Spinal Stenosis
Causes, Symptoms, Non-Surgical Treatment, & Other Resources
Back pain can be disabling and can arise from many conditions such disc herniation, disc protrusion, and spinal stenosis. Today we’ll be concentrating on spinal stenosis. How is it treated? Is surgery needed? Are there alternatives to back surgery for spinal stenosis?
What Is Spinal Stenosis?
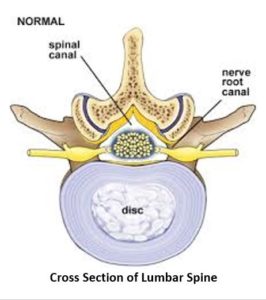
Lumbar stenosis is narrowing of the spinal canal and is sometimes referred to as central canal stenosis (1). The spinal canal is important as it is a hole that runs through the spinal bones from the top of the neck to your low back. It’s located directly behind each disc and contains the spinal cord, spinal fluid, and spinal nerves.
To better understand stenosis, please watch the video below on the neck stenosis. The same concepts apply to the low back.
What are the Causes of Spinal Stenosis?
The spinal canal is outlined by the red line. The disc is in front of the spinal canal whereas the ligamentum flavum and lumbar facet joints are behind the spinal canal. Any structure that pushes or extends beyond the red line can narrow the spinal canal thereby creating stenosis. (2)
There are three principles structures that can encroach upon the spinal canal thereby causing spinal stenosis: the disc, the facet joints and the ligamentum flavum
- Disc protrusion. The disc is in front of the spinal canal. A disc protrusion can extend into the spinal canal and narrow the diameter of the spinal canal creating stenosis as illustrated below by the blue arrow.
- Overgrowth the lumbar facets. The facet joints are behind the spinal canal and in the presence of trauma, overloading or instability can beef up in size and encroach on the spinal canal thereby causing spinal stenosis as illustrated by the green arrow
- The ligamentum flavum is in the back of the spinal canal and is a thick elastic tissue that connects the vertebral bodies. In the illustration below it is the thick yellow band that is identified by the two blue arrows. In the presence of instability, the ligamentum flavum can become thickened pushing forward on the spinal canal creating stenosis illustrated below by the purple arrow.
What are the Treatment Options?
Conservative treatment options include physical therapy (3), medications, lifestyle modifications, steroid injections, and rehabilitation. (4). When these treatment options fail many consider surgery. Current surgical options include:
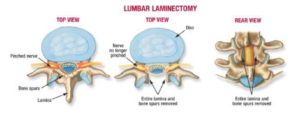
- Lumbar decompression whereby a piece of bone(lamina) and supporting ligaments is removed to open the narrowed spinal canal (5). The major drawback of lumbar decompression surgery is that it creates instability in the low back as a result of removing important bones and ligaments. This instability oftentimes leads to additional degenerative changes in the spine.
- Lumbar fusion where two or more of the vertebral bodies are bolted together (6). There are significant complications associated with lumbar fusion which include infection, nerve injury, escalation in pain and adjacent segment disease (ASD). The job of the disc is to absorb the forces of daily living. When one of more discs are surgically fused the forces of daily living are then transferred to the lumbar disc and facet above and below the fusion which can result in injury, degeneration and in many cases pain. A recent study found 11.7% in patients who had lumbar fusions developed adjacent segment disease at 28 months. (7).
- Interspinous process spacers are thin implanted spacers designed to create more space more space in the spinal canal without removing the bone. (8)
How Effective is Spinal Stenosis Surgery?
Literature for lumbar stenosis is not very encouraging. One high-level randomized trial followed patients for 8 years. Patients were randomized to surgery or non-operative care. At 8 years surgery was not found to be superior to non-operative care. (9) Another study followed 169 patients from 2000-2007 who were randomly assigned PT or surgery (10). Surgical decompression had a similar effect as physical therapy (9). A different study critically reviewed 26 studies and 5 randomized control studies and was unable to demonstrate surgery to be the superior treatment to non-surgical for lumbar stenosis (11). What was interesting was the number of side effects in the surgical cases ranged from 10-24 % vs zero in the non-surgical group. Complications included stroke, respiratory distress, heart attack, and death due to a blood clot.
Are There Alternatives to Back Surgery for Spinal Stenosis?
Yes!
The Regenexx DDD procedure uses precise injections of platelets into the lumbar spine. The Centeno-Schultz Clinic pioneered the procedure and has successfully treated many patients. Specifically, the platelets are injected:
- Into facet joints to reduce swelling and overgrowth. Overgrowth as illustrated above can cause stenosis.
- Around spinal nerves to reduce swelling and increase blood flow. This allows for a better electrical signal to the muscles.
- Into spinal muscles to improve stability. Stability is critical in the lumbar spine and provided by ligaments and muscles.
- Into the ligamentum flavum to improve the stability and reduce thickening. Ligamentum flavum thickening as illustrated above can cause stenosis.
To better understand Regenexx DDD click on video below.
Spinal stenosis is the narrowing of the central spinal canal and is a cause of significant pain and disability. Common causes of spinal stenosis include disc protrusion, facet overgrowth and ligamentum flavum thickening. Surgery is often chosen when conservative therapies fail despite the lack of convincing evidence that it is a superior treatment option. Are there alternatives to back surgery for spinal stenosis? Yes. Regenexx DDD utilizes precise platelet injections into the facets, muscles, and ligaments to treat the lumbar stenosis, treating all of the components of the issue, which is crucial.
Treatment Options
ACDF Surgery
ACDF stands for “anterior cervical discectomy and fusion.” It is a surgical procedure performed on the neck to relieve pressure on the spinal cord or nerve roots caused by a damaged or degenerated disc. During the procedure, the surgeon removes the damaged disc and replaces it with a bone graft or synthetic implant. Metal plates and screws may be used to hold the vertebrae together during the fusion process. ACDF surgery can help relieve symptoms such as neck pain, numbness, tingling, and weakness in the arms or hands caused by nerve compression in the neck. It is a commonly performed procedure…
Read More About ACDF SurgeryArtificial Cervical Disc Replacement Surgery
Also known as cervical disc replacement is a surgical procedure designed to alleviate neck pain and other symptoms caused by a herniated disc, annular tears, and degenerative discs that fail conservative treatments. While this technology is still new, the promise from surgeons and the companies that are producing the device touted it as a solution to the ASD – adjacent segment disease that comes with fusion of the cervical spine. In reality, that didn’t happen, but it has reduced ASD. Research has shown that ACDF (anterior cervical discectomy with fusion) can result in ASD 7-8 out of 10 times.
Read More About Artificial Cervical Disc Replacement SurgeryCervical Disc Replacement
Cervical disc arthroplasty (CDA), also known as cervical disc replacement, is a surgical procedure used to treat cervical disc disease. The procedure involves removing the damaged or degenerated intervertebral disc in the cervical spine and replacing it with an artificial disc device. CDA is typically performed for patients with symptomatic cervical disc disease, such as disc herniation, degenerative disc disease, or spinal stenosis. The procedure is intended to relieve symptoms such as neck pain, arm pain, and numbness or tingling in the arms or hands. CDA is considered a less invasive and more motion-preserving alternative to traditional cervical spinal fusion surgery…
Read More About Cervical Disc ReplacementDisc Replacement Surgery
The surgeon first accesses the spinal column (for example, in the cervical spine, the surgeon would access the spine through an incision in the front of the neck). From here the surgery is quite aggressive as the disc is scraped and chiseled out of the disc space. Pins are screwed into the vertebrae above and below the disc space that will anchor the space in place as the surgeon works. A tool is inserted into the disc space and used to further separate the upper and lower vertebrae, enlarging the space. The vertebrae surfaces within the disc space are prepared…
Read More About Disc Replacement SurgeryL 4/5 Fusion Surgery
Spinal fusion is a major surgery where one or more spinal bones (vertebrae) are fused together using screws, bolts, and or plates. The hardware may be placed in the front (anterior) or the back (posterior) of the spine. The disc between the spinal bones is often times removed and replaced with bone or a spacer. L 4/5 refers to the level of the surgery. There are 5 spinal bones in the low back which are numbered from top to bottom L1, L2, L3, L4, and L5. Sandwiched between each of the spinal bones is a disc. The disc is named for the two spinal bones it is sandwiched between.
Read More About L 4/5 Fusion SurgeryL5 S1 Fusion Surgery
Spinal fusion is a major surgery where one or more spinal bones (vertebrae) are fused together using screws, bolts, and or plates. The hardware may be placed in the front (anterior) or the back (posterior) of the spine. The disc between the spinal bones is often times removed and replaced with bone or a spacer. L5 S1 Fusion refers to the level of the surgery. There are 5 spinal bones in the low back which are numbered from top to bottom L1, L2, L3, L4, and L5. Sandwiched between each of the spinal bones is a disc. The disc is named for the two spinal bones it is sandwiched between.
Read More About L5 S1 Fusion SurgeryLaminectomy
A laminectomy is a surgical procedure designed to relieve pressure on the spinal cord or nerves by removing a portion of the vertebral bone called the lamina. This procedure is typically performed to alleviate symptoms caused by spinal stenosis, herniated discs, or other conditions that result in spinal nerve compression. By removing the lamina, the spinal canal is widened, reducing pressure and providing relief from pain, numbness, and weakness. This surgery is often recommended when conservative treatments, such as physical therapy and medication, have not provided sufficient relief.
Read More About LaminectomyNSAIDs
The other day I was evaluating a patient and reviewing the treatment options for their spine condition. After discussing prior treatments, we got to the topic of medications taken for pain relief. She explained that she mainly utilized anti-inflammatory (NSAID) medications and then she told me to hold much she takes and has been for many years…..she takes close to 2 grams (2000 milligrams) on a daily basis which equated to about 9-10 capsules of medication per day. I was shocked, considering she was pre-diabetic and with high blood pressure plus the kicker of it is that her PCP (primary care physician) is ok with this…
Read More About NSAIDsPerc-FSU – Trusted Alternative to Spinal Fusion
The Perc-FSU Procedure is an injection-based treatment that utilizes the patients’ own blood platelets to bring stability to the spine without the need for the rods, nuts, bolts, and hardware of fusion surgery. “Perc” stands for percutaneous, and “FSU” stands for “Functional Spinal Unit,” which means that the spine is treated as one functioning unit. Up and down the spine, the discs, facet joints, ligaments, and muscles that assist in stabilizing the spine are treated with image-guided injections of PRP and Platelet Lysate to help bring stability to the spine as a whole. It is the trusted alternative to spinal fusion.
Read More About Perc-FSU – Trusted Alternative to Spinal FusionPLIF Surgery
PLIF is a specific type of lumbar fusion surgery. It is an acronym that stands for the Posterior Lumbar Interbody Fusion (1). Posterior refers to the approach used by the surgeon. Posterior refers to the backside of the body vs anterior which refers to the front. Lumbar is the section of the spine involved. The spine is divided into cervical, thoracic, and lumbar. Lumbar is your low back. Interbody fusion refers to a specific type of fusion. For example, in interbody fusion, the disc is surgically removed and a bone graft and spacer is inserted between the spinal bones (vertebral bodies). The inserted bone graft is expected…
Read More About PLIF SurgeryThoracic Spine Surgery
Thoracic spine surgery is a major surgery aimed at treating injuries in the thoracic spine. Because of the complex anatomy and close proximity to the heart and lungs, there are significant surgical risks and complications. Surgery on the thoracic spine can take hours and may require deflating the lung in order to gain access to the thoracic injury. Recovery can be lengthy depending upon the specific thoracic spine surgery performed. There are several different types of thoracic spine surgery. The specific thoracic spine performed depends upon the underlying thoracic injury and a symptoms of the patient. For example, a thoracic disc herniation…
Read More About Thoracic Spine SurgeryTransforaminal Lumbar Interbody Fusion (TLIF)
Transforaminal Lumbar Interbody Fusion is a variant of the Posterior Lumbar Interbody Fusion (PLIF) technique described by Cloward in the 1950s. PLIF has been associated with the high incidences of neurological complications, up to 13.6% of permanent neurologic lesions in Barnes’ et al. study, in particular of the traversing nerve root (2,3) This is due to the fact that a great amount of traction on the dural sac is required to implant the interbody fusion devices. Surgeons have transitioned to TLIF in efforts to reduce complication rates. Success rates vary depending on what literature you read and recently all orthopedic surgery literature has come under fire…
Read More About Transforaminal Lumbar Interbody Fusion (TLIF)Common Symptoms of Spinal Stenosis
Big Toe Numbness
Believe it or not, one of those significant issues that can present as numbness stems from the low back. In the lumbar spine, the nerve that exits the spine at the L5 level branches down through the hip, thigh, knee, lower leg, and, yes, all the way into the foot and toes. So a pinched or irritated nerve at that L5 level in the back can create problems, such as pain, numbness, tingling, and so on, anywhere along the nerve branch. So what can irritate the L5 spinal nerve? The list is long, but it includes disc issues, such as herniated…
Read More About Big Toe NumbnessCervicalgia / Neck Pain
Cervicalgia is also known as neck pain, which is an all-too-common, unpleasant pain. Read here to learn the symptoms, diagnosis, and treatment options. We will discuss other causes for cervicalgia. What symptoms are associated with cervicalgia? How is cervicalgia diagnosed? What are the treatment options for cervicalgia? Cervicalgia is a medical term used to describe neck pain. It is very common and affects approximately 2/3 of the population at some point in their life. Cervicalgia is the 4th major cause of disability. Risk factors include injury, prior history of neck and musculoskeletal pain, jobs that require a lot of desk work, low social support, job insecurity, physical weakness, and poor computer station setup.
Read More About Cervicalgia / Neck PainKnee Twitching & Spasms
Knee twitching and or spasms are common occurrences that can be caused by a variety of factors. In most cases, it is not a cause for concern and does not require treatment. However, in some instances, knee twitching may be a sign of a more serious condition. Knee twitching is often accompanied by a feeling of pins and needles or tingling in the knee. It may also be accompanied by a burning sensation. The twitching usually occurs intermittently and lasts for a few seconds. There are a number of things that can cause knee twitching. Some of the most common…
Read More About Knee Twitching & SpasmsLeft Arm Numbness
Treatment depends upon the underlying cause of the arm numbness. Left-arm numbness is a warning sign that requires attention. As noted above unexplained numbness requires immediate attention. At the Centeno-Schultz Clinic, we are experts in the treatment of left-arm numbness due to cervical nerve irritation, cervical stenosis, thoracic outlet syndrome, and peripheral nerve injuries. When appropriate first-line treatment should involve conservative care including physical therapy and stretching. Steroid injections should be avoided as they are toxic to orthopedic tissue and can accelerate damage. Surgery for Cervical Stenosis and Thoracic…
Read More About Left Arm NumbnessLeg Gives Out
Have you ever been walking and your leg gives out? It can be both surprising and alarming What would cause your leg to give out? Can sciatica cause your leg to give out? How do you treat weak legs? Let’s dig in.Weakness in the leg can arise from three principal sources: nerve problems, muscle weakness, and SI joint dysfunction. Weakness in the legs may indicate a significant nerve problem. In many cases, it may be the first indication of a nerve problem. There are three common causes of nerve injury: low back disorders, nerve compression as it descends down into the hip, thigh, and shin and medical conditions such as diabetes…
Read More About Leg Gives OutLower Back Pain When Sitting
After a long day on your feet sitting down is supposed to be way to relaxing. Unfortunately for some sitting for any length of time can be painful. Most people experience low back pain at some point in their life. The lifetime prevalence of low back pain is 85% (1). Let’s take a deeper look at the different types of pain and causes of low back pain when sitting. Pain can present in many different ways. It can be intermitent or constant. The quality of the low back pain can also vary depending upon the actual source of injury. Common examples include: Sharp and Stabbing, Dull and Aching, Throbbing/ Pulsating, Pins and Needles, Burning, Electrical
Read More About Lower Back Pain When SittingNerve Pain in Knee
Nerve pain in the knee can be very irritating and life-altering during normal activities as well as leisurely pursuits. Nerve pain in the knee can radiate from the lumbar spine, the pelvis, or the small nerves in the knee. It also can begin after surgery from surgical nerve irritation from the incision or can be the type of pain related to knee arthritis. At the Centeno-Schultz Clinic, we are experts in spine, pain management, and non-surgical orthopedics. We perform a thorough physical examination and musculoskeletal ultrasound of your knee to identify the root cause of your pain and how to treat it appropriately….
Read More About Nerve Pain in KneePain In Left Side Of Neck
Almost everyone has experienced a sore or stiff Neck at some point. The overall prevalence of Neck pain ranges from 04. to 86.8% of the general population (1). Read more to learn the signs, symptoms, causes of treatment options for pain in the left side of Neck. Neck pain can arise from a number of different conditions. Common causes of minor, intermittent Neck pain include fatigue, improper sleeping position, stress and overactivity. If neck pain persists it is a warning sign that you may have a problem that warrants investigation. Think of it as the red engine light on your car. It is warning that if left unchecked can progress to serious and expensive consequences.
Read More About Pain In Left Side Of NeckPain In The Back Of The Heel
Heel pain can be intense and, despite rest and trying a variety of other conservative measures, it can often also be persistent. Every year, there are over a million visits to primary physicians for plantar heel pain. Plantar heel pain affects both men and women equally, and there are many causes of plantar heel pain. Therefore, it is important to diagnose the cause of the heel pain so that it can be treated appropriately. We will review the causes, complications, and treatment options for plantar heel pain.
Read More About Pain In The Back Of The HeelWeak in Knees
Weakness in the knee can be a symptom of many different knee conditions. Some of the most common causes of weakness in the knee include ligament tears, meniscus tears, and arthritis. Another important but often overlooked cause of knee weakness is irritation or injury of the nerves in the low back. If you are experiencing any type of weakness in your knee for long durations of time (3 weeks), it is important to see a doctor to determine the cause. Some of the most common symptoms of knee weakness include difficulty standing up from a seated position, difficulty walking, climbing or descending stairs…
Read More About Weak in Knees3 Questions to Ask Before You Get Spinal Stenosis Surgery
Spinal stenosis is often an age-related condition attributed to compounding osteoarthritis, where the cushion positioned between vertebral discs starts to break down over time, causing a narrowing of the spinal canal and pinched nerves throughout the back and legs.
Often, physicians recommend surgery to those suffering from spinal stenosis…but is surgery the only option? And is it the best option?
Before you agree to undergo invasive surgery for your spinal stenosis, there are a few questions you should consider:
#1: How effective is spinal stenosis surgery, anyway?
While surgery is a common enough recommendation for spinal stenosis treatment, the biggest question that should be on a patient’s mind is, Will this actually work?
What the Research Says…
One research study around spinal stenosis treatment examined patients who had surgery for their spinal stenosis versus those who did not have surgery; unfortunately, the trial found that, once patients got to four years after surgery (or more), there was no difference between those who had undergone surgery and those who had not (11). Another high-level study randomized patients, looking for differences between those who had gone through with spinal stenosis surgery versus patients who had simply adhered to a regular physical therapy regimen. Results concluded that surgery patients did no better than physical therapy patients when it came to long-term effectiveness against spinal stenosis (12).
This research seems to show that spinal stenosis surgery is no silver bullet for alleviating the symptoms that come with the condition. In fact, in the long-term, there is no evidence that an invasive procedure such as this one provides any better, more lasting relief than other spinal stenosis treatment options.
#2: What are the risks associated with spinal stenosis surgery? Is it dangerous?
It’s important to remember that spinal stenosis surgery is considered major surgery. As such, there are most definitely complications that can arise from this procedure, as with any major surgery. However, because this particular procedure is operating on areas around a patient’s spine, it’s important to weigh the severity of potential complications as well.
It is important to understand, as well, that when it comes to spinal surgeries, the definition of a “complication” may differ between the actual surgeons and the patients themselves, meaning that patients can often feel complications after the fact, as opposed to during the procedure itself (13). In one analysis that reviewed five different large studies, the complication rate of surgery as reported by surgeons who conducted the spinal stenosis procedure was a wide range: between 10 and 24%. That can be anywhere from 1 in 10 patients, to 1 in 4 patients. Reported complications include infection, nerve damage, the need for follow-up surgery, and even increased pain, among other issues, all from a procedure that is supposed to alleviate those very concerns.
#3: Can I avoid spinal stenosis surgery altogether? Are there alternatives for spinal stenosis treatment?
There are a handful of different spinal stenosis treatment options that do not involve major surgery, though some are more invasive than others.
One option is a Coflex device, which is a metal spacer that is implanted in between the spinous processes, often after surgical decompression (18). The thought process behind implanting this device is that it will preserve some motion. However, complications can arise through implantation, which may include destruction of the normal fascia, muscles, and ligaments in the area.
Another spinal stenosis treatment option is something called the MILD procedure. This is a type of spinal stenosis treatment that cuts the ligamentum flavum, or the swollen ligament that often places pressure on the spinal cord or nerves. The idea is that this ligament will retract back like a rubber band (19). While this does, in fact, open up the area, it also reduces spinal stability, since this ligament, uncut, helps to keep things stable.
There are also spinal stenosis treatment options that can be performed or implanted using just x-ray guidance, with no surgical procedure at all. For instance, a newer implant-based solution such as interspinous spacers, like the Superion device, that can be inserted during fluoroscopy (20). However, though the device is placed without surgery, the implant still can destroy the original ligament architecture, putting more pressure on the discs.
There is, however, another way. The process we have patients undergo at Centeno-Schultz is one that both avoids surgery and avoids hurting or altering a patient’s original ligament structure. Our procedure is called the Perc-Flavoplasty, and is the only spinal stenosis treatment procedure of its kind, designed to maintain a patient’s normal anatomy with no metal implantations. Our patients not only appreciate the less invasive procedure, they report afterward that they feel much better.
We use precise, image-guided injections in the Perc-Flavoplasty, ensuring that we find the exact area causing a patient pain, ensuring the best possible results. All of our physicians are musculoskeletal specialists with advanced training, and our procedures are backed by extensive research and published patient outcome data. One recent patient, a 66-year-old female working in healthcare, came to use with severe central canal stenosis in her low back; she was able to only stand for 15 minutes at a time before seeing us. After three injection-based treatments using both fluoroscopy and ultrasound guidance, all in our Perc-Flavoplasty method, the patient is now able to stand for more than an hour at a time and is even planning an upcoming vacation where she will be walking for miles at a time.
Our Doctors Who Can Assist with Spinal Stenosis

Christopher J. Centeno, MD
Christopher J. Centeno, M.D. is an international expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate in orthopedics.
Dr. Centeno is one of the few physicians in the world with extensive experience in the culture expansion of and clinical use of adult bone marrow concentrate to treat orthopedic injuries. His clinic incorporates a variety of revolutionary pain management techniques to bring its broad patient base relief and results. Dr. Centeno treats patients from all over the US who travel to Colorado to undergo innovative, non-surgical treatments. Dr. Centeno has chaired multiple international research-based conferences. He also maintains an active research-based practice, with multiple publications listed in the US National Library of Medicine. Dr. Centeno has also served as editor-in-chief of a medical research journal dedicated to traumatic injury.
Dr. Centeno trained at the Baylor College of Medicine, Texas Medical Center, and the Institute for Rehabilitation Research. He hails from both Florida and New York and currently resides in Boulder, Colorado with his wife and three children.

John Schultz, MD
John R. Schultz M.D. is a national expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate for orthopedic injuries. He is board certified in Anesthesiology and Pain Medicine and underwent fellowship training in both. Dr. Schultz has extensive experience with same day as well as culture expanded bone marrow concentrate and sees patients at the CSC Broomfield, Colorado Clinic, as well the Regenexx Clinic in Grand Cayman. Dr. Schultz emphasis is on the evaluation and treatment of thoracic and cervical disc, facet, nerve, and ligament injuries including the non-surgical treatment of Craniocervical instability (CCI). Dr. Schultz trained at George Washington School of…
Read more
John Pitts, M.D.
Dr. Pitts is originally from Chicago, IL but is a medical graduate of Vanderbilt School of Medicine in Nashville, TN. After Vanderbilt, he completed a residency in Physical Medicine and Rehabilitation (PM&R) at Emory University in Atlanta, GA. The focus of PM&R is the restoration of function and quality of life. In residency, he gained much experience in musculoskeletal medicine, rehabilitation, spine, and sports medicine along with some regenerative medicine. He also gained significant experience in fluoroscopically guided spinal procedures and peripheral injections. However, Dr. Pitts wanted to broaden his skills and treatment options beyond the current typical standards of care.
Read more
Jason Markle, D.O.
Post-residency, Dr. Markle was selected to the Interventional Orthopedic Fellowship program at the Centeno-Schultz Clinic. During his fellowship, he gained significant experience in the new field of Interventional Orthopedics and regenerative medicine, honing his skills in advanced injection techniques into the spine and joints treating patients with autologous, bone marrow concentrate and platelet solutions. Dr. Markle then accepted a full-time attending physician position at the Centeno-Schultz Clinic, where he both treats patients and trains Interventional Orthopedics fellows. Dr. Markle is an active member of the Interventional Orthopedic Foundation and serves as a course instructor, where he trains physicians from around the world.
Read more
Brandon T. Money, D.O., M.S.
Dr. Money is an Indiana native who now proudly calls Colorado home. He attended medical school at Kansas City University and then returned to Indiana to complete a Physical Medicine and Rehabilitation residency program at Indiana University, where he was trained on non-surgical methods to improve health and function as well as rehabilitative care following trauma, stroke, spinal cord injury, brain injury, etc. Dr. Money has been following the ideology behind Centeno-Schultz Clinic and Regenexx since he was in medical school, as he believed there had to be a better way to care for patients than the status quo. The human body has incredible healing capabilities…
Read moreOur Other Resources Relating to Spinal Stenosis
The Spine Owner’s Manual: How to Avoid Back Pain & Life-Altering Surgery
This e-book from Dr. Chris Centeno focuses on the spine and how it functions within the human musculoskeletal system and the body as a whole. Everything in our bodies works together like a well-tuned symphony to support our well-being, and a strong spine (including all of its component parts, such as spinal nerves, ligaments, muscles, etc.) is critical to complete health.
Using the Regenexx SANS approach, The Spine Owner’s Manual provides a series of tests and clearly defined exercises that you can do on your own to measure and monitor your own spinal health. These musculoskeletal tests will allow you to monitor where your own body might be struggling to maintain proper stability, articulation, symmetry, and neuromuscular function.
References
- Lurie JD, Tosteson TD, Tosteson A, et al. Long-term outcomes of lumbar spinal stenosis: eight-year results of the Spine Patient Outcomes Research Trial (SPORT). Spine (Phila Pa 1976). 2015;40(2):63–76. doi: 10.1097/BRS.0000000000000731
- Delitto A, Piva SR, Moore CG, Fritz JM, Wisniewski SR, Josbeno DA, et al. Surgery Versus Nonsurgical Treatment of Lumbar Spinal Stenosis: A Randomized Trial. Ann Intern Med. 2015;162:465–473. doi: 10.7326/M14-1420
- Ratliff JK, Lebude B, Albert T, Anene-Maidoh T, Anderson G, Dagostino P, Maltenfort M, Hilibrand A, Sharan A, Vaccaro AR. Complications in spinal surgery: comparative survey of spine surgeons and patients who underwent spinal surgery. J Neurosurg Spine. 2009 Jun;10(6):578-84. doi: 10.3171/2009.2.SPINE0935.
- Zaina F, Tomkins-Lane C, Carragee E, Negrini S. Surgical versus non-surgical treatment for lumbar spinal stenosis. Cochrane Database Syst Rev. 2016;2016(1):CD010264. Published 2016 Jan 29.doi: 10.1002/14651858.CD010264.pub2
- Epstein NE, Hollingsworth RD. Nursing Review Section of Surgical Neurology International Part 2: Lumbar Spinal Stenosis. Surg Neurol Int. 2017;8:139. Published 2017 Jul 7.doi: 10.4103/sni.sni_150_17
- Lurie J, Tomkins-Lane C. Management of lumbar spinal stenosis. BMJ. 2016 Jan 4;352:h6234. doi: 10.1136/bmj.h6234.
- Vail D, Azad TD, O’Connell C, Han SS, Veeravagu A, Ratliff JK. Postoperative Opioid Use, Complications, and Costs in Surgical ManagementofLumbarSpondylolisthesis.Spine(PhilaPa1976).2018;43(15):1080–1088.doi: 10.1097/BRS.0000000000002509
- Li D, Hai Y, Meng X, Yang J, Yin P. Topping-off surgery vs posterior lumbar interbody fusion for degenerative lumbar disease: a comparativestudyofclinicalefficacyandadjacentsegmentdegeneration.JOrthopSurgRes.2019;14(1):197.Published2019Jun28. doi: 10.1186/s13018-019-1245-3
- Chen H, Kelling J. Mild procedure for lumbar decompression: a review. Pain Pract. 2013 Feb;13(2):146-53. doi: 10.1111/j.1533-2500.2012.00574.x.
- Nunley PD, Deer TR, Benyamin RM, Staats PS, Block JE. Interspinous process decompression is associated with a reduction in opioid analgesia in patients with lumbar spinal stenosis. J Pain Res. 2018;11:2943–2948. Published 2018 Nov 20. doi: 10.2147/JPR.S182322
- Lee GY, Guen YL, Lee JW, et al. A new grading system of lumbar central canal stenosis on MRI: an easy and reliable method. Skeletal Radiol. 2011;40(8):1033-9.DOI: 10.1007/s00256-011-1102-x
- Arabmotlagh M, Sellei RM, Vinas-Rios JM, Rauschmann M. [Classification and diagnosis of lumbar spinal stenosis]. Orthopade. 10.1007/s00132-019-03746-1.DOI: 10.1007/s00132-019-03746-1
- Zaina F, Tomkins-Lane C, Carragee E, Negrini S. Surgical Versus Nonsurgical Treatment for Lumbar Spinal Stenosis.Spine. 2016;41(14):E857-68. https://www.ncbi.nlm.nih.gov/pubmed/27128388
- Lurie J, Tomkins-Lane C. Management of lumbar spinal stenosis.BMJ. 2016;352:h6234. DOI:10.1136/bmj.h6234. https://www.ncbi.nlm.nih.gov/pubmed/26727925
- Overdevest GM, Jacobs W, Vleggeert-Lankamp C, Thomé C, Gunzburg R, Peul W. Effectiveness of posterior decompression techniques compared with conventional laminectomy for lumbar stenosis.Cochrane Database Syst Rev. 2015;(3):CD010036. https://www.ncbi.nlm.nih.gov/pubmed/25760812
- Försth P, Ólafsson G, Carlsson T, et al. A Randomized, Controlled Trial of Fusion Surgery for Lumbar Spinal Stenosis.N Engl J Med. 2016;374(15):1413-23. https://www.ncbi.nlm.nih.gov/pubmed/27074066
- Zhong ZM, Deviren V, Tay B, Burch S, Berven SH. Adjacent segment disease after instrumented fusion for adult lumbar spondylolisthesis: Incidence and risk factors. Clin Neurol Neurosurg. 2017;156:29-34.DOI: 10.1016/j.clineuro.2017.02.020
- Nunley PD, Shamie AN, Blumenthal SL, Orndorff D, Block JE, Geisler FH. Interspinous Process Decompression: Expanding Treatment Options for Lumbar Spinal Stenosis.Biomed Res Int. 2016;2016:3267307. https://www.ncbi.nlm.nih.gov/pubmed/27819001.
- Lurie JD, Tosteson TD, Tosteson A, et al. Long-term outcomes of lumbar spinal stenosis: eight-year results of the Spine Patient Outcomes Research Trial (SPORT).Spine. 2015;40(2):63-76. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4288009/
- Delitto A, Piva SR, Moore CG, Fritz JM, Wisniewski SR, Josbeno DA, et al. Surgery Versus Nonsurgical Treatment of Lumbar Spinal Stenosis: A Randomized Trial. Ann Intern Med. 2015;162:465–473. doi: 10.7326/M14-1420.
- Zaina F, Tomkins-Lane C, Carragee E, Negrini S. Surgical versus non-surgical treatment for lumbar spinal stenosis.Cochrane Database Syst Rev. 2016;(1):CD010264. doi: 10.1002/14651858.CD010264.pub2