Prolotherapy: Cervical Spine
Am I a Candidate?At the Centeno-Schultz Clinic, we are musculoskeletal specialists who are highly trained to evaluate and treat simple and complex orthopedic conditions. Many of the tools we use to treat these conditions are known as orthobiologics, which are basically things that come from your own body that assist in your healing mechanisms.
But not everyone needs a PRP or cellular therapy! In some cases, we utilize a much more simple injectate called “prolotherapy.” This too, can aid in your body’s repair…so today let’s dive into all things prolotherapy for neck (cervical) conditions to learn more. This is just another tool in our tool belt to help get our patients better without surgery.
What Is Prolotherapy for the Cervical Spine?
Prolotherapy, short for “proliferative therapy,” is a non-surgical treatment method designed to promote the healing of injured tendons, ligaments, and joints by inducing a controlled inflammatory response.
The procedure involves injecting a solution, typically consisting of a concentration of dextrose (sugar water), into the injured or weakened areas to stimulate the body’s natural healing processes. Here’s a brief discussion of how prolotherapy can be applied to treat conditions of the cervical spine:
Mechanism of action:
- Stimulating healing: The injected solution induces localized inflammation. This inflammation attracts growth factors and stimulates the body to repair damaged tissues.
- Strengthening ligaments and tendons: By promoting the formation of new collagen tissue, prolotherapy can help strengthen weakened ligaments and tendons in the cervical spine.
- Stabilizing the cervical spine: Strengthened ligaments can help stabilize the cervical spine, reducing excessive movement and associated pain.
To review cervical spine anatomy, please see this article on cervical spine anatomy.
Conditions Treated by Prolotherapy
Applications for the cervical spine:
Chronic Neck Pain
Prolotherapy can address chronic neck pain arising from ligament laxity or minor cervical spine instability.
Whiplash/Ligament Injuries
After vehicular accidents or other trauma, patients may experience neck pain due to stretched or torn ligaments. Prolotherapy can help in the healing and tightening of these ligaments.
Cervicogenic Headaches
These are headaches that originate from problems in the cervical spine, often due to weakened or injured ligaments and joints. Prolotherapy can potentially address the cervical issues leading to these headaches.
Arthritis-Related Pain
While prolotherapy won’t reverse arthritis, it can help alleviate pain by stabilizing the surrounding ligamentous structures, thus reducing joint irritation.
Stiff Neck
Cervical Disc Problems
Benefits of Prolotherapy for the Cervical Spine
Prolotherapy for the cervical spine has gained attention as a potential non-surgical intervention for various neck-related conditions. It targets weakened or damaged ligaments, tendons, and joints, aiming to stimulate the body’s natural healing processes. Here are some of the reported benefits of prolotherapy for the cervical spine:
- Pain reduction: One of the primary benefits reported by patients undergoing prolotherapy is a significant reduction in pain. By promoting the healing of weakened or injured ligaments and tendons, prolotherapy can help decrease inflammation and alleviate chronic pain.
- Improved stability: The cervical spine is stabilized by a complex network of ligaments and tendons. Prolotherapy can help strengthen these structures, resulting in enhanced stability of the neck. This can be particularly beneficial for those with minor cervical spine instabilities.
- Reduced headaches: Cervicogenic headaches, which originate from issues in the cervical spine, can be alleviated through prolotherapy. By addressing the root causes in the cervical region, many patients report fewer and less severe headaches.
- Enhanced mobility: With reduced pain and increased stability, many patients experience improved range of motion and flexibility in their necks.
- Alternative to surgery: For some patients, prolotherapy offers a non-surgical alternative to address cervical spine issues. This means fewer risks associated with surgeries, such as infections or complications and no prolonged recovery periods.
- Increased collagen production: Prolotherapy stimulates the production of collagen, a key component of ligaments and tendons. This results in thicker and stronger tissues, further aiding in the stability of the cervical spine.
- Long-term relief: While it might require multiple sessions, many patients report long-term pain relief after completing their prolotherapy treatment regimen. This is because the therapy aims to address the root causes of the pain rather than just masking the symptoms.
- Safety and tolerance: When administered by trained professionals, prolotherapy has a good safety profile with minimal side effects. Most adverse reactions are mild and temporary, such as pain or swelling at the injection site.
- Complement to other therapies: Prolotherapy can be effectively combined with other treatments, such as physical therapy, to maximize therapeutic benefits. This holistic approach can lead to better outcomes in cervical spine rehabilitation. In many instances, we utilize a combination of prolotherapy and PRP in spinal cases to maximize patients’ outcomes.
The Background of Prolotherapy
Prolotherapy has its roots in the early 20th century. The earliest documented use of an injection therapy resembling prolotherapy can be traced back to the 1930s.
Dr. Earl Gedney, an osteopathic physician, is often credited with the initial development of the technique. He stumbled upon the idea after he himself sustained a thumb injury and noticed improvement after an accidental injection that caused inflammation.
Recognizing the potential therapeutic benefits of such injections, Dr. Gedney began refining the technique and presented his findings to the osteopathic community in the mid-1930s.
In the subsequent decades, particularly in the 1950s and 1960s, the technique was further developed and popularized by physicians like Dr. George Hackett. Dr. Hackett conducted extensive research on prolotherapy, which he termed “proliferative therapy” because of its ability to proliferate, or stimulate the growth of, new tissue. He published a foundational textbook on the subject, “Ligament and Tendon Relaxation Treated by Prolotherapy,” which has been instrumental in establishing prolotherapy’s place in medicine.
Since those early days, the techniques, solutions used, and applications of prolotherapy have evolved, but the core principle—inducing a controlled inflammatory response to promote healing—has remained consistent.
The Prolotherapy Process
While those early days helped establish prolotherapy as an effective treatment option for many orthopedic conditions, how it was done in the old days is far from how much more advanced we have become in current-day practice.
It is important when getting prolotherapy or any type of orthobiologic that guidance and precision are paramount for the physician giving the treatment. This means that gone are the old days when a physician would ask, “Where does it hurt” and then start feeling and poking the areas several times. These blind injections, while effective, are not the most efficient way to achieve the fastest success.
The best and current day standard of care is with needle guidance and planned structure injections. More precision-guided injections are the key to short-term and long-term success.
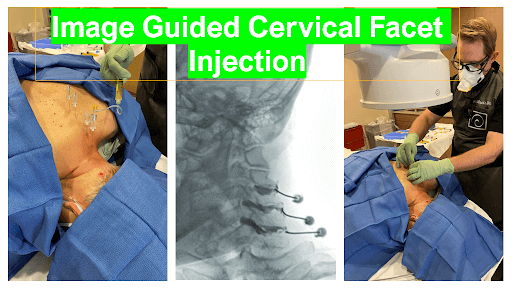
Also for safety, physicians should always understand where their needle is. Poorly placed needles can result in catastrophic injuries, especially in the cervical spine. The cervical spine houses your spinal cord, brainstem, and multiple structures vital to your central nervous system. Poorly placed injections can result in terrible complications such as strokes, spinal cord injuries, and paralysis, to name a few.
Best Candidates for Cervical Spine Prolotherapy
Prolotherapy is a regenerative injection therapy that stimulates the body’s natural healing processes to strengthen and repair injured and painful joints and connective tissue. It involves injecting a substance, commonly a solution of dextrose, saline, and local anesthetic, into the affected area to stimulate healing.
When it comes to the cervical spine, prolotherapy can be an option for individuals with various conditions, although it’s essential to consult with a qualified physician to determine your suitability. Here are some of the best candidates for cervical spine prolotherapy:
- Chronic neck pain: Patients who have tried conventional treatments (like physiotherapy, medications, etc.) without relief might consider prolotherapy as an option.
- Whiplash injuries: Prolotherapy can be effective for patients who have lingering pain after a whiplash injury.
- Ligament or tendon strain: In cases where the ligaments or tendons supporting the neck are weakened or overstretched, prolotherapy can be considered.
- Osteoarthritis: Patients with cervical osteoarthritis, which results in the degeneration of the joints in the neck, might benefit from prolotherapy.
- Cervical instability: For those who have excessive movement between cervical vertebrae due to weakened ligaments, prolotherapy can help strengthen and stabilize the area.
- Disc issues: Although more research is needed, some individuals with degenerative disc disease or other disc-related problems in the neck have reported relief after undergoing prolotherapy.
- Headaches and migraines: Some types of headaches or migraines that are believed to originate from neck issues might respond well to prolotherapy.
- Sports injuries: Athletes with neck injuries that haven’t healed properly might be suitable candidates.
- Post-surgery pain: In some cases, if pain persists after a neck surgery, prolotherapy might be considered as a treatment option.
- Individuals looking for alternative treatments: For those who wish to avoid surgery or prolonged use of medications, prolotherapy might be an attractive option.
However, not everyone is a suitable candidate for prolotherapy. It might not be recommended for:
- Individuals with certain medical conditions such as active cancers, infections, bleeding disorders, or certain types of rheumatological conditions
- Pregnant women
- People who are on certain medications like anticoagulants
It’s crucial for patients to have a thorough evaluation and discuss potential risks and benefits with a knowledgeable physician, ideally one who specializes in regenerative medicine or physical medicine and rehabilitation.
Find Out if Prolotherapy Is Right for You
While prolotherapy can be an effective treatment for many cervical conditions, finding the right physician who can properly evaluate your condition and, more importantly, deliver an accurate/guided injection to obtain the maximal benefit is key.
At the Centeno-Schultz Clinic, our physicians are among the top leading interventionists in the world. If you are considering an alternative to surgery and traditional medicine, contact us today so we can set you up for an evaluation to see what treatment option is right for you!

Christopher J. Centeno, MD
Christopher J. Centeno, M.D. is an international expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate in orthopedics.
Dr. Centeno is one of the few physicians in the world with extensive experience in the culture expansion of and clinical use of adult bone marrow concentrate to treat orthopedic injuries. His clinic incorporates a variety of revolutionary pain management techniques to bring its broad patient base relief and results. Dr. Centeno treats patients from all over the US who travel to Colorado to undergo innovative, non-surgical treatments. Dr. Centeno has chaired multiple international research-based conferences. He also maintains an active research-based practice, with multiple publications listed in the US National Library of Medicine. Dr. Centeno has also served as editor-in-chief of a medical research journal dedicated to traumatic injury.
Dr. Centeno trained at the Baylor College of Medicine, Texas Medical Center, and the Institute for Rehabilitation Research. He hails from both Florida and New York and currently resides in Boulder, Colorado with his wife and three children.

John Schultz, MD
John R. Schultz M.D. is a national expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate for orthopedic injuries. He is board certified in Anesthesiology and Pain Medicine and underwent fellowship training in both. Dr. Schultz has extensive experience with same day as well as culture expanded bone marrow concentrate and sees patients at the CSC Broomfield, Colorado Clinic, as well the Regenexx Clinic in Grand Cayman. Dr. Schultz emphasis is on the evaluation and treatment of thoracic and cervical disc, facet, nerve, and ligament injuries including the non-surgical treatment of Craniocervical instability (CCI). Dr. Schultz trained at George Washington School of…
Read more
John Pitts, M.D.
Dr. Pitts is originally from Chicago, IL but is a medical graduate of Vanderbilt School of Medicine in Nashville, TN. After Vanderbilt, he completed a residency in Physical Medicine and Rehabilitation (PM&R) at Emory University in Atlanta, GA. The focus of PM&R is the restoration of function and quality of life. In residency, he gained much experience in musculoskeletal medicine, rehabilitation, spine, and sports medicine along with some regenerative medicine. He also gained significant experience in fluoroscopically guided spinal procedures and peripheral injections. However, Dr. Pitts wanted to broaden his skills and treatment options beyond the current typical standards of care.
Read more
Jason Markle, D.O.
Post-residency, Dr. Markle was selected to the Interventional Orthopedic Fellowship program at the Centeno-Schultz Clinic. During his fellowship, he gained significant experience in the new field of Interventional Orthopedics and regenerative medicine, honing his skills in advanced injection techniques into the spine and joints treating patients with autologous, bone marrow concentrate and platelet solutions. Dr. Markle then accepted a full-time attending physician position at the Centeno-Schultz Clinic, where he both treats patients and trains Interventional Orthopedics fellows. Dr. Markle is an active member of the Interventional Orthopedic Foundation and serves as a course instructor, where he trains physicians from around the world.
Read more
Brandon T. Money, D.O., M.S.
Dr. Money is an Indiana native who now proudly calls Colorado home. He attended medical school at Kansas City University and then returned to Indiana to complete a Physical Medicine and Rehabilitation residency program at Indiana University, where he was trained on non-surgical methods to improve health and function as well as rehabilitative care following trauma, stroke, spinal cord injury, brain injury, etc. Dr. Money has been following the ideology behind Centeno-Schultz Clinic and Regenexx since he was in medical school, as he believed there had to be a better way to care for patients than the status quo. The human body has incredible healing capabilities…
Read moreYou can find non-surgical solutions for chronic neck pain. Learn more about how we approach prolotherapy at the Centeno-Schultz Clinic.
Am I a Candidate?
To answer this question, fill out the candidate form below to request a new patient evaluation, and a patient advocate will reach out to you to determine your next steps. Your one-hour, in-office or telemedicine evaluation will be with one of the world’s experts in the field of Interventional Orthopedics.