Laminectomy
Am I a Candidate?If you have had an MRI of your spine, you are probably like most patients. You read the MRI report and then google every term on your MRI report from the Radiologist trying to figure out what it all means! Alternatives to Laminectomy should be an important part of that search.
Today you’re in luck, we are going to take a deep dive into the term “Spinal Stenosis”, so you’ll have a better understanding of what it means anatomically, clinically, and how to avoid spinal surgery because of it. Lets dig in!
Lumbar Spinal Stenosis (LSS) is one of the most diagnosed spinal disorders of patients over 45 years old. At least 200,000 adults in the United States have LSS symptoms that require treatment. The Framingham Study reported a prevalence of absolute Lumbar Stenosis of 47.2% for patients aged 60–69 years, with this number increasing with age.
What Does “Lumbar Stenosis” Mean?
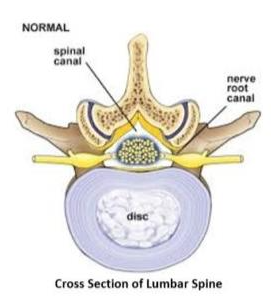
Lumbar Stenosis = narrowing or crowding of the spinal nerves as the travel down the spinal canal or as they exit the spinal canal via foramen.
Narrowing or crowding of the nerves can be caused by multiple things in the spinal canal:
1. Disc bulge / herniation push backwards into the nerves
2. Thickened ligamentum flavum, a ligament that can become thickened pushing forward into the canal
3. Arthritic facet joints can become hypertrophied (enlarged with bone spurs), pushing forward into the canal
With the disc pushing backwards and the facets / ligaments pushing forwards, the descending spinal nerves get caught in the middle creating stenosis symptoms!
What Are the Symptoms of Lumbar Stenosis?
Patients with Lumbar Stenosis symptoms classically complain of “ Neurogenic Claudication”, which is a doctor term for pain or discomfort that radiates to the hip, lower leg, thigh, and/or buttocks while walking.
– Patients typically report relieving symptoms of neurogenic claudication with sitting down or leaning forward, referred to as the “shopping cart sign.”
– We document patient’s “walking tolerance” in minutes and blocks with many patients limited to walking few minutes or a single block before symptoms start arising!

What is Treated with a Laminectomy?
Degenerative Scoliosis
Degenerative Scoliosis, also known as Adult-onset Scoliosis, is a medical condition that involves a side bending in the spine. The bending can be mild, moderate, or severe with side-bending to either the right or the left. The term degenerative means generalized wear and tear and is common as we get older. Degenerative scoliosis is the curvature of the spine that occurs as a result of degeneration of the discs, small joints, and building blocks. The Degenerative Scoliosis curve is often located in the low back and forms a ‘C” shape. There is a convex and a concave side. The convex side is the open side where it curves outward.
Read More About Degenerative ScoliosisPinched Nerves in the Back
We talk a lot about leg pain stemming from a pinched or irritated nerve in the lower back. And, indeed, that’s what our physicians are traditionally taught in medical school—a pinched nerve in the lumbar spine typically presents as a symptom in the leg. However, what if you have some butt pain but no pain or other symptoms in the leg? Does this mean it couldn’t be a pinched nerve? Not so fast. Turns out a pinched low back nerve doesn’t always have to be accompanied by leg symptoms. Let’s start by taking a look at how the back is structured.
Read More About Pinched Nerves in the BackSpinal Instability
Spinal instability is a condition that occurs when the spinal column is not able to maintain its normal alignment and function under normal loads. It can be caused by various factors such as trauma, degenerative changes, infections, tumors, or congenital abnormalities. In a stable spine, the bones, discs, ligaments, and muscles work together to support and protect the spinal cord and nerve roots. However, in an unstable spine, the structures that support the spine may be damaged or weakened. This can lead to abnormal movement and excessive stress on the spinal cord and nerves. In most cases, bone and joint problems…
Read More About Spinal InstabilitySpinal Stenosis
Spinal stenosis is the narrowing of the central spinal canal and is a cause of significant pain and disability. Common causes of spinal stenosis include disc protrusion, facet overgrowth and ligamentum flavum thickening. Surgery is often chosen when conservative therapies fail despite the lack of convincing evidence that it is a superior treatment option. Are there alternatives to back surgery for spinal stenosis? Yes. Regenexx DDD utilizes precise platelet injections into the facets, muscles, and ligaments to treat the lumbar stenosis, treating all of the components of the issue, which is crucial. Spinal stenosis is often an age-related condition attributed…
Read More About Spinal StenosisThoracic Cyst
Cysts are abnormal, closed sacs that contain fluid, gas or semi-fluid material. They can develop in various parts of the body. They can vary in size from very small to large and can be located within organs, tissues or bones. Cysts can be either benign (non-cancerous) or malignant (cancerous). Most cysts are benign. They occur due to a number of different reasons that include obstruction, infection, chronic inflammation, instability or cellular abnormalities. So, thoracic spine cysts are abnormal, closed sacs that occur in the spine below the neck and above the low back.
Read More About Thoracic CystWhat Is a Lumbar Laminectomy?
A Lumbar Laminectomy is a surgical procedure to treat Spinal Stenosis. The Lamina which makes up the roof of the spinal canal is removed to give the nerve additional space.
When Is a Laminectomy Indicated?
Patients with more severe Lumbar Stenosis may also develop lower extremity weakness, muscle cramping, numbness, and imbalance. With the development of muscle weakness and sometimes an emergent situation called “Cauda Equina” where the nerves get pinched so severely that create numbness in the groin and saddle area accompanied with inability to control bowels or bladder (Incontinence). In these situations, emergent laminectomies are sometimes needed!
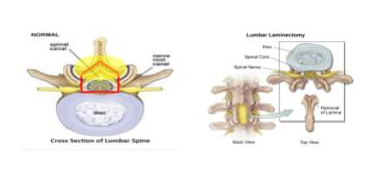
Depending on the root cause of the Spinal Stenosis, Laminectomy may be coupled with additional surgical procedures such as:
– Discectomy: removal of the disc that is bulging, pushing on the nerves.
– Facetectomy: removal of the facet joint that has boney overgrowth, pushing on the nerve.
– Fusion: with removal of the lamina, which provides stability to the spine, the spine becomes unstable requiring fusing the level making it immobile.
Is a Lumbar Laminectomy Successful?
Going under an invasive surgical procedure with significant risks should be a last resort after all less invasive treatment is tried first.
In 2016, a Cochrane Review looked at all the available data complied (12,966 research articles screened!) looking at both surgical and non-surgical treatment outcomes for Lumbar Stenosis. Authors said there is very little confidence to conclude whether surgical treatment or a conservative approach is better for Lumbar Spinal Stenosis! However, it should be noted that the rate of side effects ranged from 10% to 24% in surgical cases, and no side effects were reported for any conservative treatment. Complications sometimes follow surgery, particularly spinal instability resulting in Fusion. In fact, reoperation rates as high as 27% in the first postoperative year have been reported!
– Still, these figures show that at long‐term follow‐up in up to 22% of patients, the results of surgery are unsatisfactory, and patients still have symptoms.
Are there risks of complications with Lumbar Laminectomy, Discectomy and Fusion surgery?
Lumbar Laminectomy with or without Discectomy or Fusion are all invasive surgeries that come with significant risks associated with them! It should be noted that the rate of side effects ranged from 10% to 24% in surgical cases.
- Instability was seen in 5.5% of patients. Instability was seen more frequently in patients with pre-existing Spondylolisthesis (12.6%) and in those treated with open Laminectomy (12%).
- Reoperation for instability was required in 1.8% of all patients, and was higher for patients with preoperative Spondylolisthesis (9.3%) and for those treated with open Laminectomy (4.1%).
- Intraoperative blood transfusion and Dural tear requiring surgical repair, occurred in 2.34% of cases.
- Postoperative delirium 1-3%
- It is estimated that 3% to 12% of patients who have disc surgery will have recurrent symptoms, and most of these patients will have surgery again. Making the case for the need for alternatives to Laminectomy.
Alternatives to Laminectomy
Traditional treatment options before Laminectomy should be considered are medications (NSAIDS, Nerve Medications – Gabapentin), Physical Therapy, Corticosteroid Epidurals should be exhausted before even considering any invasive treatments such as a Laminectomy! But with most of these treatments, they too come at a risk. Check here for issues related to steroids. Therefore, non-surgical alternatives to Laminectomy beyond these treatment options are essential.
Lumbar Stenosis Treatment Without Surgery – Regenexx DDD
As discussed above, Lumbar Spinal Stenosis is developed from 3 main structures being damaged and crowding the spinal nerves. So lets discuss how we have been treating Stenosis non-surgically using advanced procedures using the healing agents from the patient’s own body with the Regenexx DDD procedure!
The spinal level that ends up developing Stenosis first gets sloppy and moves too much, that’s called degenerative instability. That extra motion then causes facet joint arthritis and oftentimes the Ligamentum Flavum will get bigger. This hypertrophy is really the same thing that we see in tendons that get weaker. How does that work?
Let’s focus on why tendons get bigger when they get weak. A normal tendon is small and dense. When a tendon has more wear and tear than it can repair, your body throws more tissue at the problem. However, it’s unable to repair the tendon like the original, so while the per unit area strength of the tendon is less, since the tendon is larger, it can still handle the total loads placed on it. We often fix this using regenerative medicine by injecting substances that will prompt more repair in the tendon than the wear and tear it’s experiencing. This causes the tendon to get smaller and stronger. Now let’s translate these concepts into the Ligamentum Flavum.
If the Ligamentum Flavum also gets more wear and tear than it can repair, it also gets larger or undergoes hypertrophy. Hence, it would make sense that injecting substances that can repair this ligament should make it smaller. A smaller ligament means less pressure on the nerves. However, nobody had ever intentionally injected anything into the Ligamentum Flavum before. Hence, we needed to develop new x-ray guided injection techniques for the DDD procedure.
In our alternatives to Laminectomy, we also focus on treating the whole functional spinal unit in this procedure. Meaning, we also perform precise image-guided injections to strengthen the ligaments and muscles that support this spinal segment, help arthritis in the joint, and reduce the swelling around the irritated spinal nerves. To learn more, see the video below:
Another of the Alternatives to Laminectomy if Regenexx DDD fails
While our goal is to initially avoid any tissue damage and healthy alternatives to Stenosis, a few patients will fail to respond to our Regenexx DDD protocol as discussed above. When this occurs there is a new treatment option that we can combine with the Regenexx DDD protocol called M.I.L.D. procedure (minimally invasive lumbar decompression.
This is an interventional medical device aimed at debulking the Ligamentum Flavum, and there has been excellent short-term follow up research in these patients. But this procedure only addresses the hypertrophied ligament and not the disc injury or the arthritis in the spine which are also a source of pain. So the best of both worlds allow us to utilize the most advanced Interventional Orthopedics with a minimally invasive procedure to maximize our results!
The Upside with Treating Lumbar Spinal Stenosis
We have been using advanced regenerative therapies to treat Lumbar Spinal stenosis for almost 2 decades with great success. We are dedicated to continuing to advance the options patients have that can be safe and effective in treating Lumbar Spinal Stenosis without surgery, allowing patients to continue living their best lives! If you or anyone you know has been living with Spinal Stenosis and contemplating an invasive surgery or looking for alternatives to Laminectomy and traditional treatments like corticosteroid injections, give us a call today and happy to evaluate you and discuss treatment options!
References
Kalichman L, Cole R, Kim DH, Li L, Suri P, Guermazi A, Hunter DJ. Spinal stenosis prevalence and association with symptoms: the Framingham Study. Spine J. 2009 Jul;9(7):545-50. doi: 10.1016/j.spinee.2009.03.005. Epub 2009 Apr 23. PMID: 19398386; PMCID: PMC3775665.
Guha D, Heary RF, Shamji MF. Iatrogenic spondylolisthesis following laminectomy for degenerative lumbar stenosis: systematic review and current concepts. Neurosurg Focus. 2015 Oct;39(4):E9. doi: 10.3171/2015.7.FOCUS15259. PMID: 26424349.
Zaina F, Tomkins-Lane C, Carragee E, Negrini S. Surgical versus non-surgical treatment for lumbar spinal stenosis. Cochrane Database Syst Rev. 2016 Jan 29;2016(1):CD010264. doi: 10.1002/14651858.CD010264.pub2. PMID: 26824399; PMCID: PMC6669253.
Sobottke R, Röllinghoff M, Siewe J, Schlegel U, Yagdiran A, Spangenberg M, Lesch R, Eysel P, Koy T. Clinical outcomes and quality of life 1 year after open microsurgical decompression or implantation of an interspinous stand-alone spacer. Minim Invasive Neurosurg. 2010 Aug;53(4):179-83. doi: 10.1055/s-0030-1263108. Epub 2010 Dec 3. PMID: 21132610.
Oosterhuis T, Costa LO, Maher CG, de Vet HC, van Tulder MW, Ostelo RW. Rehabilitation after lumbar disc surgery. Cochrane Database Syst Rev. 2014 Mar 14;2014(3):CD003007. doi: 10.1002/14651858.CD003007.pub3. PMID: 24627325; PMCID: PMC7138272.
Tohidi M, Lung T, Yen D. Routine perioperative practices and postoperative outcomes for elective lumbar laminectomies. J Spine Surg. 2018 Sep;4(3):588-593. doi: 10.21037/jss.2018.09.01. PMID: 30547123; PMCID: PMC6261752.
Staats PS, Chafin TB, Golovac S, Kim CK, Li S, Richardson WB, Vallejo R, Wahezi SE, Washabaugh EP 3rd, Benyamin RM; MiDAS ENCORE Investigators. Long-Term Safety and Efficacy of Minimally Invasive Lumbar Decompression Procedure for the Treatment of Lumbar Spinal Stenosis With Neurogenic Claudication: 2-Year Results of MiDAS ENCORE. Reg Anesth Pain Med. 2018 Oct;43(7):789-794. doi: 10
Am I a Candidate?
To answer this question, fill out the candidate form below to request a new patient evaluation, and a patient advocate will reach out to you to determine your next steps. Your one-hour, in-office or telemedicine evaluation will be with one of the world’s experts in the field of Interventional Orthopedics.