Patellofemoral Pain Syndrome
Patellofemoral pain syndrome (PFS), also called runner’s knee or retropatellar pain syndrome, is a significant cause of pain in the front of the knee. The pain is usually experienced behind or around the patella (kneecap) when the knee is bent or fully loaded. This post discusses everything you need to know about patellofemoral pain syndrome.
What Is Patellofemoral Syndrome?
Patellofemoral pain syndrome commonly causes pain in the front of the knee (anterior). It is believed to account for about 11-17% of all causes of knee pain (1). The anterior knee pain commonly occurs when the knee is flexed or fully loaded, such as while squatting, running, or cycling.
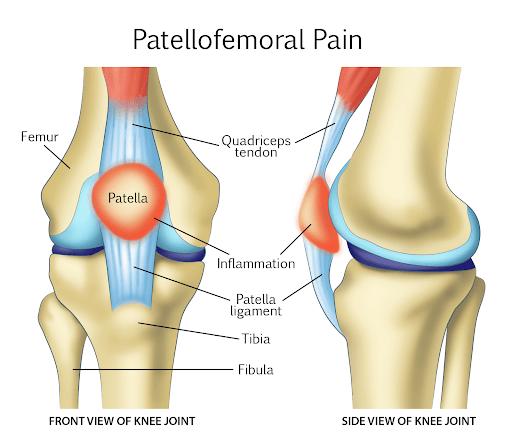
The knee joint is composed of the following structures:
- Bones: thigh bone, shin bone and knee cap
- Synovium of the joint: connective tissue that lines the inside of the joint
- Retinaculum: thick connective tissue on the outside of the knee that supports the kneecap
- Cartilage: strong, flexible connective tissue on the ends of the tibia, femur and underneath the patella that acts a shock absorber and allows the bones to slide smoothly.
- Meniscus: C shaped piece of cartilage that cushions and stabilized the knee joint.
- Muscles: provide stability and movement of the knee. The three major muscles are the quadriceps, hamstring and calf muscle.
The clinical symptoms of patellofemoral pain syndrome are similar to other conditions, such as, patellofemoral osteoarthritis, Osgood-Schlatter disease, plica, prepatellar or Hoffa’s bursitis, saphenous neuritis, quadriceps tendinopathy patellar tendinopathy, chondromalacia patella, and patellar dislocaton.
Anterior knee pain can also arise from irritation of nerves in the low back or hip joint arthritis.
It is important to differentiate patellofemoral pain syndrome from patellofemoral osteoarthritis. Both conditions can cause pain and swelling in the front of the knee. Patellofemoral pain syndrome is a muscoskkeletal disorder that is tyically caused by overuse or poor alignment of the patella.
Patellofemoral arthritis, on the other hand, is a degenerative joint disease characterized by loss of cartilage in the patellofemoral joint (7).
Symptoms Of Patellofemoral Pain Syndrome
Patellofemoral pain syndrome is a common knee condition characterized by pain around the kneecap (patella). Other common symptoms include:
Pain During Muscle Contraction
The quadricep is the large leg anterior muscle that is also known as the thigh. It is an important muscle as it controls kneecap movement during walking, running and jumping. Strong and balanced quadriceps muscles are essential for maintaining proper knee alignment. Individuals with patellofemoral pain syndrome often have pain when the quadriceps contract due to muscular imbalance.
Pain When Squatting
Patients with PFPS often have knee pain that worsens with bending of the knee, climbing stairs, or sitting for prolonged periods with knees bent.
Pain During Palpation of the Kneecap
Individuals with patellofemoral syndrome may have tenderness on palpation of the patella. On palpation, there is localized tenderness of the quadriceps muscles and patellar tendons.
There may also be warmth, swelling, and redness in and around the knee joint.
Restriction in range of Motion
Patients with patellofemoral pain syndrome may experience knee restriction in motion particularly during activities that involve bending and straightening the knee. This limitation in knee range of motion may be due to tightness or weakness in the muscles surrounding the knee joint.
Swelling
Knee swelling is a common symptom of patellofemoral pain syndrome espically after prolonged or high intensity activities. The swelling is typically localized around the kneecap and can be associated with the feeling of stiffness or tightness in the knee joint.
Burning Pain on Outside of Knee When Kneeling
There are many possible causes of burning pain on the outside of the knee while kneeling. One possibility is that you may have patellofemoral syndrome, which is a condition that results in pain around the kneecap. This pain can be aggravated by activities such as kneeling or squatting. Other potential causes of this type of pain include iliotibial band syndrome, runners knee, and meniscal tears. If you are experiencing burning pain on the outside of your knee while kneeling, it is important to see a doctor for evaluation. Some of these conditions can be treated with conservative measures such as rest, ice, and physical therapy…
Read More About Burning Pain on Outside of Knee When KneelingKnee Buckling
Knees can buckle, causing a sensation of one or both knees giving out that affects nearly 17% of adults. The knees are regarded to be one of the most essential (and biggest) joints in the human body because they play significant roles in basic activities such as walking and sitting. When our knees begin to feel unstable, weak, or begin giving out, it is easy to become stressed since we rely so heavily on them for movement. The knee can become stable from numerous types of injuries. The knee is kept stable by the following structures: Tendons attach the leg muscles…
Read More About Knee BucklingKnee Clicking
Clicking in the knee can occur for a number of reasons. The 5 major causes include: ligament injuries, meniscus tears, knee arthritis, patellofemoral syndrome, and soft/scar tissue. Let us start with ligament tears. A ligament is a thick piece of connective tissue that connects one bone to another. The knee has 4 principal ligaments: ACL, PCL, MCL, and LCL. Ligaments provide important stability for the knee (1). If injured or torn, ligaments can create instability. This instability can cause clicking in the knee. As ligaments travel across boney surfaces they can also catch make the knee click. The meniscus is a C-shaped cushion situated between the thigh bone and shin bone.
Read More About Knee ClickingKnee Hurts When I Bend It and Straighten It
Your knees bend countless times throughout the day. Running up the stairs, down the hall after kids, and getting into the car. You straighten the knee as you walk, descend stairs or get into and out of the car. Bending and straightening the knee are necessary for daily activities. Knee pain with bending or straightening may be a mild, transient irritation or may indicate a more significant problem. Learn more below and avoid further injury and dysfunction. Knee pain can vary significantly depending upon many factors including the actual source of the pain, the severity of the injury, general health, and level of activity…
Read More About Knee Hurts When I Bend It and Straighten ItKnee Pain
Knee pain can be caused by many factors. Overuse injuries, direct trauma to the knee and arthritis are the most common causes of knee pain. Damage to the knee structures may cause swelling, scar tissue formation (fibrosis), and loss of function of the joint. Pain is often accompanied by difficulty walking, weakness, and instability. When the knee is overused, the thigh and shin bones (femur and tibia), cartilage, or tendons may experience stress. This leads to pain and discomfort as well as stiffness in the knee. Overuse injuries are common among athletes who participate in sports that involve running, jumping…
Read More About Knee PainKnee Popping
Knee popping can be a sensation that something is moving around in the knee. There may also be an audible sound associated with the popping, which in medical terms is called crepitus. This can also cause what we call mechanical catching or locking, which may make the knee feel like it is stuck in an extended or flexed position, and you have to move it in certain ways to get out of that. This knee popping sensation or sound or could be a very simple issue or it could be a sign that more serious damage is going on in the knee, so determining what is causing it is very important. So, the knees may pop and get in a certain position….
Read More About Knee PoppingKnee Swelling
Swelling of the knee, also known as water on the knee, is a condition in which fluid collects around the knee joint. Swelling can occur for a variety of reasons and affect patients of any age. Some swelling can be treated with over-the-counter medicines, but persistent and continuous swelling might result in tissue damage, bone softening, and cartilage deterioration. Over-the-counter medicines will assist relieve pain for individuals with a history of osteoarthritis and swelling following physical activity, such as exercise or running. During and after activity, the patient may apply compression sleeves to reduce the inflammation. Ice is another method…
Read More About Knee SwellingKnee Twitching & Spasms
Knee twitching and or spasms are common occurrences that can be caused by a variety of factors. In most cases, it is not a cause for concern and does not require treatment. However, in some instances, knee twitching may be a sign of a more serious condition. Knee twitching is often accompanied by a feeling of pins and needles or tingling in the knee. It may also be accompanied by a burning sensation. The twitching usually occurs intermittently and lasts for a few seconds. There are a number of things that can cause knee twitching. Some of the most common…
Read More About Knee Twitching & SpasmsNerve Pain in Knee
Nerve pain in the knee can be very irritating and life-altering during normal activities as well as leisurely pursuits. Nerve pain in the knee can radiate from the lumbar spine, the pelvis, or the small nerves in the knee. It also can begin after surgery from surgical nerve irritation from the incision or can be the type of pain related to knee arthritis. At the Centeno-Schultz Clinic, we are experts in spine, pain management, and non-surgical orthopedics. We perform a thorough physical examination and musculoskeletal ultrasound of your knee to identify the root cause of your pain and how to treat it appropriately….
Read More About Nerve Pain in KneeOutside Knee Pain
What causes outside knee pain? How do you treat it? Let us go over all of this and also review how one patient avoided a huge surgery. What is On the Outside of the Knee? You have a couple of key structures here (1). They include the: Lateral meniscus, Lateral joint compartment, Popliteus tendon, Iliotibial band, Lateral collateral ligament , and anterolateral ligament, and Fibula. The meniscus is a figure-8 shaped fibrous structure (shown here from above) that is a shock absorber for the knee joint. It has an outside part (lateral meniscus) that cushions the joint. The meniscus can become torn or degenerated. If you are young…
Read More About Outside Knee PainCommon Causes Of Patellofemoral Pain Syndrome
The are several different causes of patellofemoral pain syndrome. The most common causes include:
Overuse Or Overload Of The Knee
Overuse or overload of the patellofemoral joint is the most common cause of patellofemoral pain syndrome. These movements can increase the pressure between the patella and femur (thigh bone) increasing the risk for patellofemoral pain syndrome.
Studies have revealed that activities that overload the knee (running, cycling, and work that engages the knee) correlate with an increase in the development of patellofemoral syndrome (2).
Obesity, being overweight, or having a high BMI of over 25, can increase the load on the knee joint, leading to patellofemoral syndrome.
Fall Or Trauma
A fall or direct trauma to the patella can injure the patella and knee joint, leading to inflammation of the patellofemoral joint.
Inflammation of the patella, the muscles, or even the joint’s synovium can cause symptoms of PFS.
Foot Abnormalities
There is a correlation between foot pressure and the knee joint. Dorsiflexion of the ankle refers to the movement where you pull your toes upwards towards your shin.
Studies have found that limited dorsiflexion of the ankle can lead to compensatory movements in the knee during activities like squatting, lunging, or going up stairs. These compensatory movements in turn can increase the pressure between the patella and femur increasing the risk for patellofemoral pain syndrome.
Surgical History
A history of anterior cruciate ligament (ACL) repair surgery can lead to PFS.
Muscle Weakness
Muscle strength is critical for proper patellofemoral joint health and function because the muscles around the knee joint help stabilize and support it. The quadriceps, the large muscle in the front of the thigh helps to control the movement of the kneecap and keep it properly aligned during activities that involve bending and straightening of the knee.
Patellar tracking refers to the patella staying in a boney groove called the trochlear groove. This is located in the femur bone. For optimal knee health and function the patella should track in the trochlear groove as it allows the knee to distribute the weight and pressure of your upper body evently across the joint.
If the patella does not track properly within the trochlear groove it can rub up against the boney sidewall or pop out causing injury to the cartilage.
If the quadriceps are weak or if there is muscular imbalance the patella may not track smoothly within the trochlear groove potentially causing pain, swelling and stiffness in the joint.
Increase BMI
Increased body mass index (BMI) is a risk factor for developing patellofemoral pain syndrome as it puts extra stress on the knee joint during weight bearing activities. In addition increases in body weight can lead to poor alignment of the knee cap increasing the risk of patellofemoral pain syndrome (2A).
Common Treatments For Patellofemoral Syndrome
Treatments for Patellofemoral pain syndrome aim to reduce pain and to correct any misalignment or imbalance issues. The best treatment option will depend upon many factors that include the severity of the misalignment or overuse issues in addition to the overall health of the knee joint. When appropriate conservative care should always been first line treatment. There are conservative and surgical treatment options which are discussed below.
Natural Therapies For Patellofemoral Syndrome
Natural therapies like exercise therapy and physical therapy are the most important treatments for PFS. Other therapies can supplement. However, these are the core of any treatment program for PFS.
- Exercise Therapy: Exercise therapy or exercise physiology is reconditioning the body and relieving symptoms through exercise. A fixed and planned regimen of movements and exercises under a trained health professional can be used to relieve symptoms of PFS.
- Physical Therapy: Physical therapy is designed to restore muscle strength, balance and function. Physical therapists use exercises that aim to increase the joint’s flexibility and the strength of the muscles supporting the joint.
Surgical Approaches For Patellofemoral Syndrome
Surgery is not usually the first option for PFS as the majority of patients do very well with conservative and natural treatments. Surgery is typically only considered when these conservative measures have failed. Some of the surgical options for PFS are listed below:
- Arthroscopy: a surgical procedure in which a small camera is inserted into the knee joint. It allows for visualization of the joint and any areas of injury or degeneration which can then be treated.
- Lateral Release Surgery: also known as lateral retinacular surgery. It involves cutting a band of connective tissue called the lateral retinaculum. The lateral retinaculum holds the kneecap in place. When patellar tracking remains problematic and has not responded to conservative therapy, surgeons often cut the lateral retinaculum to allow the patellar to move more freely and track within th e trochlear groove.
Other designs include the constrained hinged design, non-hinged design, and mobile design. The type of prosthesis used depends on many factors including age, mobility, cause of the PFS, and health of the individual. - Partial Knee Replacement (if one knee compartment is worn out): If just one of the knee compartments is worn out, a partial knee replacement is done. In this procedure, only damaged cartilage and bone are removed in a single compartment of the knee. For patients with severe patellofemoral pain syndrome that has been unresponsive to conservative care and injections, the patella can be removed and replaced with a prosthesis.
- Total Knee Replacement (if two or three knee compartments are worn out): A total knee replacement is where the entire knee joint is replaced if two of the three knee compartments are worn out due to inflammation or overuse.
In this procedure, the bone and cartilage are removed. A femoral metal component, a plastic spacer in between, and a plastic tibia component replace the knee joint.
Non-Surgical Treatments
Several non-surgical therapies can address the symptoms of PFS. Some of them are listed below:
- Ice/NSAIDS/Modalities: Rest and icing the knee are the first steps for pain at the onset of PFS. Analgesics, such as non-steroidal anti-inflammatory drugs (NSAIDs), may also reduce the pain and inflammation around the patella.
Other passive modalities like phonophoresis, iontophoresis, and neuromuscular electrical stimulation may also help; however, there is little clinical data about their efficacy (4). - Ultrasound Therapy: Therapeutic ultrasound can help alleviate the symptoms of PFS. It involves alternating compression and rarefaction of sound waves at a frequency of 0.7 to 3.3 MHz, which help treat PFS. The sound energy produces heat, which relaxes the muscles and reduces inflammation.
- Acupuncture: Acupuncture has been used to treat PFS in conjunction with other therapies. This involves inserting 0.25 mm X 1.5-inch needles at specific points near the patella. It stimulates nerves in the area to release endorphins and alter how the body processes pain.
Additionally, electroacupuncture can be applied for 25-30 minutes. In some cases, infrared radiation is also applied for 3-5 minutes to stimulate certain points around the knee for pain relief. - Orthotics/Bracing/Taping: Orthotics such as foot inserts, insoles, and other foot supports can be used to treat PFS when the foot dynamics are the primary cause of the condition.
For example, flat feet or tightness of the foot muscles are taken care of with orthotics. Additionally, knee braces and straps can also be used to stabilize the patella if there is any patella instability or weakness in the supporting muscles.
Another modality that can reduce pain associated with PFS due to knee instability is Kinesio taping, which can help improve the alignment of the patella. - Steroid Injections: when conservative therapy has failed to provide significant or sustained benefit some patients are referrred for knee steroid injections. Steroids are powerful anti-inflammatory agents that can reduce pain and swelling. Unfortunately they have signficant side effects that include injury to the cartilage and tendons.
- Hyaluronic Acid Injections: Hyaluronic acid is a natural substance found in the body that helps to lubricate and cushion joints. Hyaluronic acid injections are a common treatment option to relieve joint pain and inflammation. The injection helps restore the natural lubrication and cushioning of the joint thereby reducing friction, pressure and pain.
- Regenexx: Regenerative therapies, such as Regenexx, are also a great option for treating PFS. At Centeno Schultz Clinic, our clinicians use platelet-rich plasma (PRP) and stem cells to promote recovery.
Platelet-rich plasma is drawn from the individual and reinjected into the knee joint with additional growth factors that facilitate healing in the inflamed cartilage, patella, and synovium. Stem cells from the bone marrow can also be extracted, processed, and then reinjected into the knee joint to form healthy bone, cartilage, and tissue.
Knee Arthroscopy Surgery
Knee arthroscopy surgery is a very common procedure performed by orthopedic surgeons in an attempt to treat knee pain. Knee arthroscopic surgery is typically performed in an outpatient surgical facility where a small camera is inserted into the knee joint, which allows the surgeon an inside view of one’s knee to operate. It is used both to diagnose and treat a wide variety of knee problems. Utilizing arthroscopic surgery the surgeon can trim any damaged ligaments which are called knee ligament surgery. Alternatively, if ‘damaged’ meniscus is detected, it also is trimmed and or removed, which is called meniscus knee surgery.
Read More About Knee Arthroscopy SurgeryNSAIDs
The other day I was evaluating a patient and reviewing the treatment options for their spine condition. After discussing prior treatments, we got to the topic of medications taken for pain relief. She explained that she mainly utilized anti-inflammatory (NSAID) medications and then she told me to hold much she takes and has been for many years…..she takes close to 2 grams (2000 milligrams) on a daily basis which equated to about 9-10 capsules of medication per day. I was shocked, considering she was pre-diabetic and with high blood pressure plus the kicker of it is that her PCP (primary care physician) is ok with this…
Read More About NSAIDsProlotherapy Injections
It has been successful in the treatment of many disorders including neck, shoulder, knee, and ankle pain. Dr. Centeno recently published an article in The Journal of Prolotherapy in which he discusses the use of x-ray guidance with prolotherapy. This ensures that the injection is in the correct place to maximize clinical results. Dr. Centeno discusses the use of prolotherapy for the treatment of neck, knee, sacroiliac joint, ankle, ischial tuberosity, and shoulder pain. At the Centeno-Schultz Clinic x-ray guided prolotherapy is just one of the therapies utilized in the successful treatment of pain. Regenerative injection therapy (RIT) or prolotherapy…
Read More About Prolotherapy InjectionsPRP Injections
PRP is short for platelet-rich plasma, and it is autologous blood with concentrations of platelets above baseline values. The potential benefit of platelet-rich plasma has received considerable interest due to the appeal of a simple, safe, and minimally invasive method of applying growth factors. PRP treatments are a form of regenerative medicine that utilizes the blood healing factors to help the body repair itself by means of injecting PRP into the damaged tissue. In regenerative orthopedics, it is typically used for the treatment of muscle strains, tears, ligament and tendon tears, minor arthritis, and joint instability. There have been more than 30 randomized controlled trials of PRP…
Read More About PRP InjectionsPRP Knee Injections
PRP stands for Platelet-Rich Plasma. Platelets are blood cells that prevent bleeding. They contain important growth factors that aid in healing. Plasma is the light yellow liquid portion of our blood. So PRP is simply a concentration of a patient’s own platelets that are suspended in plasma and are used to accelerate healing. PRP is NOT stem cell therapy. Regrettably, blood contains few circulating stem cells. Rich sources of stem cells are bone marrow and fat. PRP is rich in growth factors. There are many different types of growth factors with different properties. VEGF is a very important one as it can increase the blood flow to an area.
Read More About PRP Knee InjectionsRisk Factors
Certain risk factors put people at risk of developing patellofemoral syndrome. Some of them are listed below:
High-Impact Activities
Repeated injuries to the knee from high-impact activities, particularly stop/starting movements at high speeds, can damage the patella as it overloads the knee. This includes running, jogging, cycling, stair climbing, and squatting. These high-impact activities can damage and inflame the patella, knee muscles, and tendons.
Engaging in repetitive jogging or cycling, particularly without a training plan or adequate rest in between sessions, it may increase your risk of PFS.
Age
Certain age groups are at a higher risk of developing PFS than others. There is a higher prevalence of PFS in adolescents and young people in their twenties and thirties, although it is unclear why. This could be due to the underdevelopment of the muscles that are attached to the patella (5).
Sex
There is a higher risk of PFS in women. Although the exact reason for this is unclear, it is thought to be associated with weaker quadriceps strength and higher hip adductor muscle angles (5). In women, their wider pelvis increases the angle where the bones in the knee joint meet.
Flat Feet
Flat feet tend to restrict the muscles in the lower extremity and therefore increase the load when the knee is fully flexed. As a result, flat feet can increase the risk of PFS.
Preventing Patellofemoral Syndrome
You can prevent PFS by practicing simple things. They are explained below:
- Always Warm Up Before Exercise: Before beginning any weight-bearing exercises like cycling, running, jogging, or squatting, always remember to warm up first. This will help gradually increase the blood supply to the muscles and the knee joint.
It increases the oxygen supply to the knee, so the chances of injury and fatigue are less. The muscles are also more flexible once they are warmed up. - Lose Extra Weight: Additional weight can increase pressure on the knee. Losing extra weight can help decrease the pressure on the knee joint. Every one pound of weight loss translates to a loss of four pounds of pressure on the knee joint.
- Ensure Patella Alignment: While exercising, keep an eye on the movement of the patella. If there is patellar misalignment, it can give rise to PFS. Sometimes it’s better to work with a trainer who can watch the movement of the knee and correct the exercise form. If there is patellar instability, knee braces and supports are also good options.
- Increase Intensity Slowly: With all exercise and weight-bearing activities, it is important to gradually increase the intensity. This allows the patella and its tendons to get used to the activity.
A sudden increase in the intensity of the activity can lead to patellar misalignment and symptoms of PFS, so it is important to gradually and progressively increase the intensity of the exercise. - Wear The Right Shoes: For those engaged in repetitive activities on hard surfaces, wear shoes that will cushion the impact of the feet against the ground. Additionally, for those who overpronate or have flat feet, it is important to wear orthotics or inserts to correct the deformity and align the foot.
Home Remedies That Can Help With PFS
Some home remedies can help relieve pain and reduce the symptoms of PFS. Some of them include:
- Ice Therapy: Applying ice packs for 10-15 minutes every three hours can ease the pain caused by PFS.
- Turmeric: The active component of turmeric is curcumin which has anti-inflammatory properties. As a result, turmeric can help reduce inflammation around the patella and ease the pain. Turmeric can be added to food or drink, and there are also turmeric capsules available.
- Ginger: Studies have shown that eating raw or heat-treated ginger can reduce muscle pain caused by eccentric exercise of the knee joint (6).
Examination And Diagnosis Of PFS
To diagnose PFS, doctors will do the following:
- History: The doctor will first take an extensive history of the patient and knee symptoms. They will ask about any history of trauma to the knee, knee surgeries, and a history of overall activity. The doctor will also want to know the patient’s occupation, current activity level, and if there have been any recent changes in activity.
- Physical Examination: The doctor will perform a physical examination of the hips, the knees, and the feet. They will palpate the muscles and knee joint to look for tenderness. Muscle strength, particularly in the hip adductors and abductors, will also be tested.
The doctor may ask to inspect the shoes as well to check for excessive wear on either side of the foot. - Special Tests: Certain special tests and maneuvers may be carried out to rule out other conditions.
For example, the Clarke test, the squatting test, the patellar apprehension test, and the patellar tilt test are special tests used to help diagnose various conditions related to the patella. These tests are not very specific. However, if they are positive, it can signify PFS. - Imaging: Imaging is usually only needed to rule out other diagnoses. For example, plain X-rays of the knees can rule out fractures of the patella, osteoarthritis, and osteochondritis of the knee. An MRI, CT, or even a US is not usually necessary but may be ordered if symptoms do not improve with conservative management.
Can Complications Occur If PFS Is Left Untreated?
There are two possible complications of untreated PFS:
- Osteoarthritis: The first complication of untreated PFS is patellofemoral osteoarthritis. This may develop in part due to inadequate patella tracking. Patellofemoral osteoarthritis can, in turn, lead to chronic joint pain.
- Activity Restriction: If PFS is left untreated, many weight-bearing activities can become restricted. This restriction can affect daily activities and lead to stiffness of the joint. It can also lead to weight gain, which can further increase the load on the knee and worsen the symptoms. This vicious cycle continues until the pain becomes chronic.
Early Detection And Treatment Are Key
Patellofemoral pain syndrome must be diagnosed and managed properly. If it is detected and treated early, the prognosis for PFS is generally excellent. In the first two weeks, analgesics, rest, and ice can be started to alleviate any symptoms. At-home exercises and physical therapy sessions to facilitate recovery.
Education is also a key component of treatment, including the importance of rest and the healing timeline. At CSC, our clinicians use regenerative therapies to hasten the recovery from PFS. As the patient’s cells are used, regenerative therapies can help repair and heal the inflamed tissue, so people with PFS have the best possible outcome.
If you have anterior knee pain, then don’t wait. Talk to one of our board-certified doctors today about your options.

Christopher J. Centeno, MD
Christopher J. Centeno, M.D. is an international expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate in orthopedics.
Dr. Centeno is one of the few physicians in the world with extensive experience in the culture expansion of and clinical use of adult bone marrow concentrate to treat orthopedic injuries. His clinic incorporates a variety of revolutionary pain management techniques to bring its broad patient base relief and results. Dr. Centeno treats patients from all over the US who travel to Colorado to undergo innovative, non-surgical treatments. Dr. Centeno has chaired multiple international research-based conferences. He also maintains an active research-based practice, with multiple publications listed in the US National Library of Medicine. Dr. Centeno has also served as editor-in-chief of a medical research journal dedicated to traumatic injury.
Dr. Centeno trained at the Baylor College of Medicine, Texas Medical Center, and the Institute for Rehabilitation Research. He hails from both Florida and New York and currently resides in Boulder, Colorado with his wife and three children.

John Schultz, MD
John R. Schultz M.D. is a national expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate for orthopedic injuries. He is board certified in Anesthesiology and Pain Medicine and underwent fellowship training in both. Dr. Schultz has extensive experience with same day as well as culture expanded bone marrow concentrate and sees patients at the CSC Broomfield, Colorado Clinic, as well the Regenexx Clinic in Grand Cayman. Dr. Schultz emphasis is on the evaluation and treatment of thoracic and cervical disc, facet, nerve, and ligament injuries including the non-surgical treatment of Craniocervical instability (CCI). Dr. Schultz trained at George Washington School of…
Read more
John Pitts, M.D.
Dr. Pitts is originally from Chicago, IL but is a medical graduate of Vanderbilt School of Medicine in Nashville, TN. After Vanderbilt, he completed a residency in Physical Medicine and Rehabilitation (PM&R) at Emory University in Atlanta, GA. The focus of PM&R is the restoration of function and quality of life. In residency, he gained much experience in musculoskeletal medicine, rehabilitation, spine, and sports medicine along with some regenerative medicine. He also gained significant experience in fluoroscopically guided spinal procedures and peripheral injections. However, Dr. Pitts wanted to broaden his skills and treatment options beyond the current typical standards of care.
Read more
Jason Markle, D.O.
Post-residency, Dr. Markle was selected to the Interventional Orthopedic Fellowship program at the Centeno-Schultz Clinic. During his fellowship, he gained significant experience in the new field of Interventional Orthopedics and regenerative medicine, honing his skills in advanced injection techniques into the spine and joints treating patients with autologous, bone marrow concentrate and platelet solutions. Dr. Markle then accepted a full-time attending physician position at the Centeno-Schultz Clinic, where he both treats patients and trains Interventional Orthopedics fellows. Dr. Markle is an active member of the Interventional Orthopedic Foundation and serves as a course instructor, where he trains physicians from around the world.
Read more
Brandon T. Money, D.O., M.S.
Dr. Money is an Indiana native who now proudly calls Colorado home. He attended medical school at Kansas City University and then returned to Indiana to complete a Physical Medicine and Rehabilitation residency program at Indiana University, where he was trained on non-surgical methods to improve health and function as well as rehabilitative care following trauma, stroke, spinal cord injury, brain injury, etc. Dr. Money has been following the ideology behind Centeno-Schultz Clinic and Regenexx since he was in medical school, as he believed there had to be a better way to care for patients than the status quo. The human body has incredible healing capabilities…
Read moreAm I a Candidate?
-
What Is Golfer’s Knee, And What Can I Do About It?
The nature of golf is such that both the backswing and downswing affect the knee. The entire swing takes a little over one second. However, it can exert a force of 4 times the body weight on the front knee and 3 times the weight on the back knee (1). This makes knee injuries just as…
-
Knee Pain Location Chart: What The Pain In Your Knee Means
The knee joint is the largest compound synovial joint of the human body. The joint has bones, cartilage, muscles, and bursae that are held together by ligaments and tendons. Damage to any of these structures can give rise to knee pain. The location of knee pain can be very telling, and can help narrow down…
-
Understanding Knee Pain Symptoms To Get The Best Treatments
Knee pain affects about 25% of the population (1). The knee joint involves three bones, namely the patella, the femur, and the tibia. Knee pain can be a sign of damage to the ligaments, bones, bursae, or muscle tendons because there are so many structures within the knee joint. In this post, we’ll discuss the…
-
KT Tape For Hamstring Tendonitis
Hamstring tendinosis is a condition that causes pain and inflammation in the hamstring tendons. The hamstring tendons are the tough bands of tissue that attach the hamstring muscles to the bones in the back of the thigh. Hamstring tendinosis is a degenerative condition, meaning that it is a condition that causes the tissue to break…
-
6 Meniscus Tear Types And How To Treat Them Properly
Even a small meniscus tear can make walking difficult for you. If you are experiencing any of these symptoms, you may want to seek medical help as soon as possible, depending on the type of tear you have. Needless to say, a lot depends on understanding the meniscus tear types there are and what each…
-
How To Heal A Torn Meniscus Naturally
If you have, or suspect you have a torn meniscus, and you’re wondering how to heal a torn meniscus naturally, you’ve landed on the right post. You may be wondering: Do I need surgery? Can you heal a torn meniscus naturally? The short answer is: It depends. What Is a Meniscus? The meniscus is a…
-
How to Read a Knee MRI for Meniscal Tear
Dr. Chris Centeno discusses how to read a knee MRI for meniscal tears and what you need to know about such tears. Transcript Hi, this is Dr. Centeno. And I’d like to go over today How to Read Your Knee MRI: Focus on the Meniscus. I have a whole series of these and reading a…
-
7 Most Common Symptoms of a Loose Knee Replacement
Walking became impossible. Each step was associated with severe pain. Knee replacement seemed like a good solution. Unfortunately, months after the surgery problems exist. Your doctor thinks you have a loose knee replacement. What is a knee replacement? What causes a knee replacement to become loose? What are the 7 most common symptoms of a…
-
How Likely Is a Second ACL Tear On the Same Knee?
Anterior Cruciate Ligament Injuries and Treatments The ACL (anterior cruciate ligament) is an important knee stabilizing ligament. It prevents the tibia from moving too much frontward (anterior translation) and twisting too much (internal rotation). It is under most stress with landing from a jump, or a planted foot with twisting, and this is how it…
-
How to Read Knee MRI
Transcript for “How to Read Knee MRI” Hi, this is Dr. Centeno and I’d like to go over how to read knee MRI. I got the idea for this when a friend had a knee injury, got an MRI, was sent home with the CD, and just jumped on the internet to try to figure…
References
- Crossley KM, Callaghan MJ, van Linschoten R. Patellofemoral pain. Br J Sports Med. 2016;50(4):247-250. doi:10.1136/bjsports-2015-h3939rep.
- Dye SF. The pathophysiology of patellofemoral pain: a tissue homeostasis perspective. Clin Orthop Relat Res. 2005 Jul;(436):100-10.
2A: Wang, H., Cheng, Y., Shao, D., Chen, J. Y., Wu, H., & Ding, Z. (2018). Association between body mass index and patellofemoral pain in adults: A systematic review. PloS one, 13(4), e0195486. doi: 10.1371/journal.pone.0195486
- Feucht MJ, Cotic M, Beitzel K, et al. A matched-pair comparison of inlay and onlay trochlear designs for patellofemoral arthroplasty: no differences in clinical outcome but less progression of osteoarthritis with inlay designs. Knee Surg Sports Traumatol Arthrosc. 2017;25(9):2784-2791. doi:10.1007/s00167-015-3733-2
- Lake DA, Wofford NH. Effect of therapeutic modalities on patients with patellofemoral pain syndrome: a systematic review. Sports Health. 2011;3(2):182-189. doi:10.1177/1941738111398583
- DeHaven KE, Lintner DM. Athletic injuries: comparison by age, sport, and gender. Am J Sports Med. 1986 May-Jun;14(3):218-24.
- Black CD, Herring MP, Hurley DJ, O’Connor PJ. Ginger (Zingiber officinale) reduces muscle pain caused by eccentric exercise. J Pain. 2010;11(9):894-903. doi:10.1016/j.jpain.2009.12.013
- Witvrouw, E., Callaghan, M. J., Stefanik, J. J., Noehren, B., Bazett-Jones, D. M., Willson, J. D., … & Crossley, K. M. (2014). Patellofemoral pain: consensus statement from the 3rd International Patellofemoral Pain Research Retreat held in Vancouver, September 2013. British journal of sports medicine, 48(4), 411-414.