Understanding Cervical Radiofrequency Ablation
Am I a Candidate?Chronic neck pain can be a persistent challenge, impacting daily activities and diminishing the quality of life for many individuals. Among the innovative interventions aiming to alleviate this discomfort, cervical radiofrequency ablation stands out as a promising and minimally invasive procedure.
In this introduction, we delve into the intricacies of cervical radiofrequency ablation, shedding light on how this technique offers relief to those grappling with cervical facet joint-related pain.
Cervical Facets
Neck pain can arise from different structures in the spine, including the muscles, tendons, ligaments, discs, and facet joints.
Facet joints also referred to as zygapophysial joints or Z joints, are located in the back portion of the spine. Each of us has two facet joints per cervical level, one on the right and one on the left. They provide support and stability and facilitate motion in the neck.
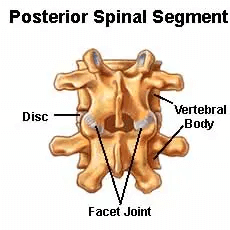
Like other joints in the body such as the knee or ankle joint, the cervical facets are lined with cartilage.(1) Cervical is the medical term for the neck. The cervical facets are susceptible to injury due to trauma such as rear-end motor vehicle accidents and martial arts, which can cause significant pain and restriction in neck movement.(2)
Pain from the injured cervical facet can be localized at the level of the injury or can be referred to the shoulders or scapula(3) as illustrated to the right.
How Radiofrequency Ablation Works
Radiofrequency ablation (RFA) or radiofrequency neurotomy (RFN), is a medical procedure utilized to treat facet-related pain.(4) Ablation means to remove or to destroy. Radiofrequency ablation uses heat energy to destroy the nerve or nerves that transmit the pain signals.
The procedure involves placing needles near the nerve that is transmitting the pain signals from the damaged cervical facet joint. This needle is then heated, thereby “barbecuing” the nerve and adjacent tissue, which kills the nerve and stops the transmission of pain.
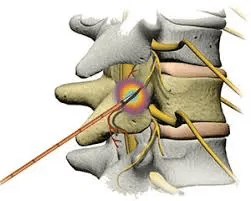
Radiofrequency ablation for neck pain does not treat the underlying issue, as the cervical facet remains injured. It simply turns off the pain signal by burning the nerve. Pain relief is temporary, as the nerve grows back. Pain relief lasts about 6-12 months, on average.
Variations of Cervical Radiofrequency Ablation (RFA)
Cervical radiofrequency ablation encompasses various techniques, each designed to address chronic neck pain with precision. These variations offer distinct approaches to disrupting pain signals from the cervical facet joints. Two notable variations are radiofrequency thermo-coagulation and pulsed RFA.
- Radiofrequency thermo-coagulation: Radiofrequency thermo-coagulation (RFT), often referred to as continuous radiofrequency ablation, involves the application of continuous and controlled heat to the targeted nerves.
The radiofrequency energy heats the nerves to temperatures ranging from 50 to 90oC. A specialized needle is precisely guided to the identified nerves responsible for transmitting pain signals. Once the needle is correctly positioned, radiofrequency energy is continuously applied, creating a thermal lesion on the nerves.
The controlled heat disrupts the nerves’ ability to transmit pain signals, providing relief to the patient. RFT offers a consistent and continuous application of heat. The procedure is effective in providing relief from chronic neck pain associated with facet joint issues.
- Pulsed RFA: Pulsed RFA, in contrast, involves the application of radiofrequency energy in pulses, creating a cyclical pattern of heating and cooling. The heat applied is typically at a lower level compared to continuous radiofrequency ablation.
Similar to continuous RFA, a specialized needle is guided to the targeted nerves responsible for transmitting pain signals. The intermittent heating disrupts pain signals while minimizing the risk of tissue damage. The cyclical nature of pulsed heating may reduce the risk of complications associated with prolonged exposure to high temperatures.
What Happens During the Procedure
Cervical radiofrequency ablation is a carefully orchestrated medical procedure aimed at providing relief from chronic neck pain associated with facet joint issues. This minimally invasive intervention involves several key stages, from preparatory measures to the actual procedure and subsequent post-treatment care.
Preparation involved:
- Setting up an IV line: Before the procedure begins, a healthcare professional may set up an intravenous (IV) line to ensure access to medications or fluids if needed during the process.
- Connecting to monitoring equipment: Monitoring equipment, such as electrocardiogram (ECG) and blood pressure monitors, will be employed to continuously assess vital signs throughout the procedure.
- Proper positioning: Ensuring the patient is in the correct position is crucial for the success of the procedure. This often involves lying on the stomach or back, depending on the specific technique used.
- Cleansing the injection site: The targeted area for needle insertion is thoroughly cleansed to minimize the risk of infection.
- Confirming precise needle injection: Using imaging guidance, such as fluoroscopy, the healthcare provider precisely positions the needle at the nerves responsible for transmitting pain signals. This step ensures accurate and effective treatment.
During the procedure
Radiofrequency current application: Once the needle is correctly positioned, a radiofrequency current is passed through the hollow needle. This current generates heat, creating a thermal lesion on the nerves responsible for transmitting pain signals from the cervical facet joints.
Post-treatment care
Waiting for further instructions: After the completion of the cervical radiofrequency ablation procedure, patients are typically observed for a short period. It is essential to follow the specific instructions provided by the healthcare provider regarding post-treatment care.
Is Radiofrequency Ablation Painful?
Radiofrequency ablation for neck pain can hurt. A needle is placed in your neck and then heated up to 194oF(5) to destroy the nerve and adjacent tissue.
When It Becomes the Ideal Treatment Option
Cervical radiofrequency ablation emerges as an ideal treatment option when individuals experience chronic pain associated with specific conditions affecting the cervical facet joints. Healthcare providers may recommend RFA for a range of conditions, each characterized by persistent discomfort that may not respond adequately to conservative treatments.
Here are some scenarios where cervical RFA becomes a viable and effective treatment option:
- Spinal arthritis: Osteoarthritis or degenerative arthritis can affect the cervical facet joints. Cervical RFA can provide relief from the pain and inflammation associated with spinal arthritis by disrupting the pain signals transmitted by the affected nerves.
- Sacroiliitis: Sacroiliitis is inflammation of the sacroiliac joints, which can cause pain radiating to the neck. When sacroiliitis contributes to neck pain, cervical RFA may be recommended to target and alleviate the discomfort originating from the cervical facet joints.
- Neck pain: Chronic neck pain can benefit from RFA, particularly when it is attributed to facet joint issues. Cervical RFA is a targeted approach to address chronic neck pain by interrupting the pain signals from the affected nerves, offering relief to individuals who may not respond adequately to other treatments.
- Shoulder pain: When shoulder pain is associated with facet joint issues in the cervical spine, RFA can be considered to alleviate the discomfort and improve overall shoulder function.
- Chronic upper back pain: Cervical RFA becomes an ideal treatment option for individuals experiencing chronic upper back pain originating from the cervical facet joints. It offers a focused and minimally invasive approach to managing their symptoms.
What Are the Side Effects of Radiofrequency Ablation?
Radiofrequency ablation for neck pain is associated with several side effects, which include:
Infection
Infection may involve the skin or deeper structures such as muscle and bone. Antibiotics are often required.
Nerve Damage
Radiofrequency ablation targets the nerves that transmit the pain signal from the cervical facet to the brain. Unfortunately, the nerves that control strength and feeling in the arm and hand are nearby and can be temporarily or permanently damaged.
Heavy or Weak Head
Radiofrequency ablation for neck pain can also result in neck muscle weakness. Some of our patients have described their heads as feeling like a bowling ball on a golf tee after the procedure due to muscle weakness.(6)
Skin Numbness
After radiofrequency ablation for neck pain, most patients will complain about severe skin pain like sunburn for 10-14, days followed by months of skin numbness in the neck. This is the result of the nerve being burned.
Dizziness
The muscles in the upper cervical spine are critical to our sense of position and balance. Radiofrequency ablation for neck pain destroys important nerves, which can compromise muscle function and balance.(7)
Phrenic Nerve Injury
The phrenic nerve is important as it controls your ability to breathe. Radiofrequency ablation for neck pain has been reported to injure the phrenic nerve.(7) Feeling short of breath with ongoing neck pain is a difficult combination.
Atrophy of Supporting Muscles
Atrophy refers to a decrease in size or wasting away of a specific tissue. Muscle atrophy means a decrease in the size of muscles.
A case in point is Christopher Reeve, who traumatically sustained a spinal cord injury. Before the injury, he had powerful, well-defined muscles. After the injury, his muscles atrophied and became small. Radiofrequency ablation has been associated with atrophy of the key supporting muscles in the spine.(8)
Hyperesthesia
Hyperesthesia refers to an increased sensitivity to stimuli, where individuals may perceive ordinary sensations as more intense or painful than usual. Following cervical radiofrequency ablation, hyperesthesia may occur as a side effect due to nerve irritation or altered sensory processing.
Patients may experience heightened sensitivity in the areas surrounding the treated nerves. Common sensations include increased sensitivity to touch or changes in temperature.
The duration and severity of hyperesthesia can vary among individuals. Patients are advised to promptly report any unusual or uncomfortable sensations to their healthcare provider.
Allergic Reaction
An allergic reaction occurs when the body’s immune system responds adversely to a substance, resulting in a range of symptoms. Allergic reactions during or after cervical radiofrequency ablation may be associated with components of the injected solutions, such as local anesthetics or contrast agents used during the procedure.
Symptoms can range from mild skin irritation to more severe reactions, including rash, itching, swelling, or difficulty breathing.
In rare cases, individuals may experience anaphylaxis, a severe and potentially life-threatening allergic reaction. Immediate medical attention is necessary if an allergic reaction is suspected.
Regenerative Medicine Options
At the Centeno-Schultz Clinic, we focus on regenerative medicine. We seek to support nerve health using the body’s healing agents, not destroying them.
An injured facet joint that is causing neck pain, muscle spasms, and restriction in range of motion is best treated by addressing the underlying joint instead of disrupting the pain signal to the brain through the burning of a nerve.
At the Centeno-Schultz Clinic, we have extensive experience in the treatment of neck pain. Treatment options include PRP and bone marrow concentrate. Both are precisely injected via ultrasound or X-ray guidance by a board-certified, fellowship-trained physician.
PRP is rich in growth factors that can increase the blood flow to a given area as well as reduce inflammation and has been effective in the treatment of facet injuries.(10)
Bone marrow concentrate contains many different types of cells, including repair cells that can accelerate your body’s natural healing process of tendon, ligament, and facet injuries.
Make Your Treatment Less Painful but More Effective
Facet joints are important structures located in the back portion of the spine. They provide stability, support, and motion and are susceptible to injury, with resultant pain and restriction in range of motion.
RFA for neck pain involves the destruction of the pain-transmitting nerves, thereby limiting the pain signal to the brain. The underlying joint remains injured and susceptible to additional injury.
At the Centeno-Schultz Clinic, we are experts in regenerative medicine. Treatment of the underlying facet injury is best for optimal long-term success as opposed to the burning of nerves with its significant side effects and its need to be repeated almost annually.
PRP and bone marrow concentrate are effective, natural options for radiofrequency ablation and the management of cervical facet pain.
Ready to take your life back from CCI, without surgery and medication? See if you are a candidate for the PICL Procedure.

Christopher J. Centeno, MD
Christopher J. Centeno, M.D. is an international expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate in orthopedics. He is board-certified in physical medicine and rehabilitation with a subspecialty of pain medicine through The American Board of Physical Medicine and Rehabilitation. Dr. Centeno is one of the few physicians in the world with extensive experience in the culture expansion of and clinical use of adult bone marrow concentrate to treat orthopedic injuries. His clinic incorporates a variety of revolutionary pain management techniques to bring its broad patient base relief and results. Dr. Centeno treats patients from all over the US who…
Read more
John Schultz, MD
John R. Schultz M.D. is a national expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate for orthopedic injuries. He is board certified in Anesthesiology and Pain Medicine and underwent fellowship training in both. Dr. Schultz has extensive experience with same day as well as culture expanded bone marrow concentrate and sees patients at the CSC Broomfield, Colorado Clinic, as well the Regenexx Clinic in Grand Cayman. Dr. Schultz emphasis is on the evaluation and treatment of thoracic and cervical disc, facet, nerve, and ligament injuries including the non-surgical treatment of Craniocervical instability (CCI). Dr. Schultz trained at George Washington School of…
Read more
John Pitts, M.D.
Dr. Pitts is originally from Chicago, IL but is a medical graduate of Vanderbilt School of Medicine in Nashville, TN. After Vanderbilt, he completed a residency in Physical Medicine and Rehabilitation (PM&R) at Emory University in Atlanta, GA. The focus of PM&R is the restoration of function and quality of life. In residency, he gained much experience in musculoskeletal medicine, rehabilitation, spine, and sports medicine along with some regenerative medicine. He also gained significant experience in fluoroscopically guided spinal procedures and peripheral injections. However, Dr. Pitts wanted to broaden his skills and treatment options beyond the current typical standards of care.
Read more
Jason Markle, D.O.
Post-residency, Dr. Markle was selected to the Interventional Orthopedic Fellowship program at the Centeno-Schultz Clinic. During his fellowship, he gained significant experience in the new field of Interventional Orthopedics and regenerative medicine, honing his skills in advanced injection techniques into the spine and joints treating patients with autologous, bone marrow concentrate and platelet solutions. Dr. Markle then accepted a full-time attending physician position at the Centeno-Schultz Clinic, where he both treats patients and trains Interventional Orthopedics fellows. Dr. Markle is an active member of the Interventional Orthopedic Foundation and serves as a course instructor, where he trains physicians from around the world.
Read more
Brandon T. Money, D.O., M.S.
Dr. Money is an Indiana native who now proudly calls Colorado home. He attended medical school at Kansas City University and then returned to Indiana to complete a Physical Medicine and Rehabilitation residency program at Indiana University, where he was trained on non-surgical methods to improve health and function as well as rehabilitative care following trauma, stroke, spinal cord injury, brain injury, etc. Dr. Money has been following the ideology behind Centeno-Schultz Clinic and Regenexx since he was in medical school, as he believed there had to be a better way to care for patients than the status quo. The human body has incredible healing capabilities…
Read moreAm I a Candidate?
To answer this question, fill out the candidate form below to request a new patient evaluation, and a patient advocate will reach out to you to determine your next steps. Your one-hour, in-office or telemedicine evaluation will be with one of the world’s experts in the field of Interventional Orthopedics.