Anterior Longitudinal Ligament Injury Treatments
Am I a Candidate?The anterior longitudinal ligament (ALL) is a strong neck stabilizer in the front of the cervical spine. It can be injured through trauma such as whiplash. Early diagnosis and treatment are key to avoiding long-term consequences related to ALL damage.
An Overview of Anterior Longitudinal Ligament (ALL) Injuries
The ALL is a wide ligament that runs down the front of the spine. Its function is to support the front part of the intervertebral disks and prevent excessive extension of the spine. It can be injured with an excessive hyperextension-type force such as with a car accident, a fall on the front of the head, or a blow to the head.
If the ALL is injured it can lead to excess stress on the back of the neck such as on the facet joints and posterior disks. Symptoms can vary from person to person, depending on which areas are becoming irritated and the severity of the damage to the ligament.
Common symptoms are pain in the back of the neck, stiffness, and spasms in the neck and shoulder, headache, pain, numbness or tingling in the arm(s), lightheadedness, and dizziness, etc. Symptoms are typically worse when looking upward.
There are three classifications of ligament injuries:
- Grade 1: Mild stretching or small partial tear of the ligament, less than 50% of the width.
- Grade 2: Moderate ligament injury with tearing of greater than 50% of the ligament fibers.
- Grade 3: Complete tear of the ligament. Complete tears can be non-retracted, meaning the fibers of the ligament are still approximated with each other. Complete retracted tears refer to ligament fibers that are completely torn apart.
Adapting Treatment to Injury Severity
The treatment of ALL injuries depends on the severity of the injury and what other structures may be injured as well.
- For grade 1 injuries, conservative care is all that is typically needed.
- For grade 2 injuries and grade 1 injuries that don’t fully heal, minimally invasive procedures can be used to help further stimulate repair.
- For grade 3 injuries, surgery is often required.
Quick At-Home Remedies for Mild ALL Injuries
While seeking professional medical advice is crucial, there are also some remedies you can try in the comfort of your own home to help with the recovery process.
- Rest
Limit activities that cause pain, such as neck extension. You generally do not want total bed rest or to stop moving your neck altogether, but just limit some of the motions and move the neck more slowly. - Ice or heat application
Ice may help to reduce any swelling and temporarily help painful areas. You only want to ice for a few minutes at a time, as excess icing can reduce blood flow, which is needed for healing.
Heat therapy, especially infrared heat, can help with pain, relax tight muscles around the neck, and promote blood flow. Be careful when using regular heating pads to not allow them to get too hot and not to leave them on an area too long as they can cause skin burns. - Activity modification
Modify activities to avoid heavy strain on the neck. No rapid neck movements, high-intensity training, or contact sports. - Stretching
Gentle stretching and mobilization of the neck can help maintain normal joint motion, which is good for joint health. Stretching can help relax tight muscles as well.
Pain Medications
When it comes to anterior longitudinal ligament injuries, there are pain medications available as an option for treatment when home remedies fail to provide relief.
- Non-prescription and prescription medications
Over-the-counter pain relievers such as Tylenol and anti-inflammatory medications such as Ibuprofen, Aleve, etc, may help manage pain and reduce inflammation. Sometimes strong pain medications can be prescribed by a doctor for more severe pain.
Non-steroidal anti-inflammatory drugs (NSAIDs) may help relieve pain but have many potential side effects so their use should be modest. Potential side effects include stomach upset, gastrointestinal bleeding, kidney or liver problems, increased risks for heart attack or stroke, and inhibiting the healing process.
Oral steroids are sometimes prescribed for severe inflammation but should rarely if ever be used for most musculoskeletal issues unless there is spinal cord damage. Steroids have even more risks than NSAIDs, including bone loss, altering hormone function, altering sugar levels, causing weight gain, temporary psychosis, and inhibiting healing.
Narcotic pain medications are sometimes used for severe pain. These, of course, have many risks such as addiction, lethargy, constipation, respiratory depression, impaired cognition, and actually increasing pain. - Pain injections
The ALL can sometimes hurt directly, but most of the time it causes pain in the neck joints or neck disks or causes irritation to the nerves.
For joint pain, these joints can be injected with a local anesthetic and steroids to help pain and reduce joint inflammation. This can serve diagnostic purposes and may help relieve pain for weeks to months. Of course, this is just a temporary help, it doesn’t address the damaged ALL, and steroids have many risks, as stated above.
Also for joint pain, the nerves that innervate the joints (medial branches) can be blocked with local anesthetic in a procedure called an MBB. This would help to diagnose facet joint pain and, if helpful for a few hours, a radio frequency ablation (RFA) can be performed. An RFA burns the nerves that innervate the joints, so it may help with pain for 6-12 months at a time.
The negatives of this are, of course, that this is still a temporary pain reliever only, it does not address the damaged ALL, and those nerves also control the neck stabilizing muscles so those muscles will get weaker and smaller (atrophy), leading to more neck instability.
For nerve pain, local anesthetic and/or steroids can be injected around the nerves in an epidural injection. Again, this can be used for diagnostic purposes and temporary pain relief but does not address the ALL injury and has all the steroid risks.
Physical Therapy and Orthotic Devices
When it comes to individuals with ALL injuries, there are various approaches to consider for rehabilitation. Physical therapy and orthotic devices play a crucial role in aiding recovery and improving quality of life.
- Physical therapy (PT)
Physical therapy is a very important treatment tool for ALL injuries. Good physical therapy should help to address poor neck and shoulder posture, help maintain or improve range of motion and neck mobility, and can help to build or maintain neck strength. Also, PT has modalities that can be used for muscle relaxation, pain relief, etc. All of these can help to facilitate the natural healing process, as they can help take extra stress off the ALL and the neck, support recovery, and reduce the risk of more injury. - Bracing
A cervical neck brace, soft or hard, can be used for moderate to severe ALL ligament injuries where there is a lot of neck instability. A brace can limit the motion of the neck to allow ligament healing and reduce the risk of further damage.
However, one has to weigh the risk of lack of motion causing muscle atrophy and neck stiffness, which would in the long term make the neck worse and less functional.
Thus, bracing should only be done for a very short period of time, a few days, or just as needed for an hour or so throughout the day if doing something with a higher risk of unpredictable neck movements such as driving on a bumpy road.
Surgical Interventions
Surgery should only be considered in the most severe ALL ligament injuries that have failed other conservative treatments. Surgery would be also indicated if the ALL ligament injury led to spinal cord injury or nerve damage, in which case you would go directly to surgery.
Anterior Fusion
Anterior fusion is the most common surgery for severe ALL injuries. The specific surgery could be an anterior cervical discectomy and fusion (ACDF) or anterior cervical corpectomy and fusion (ACCF).
In these surgeries, an incision is made in the front of the neck, important structures are moved to avoid damage and the surgery is performed. Any excess bone spurs that could be pinching nerves can be removed (decompression), parts or all of the disk may be removed and the front of the neck bone fused together with a plate and screws to keep that segment stable.
Anterior Longitudinal Ligament Reconstruction
This surgery is usually only performed if the ALL is damaged, there is an artificial disk and that segment is unstable. In this surgery, the ALL is repaired using an allograft (typically a ligament from a cadaver or a synthetic ligament).
Posterior Decompression and Fusion
Rarely, a posterior neck fusion would be performed. This is where the surgery is done from the back of the neck. The surgeon would remove any bone spurs causing nerve compression and fuse the joints and or vertebral bodies with screws. This would be considered if an upper neck ALL injury occurred that led to severe craniocervical instability or severe joint damage.
Are Surgical and Invasive Procedures the Only Options?
Fusion surgery works well in many people, but all surgeries have considerable risks, including bleeding, infection, permanent nerve injuries, stroke, and death. Also, fusion leads to a lack of mobility at that level, leading to excess stress on the levels above and below the fusion.
The excess stress at other levels can cause damage and pain to the disks, nerves, and joints, and this is called adjacent segment disease. This typically may require more treatments and possibly more surgery in the future. Given these substantial risks of invasive treatment, are there ways to avoid these major risks and repair damaged ALLs?
At the Centeno-Schultz Clinic, we have pioneered minimally invasive procedures that help the ALL heal with far less risk than any surgery, have no adverse medication risks, and actually address the underlying issue.
The Centeno-Schultz Clinic Protocol for ALL Injuries
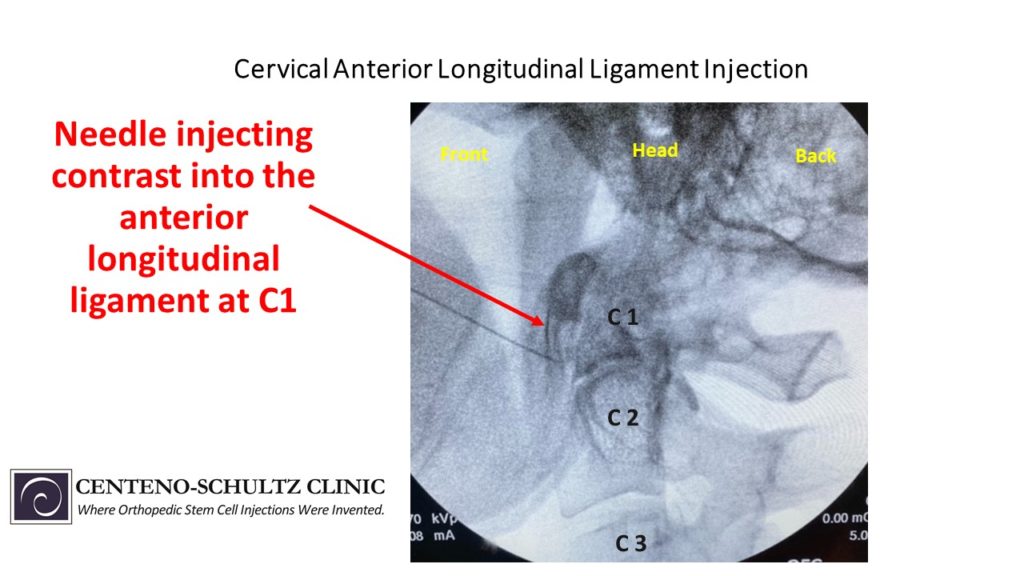
In 2005, we were the first clinic in the world to inject stem cells for orthopedic problems. Since that time we have been researching and pioneering regenerative injection procedures for orthopedic injuries. We inject orthobiologics, substances that stimulate self-healing in damaged tissues.
Here, we discuss the common orthobiologics that could be used for ALL injuries. We also pioneered an injection protocol to safely and accurately target the ALL at each level of the neck.
Prolotherapy
Prolotherapy is the injection of an irritant solution that causes small damage to the tissue, thus initiating a healing response. The most common solution is a hypertonic dextrose solution. The healing response is small, so it often requires multiple treatments but can work very well for mild ligament and tendon injuries.
We often use this for damaged posterior neck ligaments such as the supraspinous and interspinous ligaments. We typically do not use prolotherapy directly to the ALL, however. This is because the ALL is close to a lot of blood vessels, so an inadvertent injection of prolotherapy into a blood vessel could lead to damage if that blood vessel supplies a nerve or the brain.
Platelet Rich Plasma (PRP) Injections
PRP is made by taking the patient’s own blood, centrifuging (spinning it) to separate the components, and concentrating the platelets. Platelets have growth factors, cytokines, proteins, exosomes, etc. that mediate a healing response. PRP can be injected into mild to moderately injured ligaments such as the ALL and damaged neck ligaments.
We use this often to treat ALL injuries. PRP can also be used to help heal and slow arthritis progression in cervical facet joints. PRP can be used to treat cervical disk tears that may cause pain or lead to nerve irritation as well.
Lastly, the specialized form of PRP we make in our lab, called platelet lysate, can be used to treat irritated nerves by reducing inflammation and delivering healing growth factors for that nerve to repair itself.
Bone Marrow Aspirate Concentrate (BMAC)
BMAC contains stem cells as well as many other cells that can be powerful healing cells. Similarly to PRP, bone marrow can be collected, spun down, and concentrated then injected into the patient’s damaged tissue as well.
BMAC with stem cells is a more powerful healing agent and can be used for moderate to severe ligament and joint injuries. We use this often to treat ALL and other injured neck structures.
Find Relief with Effective ALL Injury Solutions
Damage to the anterior longitudinal ligament can be a major contributor to neck pain and cause damage to other structures. If conservative measures are not helping, then reach out to one of our board-certified musculoskeletal specialist physicians at the Centeno-Schultz Clinic for a thorough evaluation of your neck and ALL injuries.
We have created specialized reparative injections to treat the ALL and other injured neck structures with PRP and BMAC. These procedures can provide lasting relief and help you avoid the risks of drugs and invasive surgeries.
Schedule an in-person or telemedicine consultation with a musculoskeletal board-certified fellowship-trained physician and learn about your regenerative treatment options.
Take control of your spinal health. Schedule a consultation with our trusted specialists to find out what procedure is right for you.

Christopher J. Centeno, MD
Christopher J. Centeno, M.D. is an international expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate in orthopedics.
Dr. Centeno is one of the few physicians in the world with extensive experience in the culture expansion of and clinical use of adult bone marrow concentrate to treat orthopedic injuries. His clinic incorporates a variety of revolutionary pain management techniques to bring its broad patient base relief and results. Dr. Centeno treats patients from all over the US who travel to Colorado to undergo innovative, non-surgical treatments. Dr. Centeno has chaired multiple international research-based conferences. He also maintains an active research-based practice, with multiple publications listed in the US National Library of Medicine. Dr. Centeno has also served as editor-in-chief of a medical research journal dedicated to traumatic injury.
Dr. Centeno trained at the Baylor College of Medicine, Texas Medical Center, and the Institute for Rehabilitation Research. He hails from both Florida and New York and currently resides in Boulder, Colorado with his wife and three children.

John Schultz, MD
John R. Schultz M.D. is a national expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate for orthopedic injuries. He is board certified in Anesthesiology and Pain Medicine and underwent fellowship training in both. Dr. Schultz has extensive experience with same day as well as culture expanded bone marrow concentrate and sees patients at the CSC Broomfield, Colorado Clinic, as well the Regenexx Clinic in Grand Cayman. Dr. Schultz emphasis is on the evaluation and treatment of thoracic and cervical disc, facet, nerve, and ligament injuries including the non-surgical treatment of Craniocervical instability (CCI). Dr. Schultz trained at George Washington School of…
Read more
John Pitts, M.D.
Dr. Pitts is originally from Chicago, IL but is a medical graduate of Vanderbilt School of Medicine in Nashville, TN. After Vanderbilt, he completed a residency in Physical Medicine and Rehabilitation (PM&R) at Emory University in Atlanta, GA. The focus of PM&R is the restoration of function and quality of life. In residency, he gained much experience in musculoskeletal medicine, rehabilitation, spine, and sports medicine along with some regenerative medicine. He also gained significant experience in fluoroscopically guided spinal procedures and peripheral injections. However, Dr. Pitts wanted to broaden his skills and treatment options beyond the current typical standards of care.
Read more
Jason Markle, D.O.
Post-residency, Dr. Markle was selected to the Interventional Orthopedic Fellowship program at the Centeno-Schultz Clinic. During his fellowship, he gained significant experience in the new field of Interventional Orthopedics and regenerative medicine, honing his skills in advanced injection techniques into the spine and joints treating patients with autologous, bone marrow concentrate and platelet solutions. Dr. Markle then accepted a full-time attending physician position at the Centeno-Schultz Clinic, where he both treats patients and trains Interventional Orthopedics fellows. Dr. Markle is an active member of the Interventional Orthopedic Foundation and serves as a course instructor, where he trains physicians from around the world.
Read more
Brandon T. Money, D.O., M.S.
Dr. Money is an Indiana native who now proudly calls Colorado home. He attended medical school at Kansas City University and then returned to Indiana to complete a Physical Medicine and Rehabilitation residency program at Indiana University, where he was trained on non-surgical methods to improve health and function as well as rehabilitative care following trauma, stroke, spinal cord injury, brain injury, etc. Dr. Money has been following the ideology behind Centeno-Schultz Clinic and Regenexx since he was in medical school, as he believed there had to be a better way to care for patients than the status quo. The human body has incredible healing capabilities…
Read moreAm I a Candidate?
To answer this question, fill out the candidate form below to request a new patient evaluation, and a patient advocate will reach out to you to determine your next steps. Your one-hour, in-office or telemedicine evaluation will be with one of the world’s experts in the field of Interventional Orthopedics.