Dr. Chris Centeno discusses how to read a knee MRI for meniscal tears and what you need to know about such tears.
Transcript
Hi, this is Dr. Centeno. And I’d like to go over today How to Read Your Knee MRI: Focus on the Meniscus. I have a whole series of these and reading a knee MRI requires some knowledge of individual areas. So this one’s going to focus on the Meniscus.
This video isn’t meant as a substitute for a radiology report or your doctor’s opinion. It’s just to educate you about what’s on that image.
Want to Get Back to What You Love, Without Surgery and Medication?
So, what does the Meniscus do?
The Meniscus a shock absorber and a spacer. So basically, it’s the shock absorber and the spacer inside your knee.
But before we start, it’s very important that you understand that there is no evidence that in middle aged to elderly patients a Meniscus tear causes symptoms. Now, you might be very surprised to hear about that, but there’s very good research that shows that Meniscus tears in that age group are just as common as grey hair. So we can’t look at a Meniscus tear on a MRI and say, “Aha, that’s causing your pain in middle-aged or elderly patients,” so be very careful about someone who just looks at your image and says, “That’s what’s causing your pain” because there is no science to support that.
In addition, there’s no evidence that operating on a Meniscus tear with or without arthritis is effective. Again, you might be very surprised to hear that, but multiple high-quality studies have now shown that operating on a Meniscus tear isn’t effective, doesn’t help. So again, just to be absolutely clear on that point, we’re going to talk today about Meniscus tears, but the concept of operating on them has not been supported in the science.
An MRI is a 3D picture that slices through things, and there’s three planes: Sagittal, Coronal, and Axial.
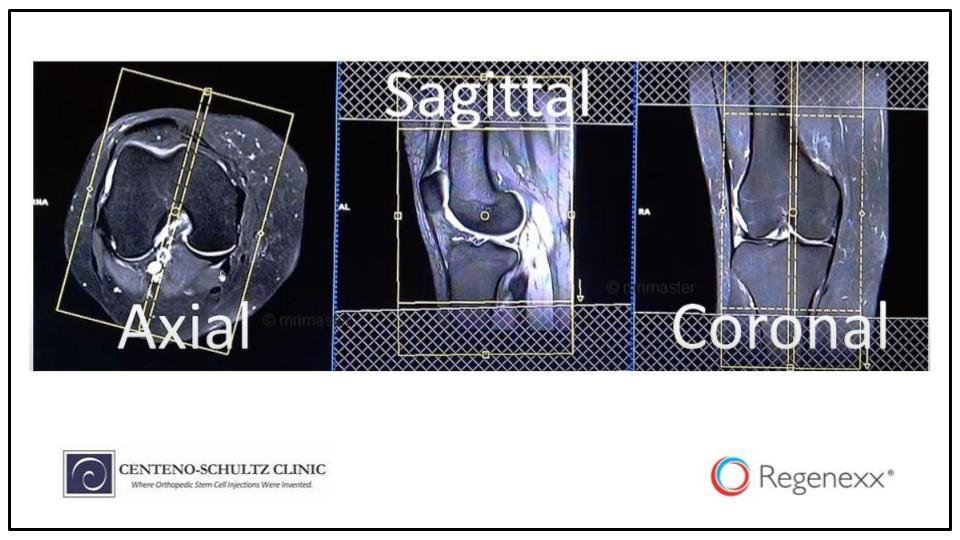
And these are what the three planes look like. The Coronal plane is this front plane. The Sagittal plane is the side plane. And the Axial plane is the sawed in half view or the looking from the top or from the bottom plane.
And on your MRI, this is what they’ll look like. This is what a knee Axial looks like. This is what the Sagittal looks like. And this is what the Coronal looks like. And again, just remember that you’re slicing through a three-dimensional structure.
The easiest way to find the Meniscus is on the Sagittal or Coronal images. This is what the Coronal will look like. This is what the Sagittal will look like.
Look for a dark triangle-shaped structure. You see here, this triangle-shaped structure here, this one here, this one here, and this one here. On the Coronal or Sagittal, the Meniscus will always look like a triangle or at least, the normal Meniscus. And I’m going to highlight those triangles right here.
Now, let’s read an image. I’m going to pop out of this program and go into the image program. This image has been donated by one of our patients who’s allowed her to use her name. And you’ll see here that I’m starting with this one up top which is the coronal image. And it’s where the bone is dark.
And I’m just going to scroll through this image, and I see the Patella there or the kneecap. And then I start to see the main knee bones come in. And I see this Meniscus coming in right here, this triangle. And as I go back further, I’m going to see this other Meniscus coming in and this other triangle, and this is over here, the middle of the Meniscus. And as I go through here, you will see, I can get through the entire Meniscus. As I scroll back to front, this is from the back.
Now I go towards the front. I’m scrolling through the Meniscus, and I see a few things here. I can see that this Meniscus is uniformly dark, and this one’s got a light bit in it, sort of a horizontal white line. And what I’m seeing there is a tear in this Meniscus, and you can always tell the inside from the outside here. The outside is going to have this extra bone on the side or the fibula. This is the outside or lateral. And the other side is the inside or medial. What I’m seeing here is this light bit inside this Meniscus is a tear in the medial Meniscus.
Now I’m going to go to the side view so we can take a quick look at what the side view looks like. And again, I’m starting from the inside here. These always start from the inside. And as I go through, I’m going to start to see the triangles of the Meniscus come in. This white stuff happens to be fluid in this patient. I’m going to see, again, this Meniscus up front looks like a nice uniformly dark triangle, but this Meniscus in the back has got some white stuff in it, and that means that there’s some tearing which we saw before.
Again, this is the medial Meniscus, and now I’m in the back. So I know it’s the posterior or the back medial Meniscus. And then I’m going to go to the middle where I see the PCL and ACL ligaments. That’s the middle. And then as I keep going across, I’m going to now go to the outside, the lateral Meniscus, and I see my little triangles coming in here and triangle and triangle, and those look pretty good. They’re uniformly dark.
So now, let’s switch back to the presentation. And so we can just take a look at what some abnormal Meniscus tissue looks like. So this is an example here of a simple horizontal Meniscus tear. You can see here a horizontal light line in the dark triangle on the Sagittal. And this is on the Sagittal image where the bone is bright. The cartilage is this gray color, and the Meniscus on this image as well is going to be dark.
This is a simple horizontal Meniscus tear on the front or the Coronal view. You can see here, the red arrow points to a white line that goes all the way through this Meniscus. Again, a normal Meniscus is uniformly dark. This white line means a tear.
A bucket handle tear. The best way to understand a bucket handle tear is to look at what it shows up like when you’re looking from the top. This is the normal Meniscus on this side, and you can see its shaped like a C. But on this side, you see a rent or a tear in the Meniscus, and you see that one part of the Meniscus has actually moved inward opening up the tear. When you were looking at this, you’ve got to realize when you’re looking at this on a cross section, you’re slicing across this like so, so you’re going to see one piece of the Meniscus over here and one piece of the Meniscus over there. That’s a bucket handle tear. That means that one piece of the Meniscus has separated from the other one. And if we were to look at it in three dimensions, it would look like this.
A displaced Meniscus with a tear is something else you should be on the lookout for because this is very common when we’re in a situation where the patient has had prior surgery. Basically, the surgeons usually take out this part of the Meniscus inside and that allows the Meniscus to spit outside the joint. So we can see this Meniscus is a nice dark triangle, and it’s contained within the joint, and this Meniscus is now outside the joint. This is where the joint ends. It’s been spit outside the joint, and it’s got this light area in it, so it’s torn and displaced. What does that mean? Well, this Meniscus is acting as a nice shock absorber, and this Meniscus is not.
A displaced Meniscus with bone spurs. You can see here that both of these Meniscuses are kind of pushed out of the joint a little bit, this one more so than this one, but you can see this Meniscus actually is pushed outside the joint, and little spurs have formed here and there. Now, these are what I call functional bone spurs. These bone spurs shouldn’t be taken off because if you take them off surgically, unless they’re causing some other problem, you’re going to end up creating less cushioning for the joint. Right now, this Meniscus has begun to spit outside the joint. The body formed these spurs to take advantage of that new position, and it’s still a valid shock absorber. But if we take those bone spurs off, we’re going to have problems.
A displaced and macerated Meniscus is right here. This is someone who’s got no cartilage on this compartment right here. You can see that this has a normal triangle, dark Meniscus. There’s a little bit of grey stuff at the end of the dark bone here which is thinning cartilage, but this side has really very little cartilage. The bone is bright which means that the bone is getting bruised and probably small fractures within the bone. And we can see here, the Meniscus is pushed out of the joint, has lots of white in it, so it’s macerated, meaning it has lots of different tears.
And this is a macerated Meniscus with bone cysts. This is what will happen in the long run if a Meniscus is not there. The bone will actually die off which is this little cyst right here. And on these before images, you can see a very nasty-looking Meniscus. It doesn’t really look like a Meniscus. You can see the normal one over here, a nice dark triangle. You can see what’s left of this one after surgery, not much. And then after a stem cell treatment, you can see here that the Meniscus actually has some form to it. It’s not normal by any stretch of the imagination, but it has some form to it. And you can see that the bone cyst went from looking like this to looking like that or much, much less.
On this side, we see a macerated Meniscus with bone cysts from the side view or the Sagittal. We see here, we have some bone cysts here. Again, the same Meniscus we’re looking at now from the side, it looks almost like a untamed dragon. And over here, we can see after the stem cell treatment, it has much better form to it, and those little bone cysts go away.
And then an absent Meniscus with no cartilage whatsoever. We can see the nice normal triangle over here. This one is completely gone, and there’s not a Meniscus there, and there’s no cartilage there either.
Well, thanks for watching. I hope this gives you some sense of what’s on your knee MRI. I always find that an empowered patient is actually the best patient because an empowered patient is one that knows what they’re looking at, that knows what all of this stuff means, is one that actually helps the doctor figure out what the best options are for that patient, so thank you for listening.