading to feelings of tightness. This tightness is your knee’s way of trying to stabilize itself, but it can make the knee feel stiff and less flexible.
Burning Pain When Kneeling
Burning pain when kneeling can happen if there’s irritation or pressure on the nerves or tissues around your knee. When you kneel, you put more stress on your knee, which can aggravate any existing issues or injuries, leading to a burning sensation. This type of pain is a signal that something in the knee might be inflamed or not working properly.
Pain When Bending and Straightening
Pain when bending and straightening the knee with an MCL injury occurs because the ligament is damaged and isn’t able to function normally. When you move your knee, the injured MCL might struggle to keep the joint stable, leading to pain as it stretches or moves incorrectly.
This movement can irritate the injured area further, causing discomfort each time you bend or straighten your knee.
Knee Buckling
Knee buckling with an MCL injury happens because the ligament, which helps stabilize the inner side of the knee, is weakened or torn. This means it can’t properly support the knee when you make certain movements, like walking or turning. As a result, the knee might suddenly give way or buckle under your weight, making it feel unstable.
Knee Locking & Catching
Knees can bend forward and back, as well as rotate slightly. When a knee is unable to execute these actions, it impairs mobility and the capacity to complete daily activities such as sitting, standing, squatting, or kneeling.
A locked knee occurs when a knee cannot be bent or straightened, so it gets stuck or feels locked in a certain position for an extended period. There are two forms of locked knees: one is the inability to move because of an actual physical or mechanical restriction, and the other feels locked because of the pain involved in moving it.
When a person has their knee joint effectively frozen into place and cannot move, this is known as a true locked knee.
Knee Popping
Knee popping can be a sensation that something is moving around in the knee. There may also be an audible sound associated with the popping, which in medical terms is called crepitus.
This can also cause what we call mechanical catching or locking, which may make the knee feel like it is stuck in an extended or flexed position, and you have to move it in certain ways to get out of that.
This knee popping sensation or sound could be a very simple issue or it could be a sign that more serious damage is going on in the knee, so determining what is causing it is very important.
Reduced Range of Motion in Knees
A knee can feel stiff if there is some swelling in or around the joint, or muscle tightness, which can cause restricted motion. This can occur from a problem in the knee joint, such as inflammation, arthritis, infection, or an injury. The distance and direction that a joint may move are referred to as its range of motion.
Various joints in the human body have specific normal ranges as measured by doctors and therapists. One study, for example, found that a normal knee should be able to bend to between 133 and 153 degrees. A typical knee should also be able to extend fully straight.
Limitation of motion occurs when a person’s range of motion in any limb is reduced below the normal range.
Causes of MCL Sprains
MCL sprains are common injuries in sports such as football, hockey, and skiing. The ligament can be stretched or even torn due to direct blows, but it usually happens when you hit the outer aspect of your knee at high speeds. Other causes could include:
- repeated stress on the joint without adequate time for healing
- abrupt change in direction or speed
- a sudden contraction of muscles with influential force.
Like other tears to knee ligaments, a doctor will ask you about your symptoms and then perform a physical examination. They may also order some tests, such as an MRI or an X-ray, to help diagnose the sprain.
An in-office ultrasound is an effective imaging modality to evaluate the presence and severity of an MCL tear or sprain. An additional advantage is that it does not require pre-authorization or a separate appointment.
Home Remedies for MCL Sprains
While consulting a doctor for an MCL sprain is crucial, there are several home remedies that can aid in the healing process and provide relief. These remedies focus on reducing swelling, alleviating pain, and improving knee functionality.
Remember, these should be used in conjunction with professional medical advice:
- Rest the knee. This is one of the most important things that you can do when you have an MCL sprain. Taking a break from strenuous activities will help the knee heal.
- Use heat, which promotes increased blood flow to the area.
- Fish oil and turmeric can help with the swelling and pain.
- Avoid the use of ice as it restricts blood flow and can limit inflammation. Inflammation is the first step in healing.
Treatment Options for MCL Sprain
An MCL sprain is a common knee injury that can vary in severity from mild to severe, affecting the stability of the knee joint. Most MCL injuries can be treated nonoperatively (1).
Even though the MCL can spontaneously heal with no additional treatment, the healing that takes place is typically incomplete (2), which can increase the risk of re-injuring the ligament over time. Treatment options for MCL sprains typically focus on reducing pain and swelling, restoring normal knee function, and preventing future injuries.
The most common treatment options include:
NSAIDs
NSAIDs are powerful anti-inflammatory drugs that are used to reduce inflammation and pain. Common examples include Ibuprofen, Naproxen, Diclofenac, and Celecoxib. These medications have significant adverse side effects and, for this reason, should be avoided.
Physical Therapy
Physical therapy is key in the rehabilitation of MCL injuries. Through a tailored regimen of exercises, physical therapy helps improve flexibility and stabilize the knee by strengthening the muscles around the joint. It also focuses on correcting biomechanical imbalances that could contribute to injury risk.
Bracing the Knee
Bracing plays a key role in the management of MCL injuries, providing essential support and stabilization to the injured knee. By restricting unnecessary movements that could aggravate the injury, braces help to prevent further damage while the MCL heals. Knee braces aid in maintaining proper knee alignment during rehabilitation.
Knee Ligament Surgery
Surgery for MCL tears is generally not the first line of treatment, as many MCL injuries can heal effectively with non-surgical methods such as bracing, physical therapy, and rest. Most isolated tears (grades 1 and 2) usually respond well to conservative treatment.
Surgery may be considered in certain cases, which include:
- Severe tear (grade 3)
- Moderate tears that do not heal with conservative treatment
- Multi-ligament injury. The ACL is the most common ligament injured with an MCL sprain.
- Bone avulsion (the ligament along with a bone fragment is torn away from the bone)
Is MCL Surgery a Good Option?
MCL surgery involves repairing or reconstructing the torn ligament to restore stability and function to the knee joint. Post-surgery, patients often undergo a rehabilitation program that includes physical therapy to help regain strength and mobility.
Knee surgery is associated with risks. The most common risks associated with MCL surgery include (6):
- Bleeding
- Infection
- Blood clots (DVT)
- Nerve and blood vessel damage
- Scar tissue formation
- Knee instability
PRP for MCL Tears & Sprains
PRP (platelet-rich plasma) is an increasingly popular treatment option used in various musculoskeletal injuries, including MCL sprains.
What Is PRP?
PRP involves concentrating platelets from the patient’s own blood. Blood typically contains about 6% platelets, whereas PRP involves a concentration of 94% platelets.
The Process:
- Blood collection: A small amount of blood is drawn from the patient.
- Centrifugation: The blood is then placed in a centrifuge, where it is spun to separate out the different components: red blood cells, platelets, and plasma.
- Extraction: The platelet-rich portion of the plasma is extracted.
- Injection: The concentrated platelets are then injected under ultrasound guidance into the injured area to stimulate and enhance healing.
PRP treatment aids in MCL sprains by:
- Enhancing healing: The concentrated platelets in PRP release growth factors that stimulate the repair and regeneration of tissue at the injury site. Growth factors and other molecules, which play various roles in tissue repair, pain modulation, and other functions, are contained within the alpha granules of platelets. A few key factors involved in tissue repair are transforming growth factor-beta 1 (TGF-B1), insulin-like growth factor (IGF), and thrombospondin-1 (7).
- Reducing inflammation: PRP can alter inflammatory processes around the injury, reducing pain and swelling.
- Accelerating recovery: By improving the healing environment within the knee, PRP can shorten the overall recovery time, enabling a quicker return to activity.
Recent studies have demonstrated that PRP in the treatment of MCL sprains reduces the recovery period and pain and improves function (8).
Relieve Yourself Safely from MCL Sprain
The medial collateral ligament (MCL) is a thick band of connective tissue on the inside portion of your knee. It connects the thigh bone (femur) to the shin bone (tibia). The MCL provides support and stability for the inside (medial) aspect of the knee.
An MCL sprain involves the stretching or tearing of the ligament on the inner part of the knee, which is crucial for stabilizing the joint against sideways movements. These injuries, categorized from mild grade 1 to severe grade 3 sprains, often occur during activities that involve sudden changes in direction or impact.
Common symptoms vary by severity but generally include pain, swelling, and instability in the knee, with severe cases potentially leading to knee buckling or locking.
For treating MCL sprains, especially grades 1 and 2, non-surgical methods such as physical therapy, bracing, and rest are usually effective. Grade 3 injuries require surgical repair.
For MCL sprains that do not respond adequately to conservative treatments such as rest, bracing, or physical therapy, PRP therapy is an effective treatment option. It utilizes a concentration of platelets from the patient’s own blood that is much higher than normal.
These platelets release growth factors that stimulate tissue repair and regeneration at the site of injury. Injecting this platelet-rich plasma directly into the affected area under ultrasound guidance can help reduce inflammation, alleviate pain, and accelerate the healing process.
PRP avoids the risks and complications associated with surgery and in most cases allows patients a quicker return to normal activities.
Consider a telemedicine or in-office consultation at the Centeno-Schultz Clinic where a board-certified, fellowship-trained physician can discuss your regenerative treatment options.
Are You a Candidate?
John Schultz, MD
John R. Schultz M.D. is a national expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate and PRP for orthopedic injuries. He is board certified in Anesthesiology and Pain Medicine and underwent fellowship training. Dr. Schultz has extensive experience with same day as well as culture expanded bone marrow concentrate and sees patients at the CSC Broomfield, Colorado Clinic, as well the Regenexx Clinic in Grand Cayman. Dr. Schultz emphasis is on the evaluation and treatment of thoracic and cervical disc, facet, nerve, and ligament injuries including the non-surgical treatment of Craniocervical instability (CCI).
Other Resources for MCL Sprains
Free Download: The Knee Owner’s Manual
This e-book by Dr. Chris Centeno examines the knee and its role in the human musculoskeletal system and the body as a whole. The Knee Owner’s Manual provides a series of tests and clearly defined exercises that you can perform on your own to assess and monitor your own knee health. It will allow you to look for trouble spots where your own body may be having difficulty with stability, articulation, symmetry, and neuromuscular function. You’ll be able to see how these deficits in other regions of the body relate to the knee.
The Knee Owner’s Manual also discusses how Regenexx is pioneering the development of interventional orthopedics, a new branch of medicine that employs regenerative biologic therapies such as adult bone marrow concentrate and platelet-rich plasma to help repair and strengthen damaged tissues in other areas of the body.
This is contrasted with invasive knee surgeries, which often remove important tissues or replace the entire knee itself when it becomes damaged. With hyperlinks to more detailed information, related studies, and commentary, this book condenses a vast amount of data, images, and resources into an enjoyable and informative read. This is the first edition of The Knee Owner’s Manual, a companion book to Orthopedics 2.0.
-
What Is Golfer’s Knee, And What Can I Do About It?
The nature of golf is such that both the backswing and downswing affect the knee. The entire swing takes a little over one second. However, it can exert a force of 4 times the body weight on the front knee and 3 times the weight on the back knee (1). This makes knee injuries just as…
-
Regenexx ACL Repair vs Reconstruction Surgery for Knee ACL
Regenexx ACL Repair vs Reconstruction Surgery for Knee ACL Today I’d like to highlight a patient named Joe’s story. Joe is unique in that he has had the non-surgical Regenexx Perc-ACLR procedure which uses your own cells injected via a small needle, and a surgical ACL reconstruction, so he can compare the two. So let’s…
References:
- Shelbourne KD, Wilckens JH, Mollabashy A, DeCarlo M. Arthrofibrosis in acute anterior cruciate ligament reconstruction. The effect of timing of reconstruction and rehabilitation. Am J Sports Med. 1991;19(4):332‐336. doi:10.1177/036354659101900402
- Wan C, Hao Z, Wen S. The effect of healing in the medial collateral ligament of human knee joint: A three-dimensional finite element analysis. Proc Inst Mech Eng H. 2016;230(9):867‐875. doi:10.1177/0954411916656662
- Memarzadeh A, Melton J. Medial collateral ligament of the knee: anatomy, management and surgical techniques for reconstruction. Orthopaedics and Trauma. 2019;33(2):91–9
- DeLong JM, Waterman BR. Surgical Techniques for the Reconstruction of Medial Collateral Ligament and Posteromedial Corner Injuries of the Knee: A Systematic Review. Arthroscopy. 2015 Nov;31(11):2258-72.e1. doi: 10.1016/j.arthro.2015.05.011. Epub 2015 Jul 17. PMID: 26194939.
- Makhmalbaf H, Shahpari O. Medial Collateral Ligament Injury; A New Classification Based on MRI and Clinical Findings. A Guide for Patient Selection and Early Surgical Intervention. Arch Bone Jt Surg. 2018 Jan;6(1):3-7. PMID: 29430488; PMCID: PMC5799597.
- Rodríguez-Merchán EC, De la Corte-Rodríguez H, Encinas-Ullán CA, Gómez-Cardero P. Complications of surgical reconstruction of multiligament injuries of the knee joint: diagnosis, prevention and treatment. EFORT Open Rev. 2021 Oct 19;6(10):973-981. doi: 10.1302/2058-5241.6.210057. PMID: 34760296; PMCID: PMC8559571.
- Leitner GC, Gruber R, Neumüller J, Wagner A, Kloimstein P, Höcker P, Körmöczi GF, Buchta C. Platelet content and growth factor release in platelet-rich plasma: a comparison of four different systems. Vox Sang. 2006 Aug;91(2):135-9. doi: 10.1111/j.1423-0410.2006.00815.x. PMID: 16907874.
- Bagwell MS, Wilk KE, Colberg RE, Dugas JR. THE USE OF SERIAL PLATELET RICH PLASMA INJECTIONS WITH EARLY REHABILITATION TO EXPEDITE GRADE III MEDIAL COLLATERAL LIGAMENT INJURY IN A PROFESSIONAL ATHLETE: A CASE REPORT. Int J Sports Phys Ther. 2018 Jun;13(3):520-525. PMID: 30038838; PMCID: PMC6044600.