Osteitis Pubis
Causes, Symptoms, Treatments, & Other Resources
We see many patients with osteitis pubis every year, but very few have been offered effective osteitis pubis treatment. So what is this diagnosis? What causes it? How can it be easily treated? Let’s dig in.
What Is Osteitis Pubis?
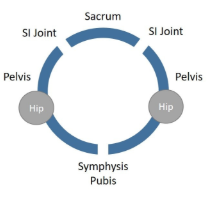
Before we can get into osteitis pubis treatment, we need to understand more about the diagnosis itself. Your pelvis is a ring with two joints in the back called the sacroiliac (SI) joints and one in the front known as the symphysis pubis. That front joint can get inflamed and when that happens the medical term is osteitis pubis. This is also called athletic pubalgia or just pubalgia.
The symphysis pubis is a disc-like fibrous joint that’s meant as a shock absorber (1). It lives in the middle of your groin, just above your genitals, so it can cause pain in the middle of the groin area. That pain can also be referred into the lower abdomen or even into one side or the other in the groin and slightly downward.
To better understand what this diagnosis is and why this all happens, you need to comprehend a bit more about this structure.
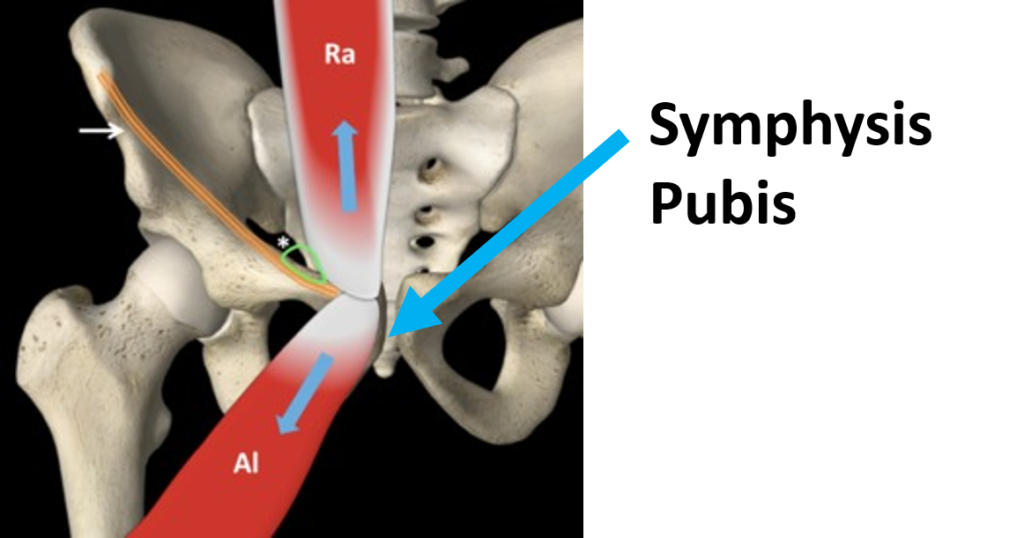
Notice that the “Ra” here is the rectus abdominus, which is the middle-lower abdominal muscle that attaches to the front of the pelvis. This pulls up. The muscle opposing this force is the adductor, which pulls down (“Al” here). This is mirrored on the other side of the symphysis pubis, making a force couple of left-right muscles pulling up on the structure and left-right muscles pulling down.
What Causes Osteitis Pubis?
Now that you know how this area is built, it’s not hard to see how it might get inflamed and pissed off. First, the symphysis pubis joint itself can be unstable due to the ligaments that hold it together being lax or loose. This can happen due to direct trauma or even pregnancy as the baby’s head exits the birth canal.
This problem has also been described in kicking athletes, so overuse can also cause osteitis pubis. However, if that’s the cause, then stopping the kicking for a few days or weeks should heal it. If that doesn’t happen, then read on.
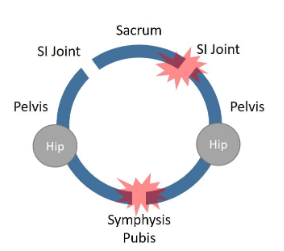
Also realize that as described above, the pelvis is a ring with three joints. Hence, if the sacroiliac (SI) joint ligaments in the back are loose, then the symphysis pubis will get too much wear and tear as well, causing inflammation upfront (see image here). Hence, a problem in the low back can cause a problem is the symphysis pubis.
In addition, as shown above, the abdominal muscles are pulling up on the symphysis pubis and the adductor muscles are pulling down. So asymmetry or weakness in either one can place too much stress on the symphysis pubis and lead to inflammation. In addition, tendinitis in any of these muscle tendons can also do the same thing.
Symptoms of Osteitis Pubis
Pain in the groin and lower abdomen is the most apparent symptom of pubic osteitis. When pressure is applied to the region before your pubic bones, you may experience discomfort or sensitivity.
The pain typically begins gradually but can eventually become constant. It may even impair your ability to stand up and walk normally.
How is Osteitis Pubis Treated?
Physical therapy is usually the first line of treatment (2). Another option is the injection of steroids into the area. The downside there is that high dose steroids can harm tissues, despite being a potent anti-inflammatory. Other options include dextrose prolotherapy and platelet-rich plasma (2,4). Radiofrequency treatment of the nerves has also been reported as well as shock wave therapy (5,6).
Surgery for this disorder is uncommon (3). This usually involves bolting the joint together or removing the joint. Both of these can lead to more problems in the SI joint. If the joint is fused together, this overloads the SI joints and if you remove the joint this causes instability in the rest of the ring, which again hits the SI joints.
How Do We Treat this Problem?
Since there are few randomized controlled trials on any of these treatments, using the research to guide the osteitis pubis treatment isn’t really possible. We have seen great results in these patients by using platelet-rich plasma and dextrose prolotherapy to tighten loose ligaments. These are ultrasound-guided injections into the ligaments that support the symphysis pubis as well as areas of tendinopathy in the adductors or rectus abdominis.
However, just treating the symphysis pubis is often not enough. Remember, this problem can be caused by unstable SI joints that have loose ligaments as well. Hence, using PRP injections with ultrasound guidance to treat those ligaments is often needed. Meaning, treating the whole pelvic ring is usually a smart idea.
The upshot? Osteitis pubis treatment options are out there. In my experience, for patients that fail physical therapy, the way to fix this is to tighten the ligaments around the joint itself and other joints of the pelvic ring (SI joints).
Providers that Help With Osteitis Pubis

Christopher J. Centeno, MD
Christopher J. Centeno, M.D. is an international expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate in orthopedics.
Dr. Centeno is one of the few physicians in the world with extensive experience in the culture expansion of and clinical use of adult bone marrow concentrate to treat orthopedic injuries. His clinic incorporates a variety of revolutionary pain management techniques to bring its broad patient base relief and results. Dr. Centeno treats patients from all over the US who travel to Colorado to undergo innovative, non-surgical treatments. Dr. Centeno has chaired multiple international research-based conferences. He also maintains an active research-based practice, with multiple publications listed in the US National Library of Medicine. Dr. Centeno has also served as editor-in-chief of a medical research journal dedicated to traumatic injury.
Dr. Centeno trained at the Baylor College of Medicine, Texas Medical Center, and the Institute for Rehabilitation Research. He hails from both Florida and New York and currently resides in Boulder, Colorado with his wife and three children.

John Schultz, MD
John R. Schultz M.D. is a national expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate for orthopedic injuries. He is board certified in Anesthesiology and Pain Medicine and underwent fellowship training in both. Dr. Schultz has extensive experience with same day as well as culture expanded bone marrow concentrate and sees patients at the CSC Broomfield, Colorado Clinic, as well the Regenexx Clinic in Grand Cayman. Dr. Schultz emphasis is on the evaluation and treatment of thoracic and cervical disc, facet, nerve, and ligament injuries including the non-surgical treatment of Craniocervical instability (CCI). Dr. Schultz trained at George Washington School of…
Read more
John Pitts, M.D.
Dr. Pitts is originally from Chicago, IL but is a medical graduate of Vanderbilt School of Medicine in Nashville, TN. After Vanderbilt, he completed a residency in Physical Medicine and Rehabilitation (PM&R) at Emory University in Atlanta, GA. The focus of PM&R is the restoration of function and quality of life. In residency, he gained much experience in musculoskeletal medicine, rehabilitation, spine, and sports medicine along with some regenerative medicine. He also gained significant experience in fluoroscopically guided spinal procedures and peripheral injections. However, Dr. Pitts wanted to broaden his skills and treatment options beyond the current typical standards of care.
Read more
Jason Markle, D.O.
Post-residency, Dr. Markle was selected to the Interventional Orthopedic Fellowship program at the Centeno-Schultz Clinic. During his fellowship, he gained significant experience in the new field of Interventional Orthopedics and regenerative medicine, honing his skills in advanced injection techniques into the spine and joints treating patients with autologous, bone marrow concentrate and platelet solutions. Dr. Markle then accepted a full-time attending physician position at the Centeno-Schultz Clinic, where he both treats patients and trains Interventional Orthopedics fellows. Dr. Markle is an active member of the Interventional Orthopedic Foundation and serves as a course instructor, where he trains physicians from around the world.
Read more
Brandon T. Money, D.O., M.S.
Dr. Money is an Indiana native who now proudly calls Colorado home. He attended medical school at Kansas City University and then returned to Indiana to complete a Physical Medicine and Rehabilitation residency program at Indiana University, where he was trained on non-surgical methods to improve health and function as well as rehabilitative care following trauma, stroke, spinal cord injury, brain injury, etc. Dr. Money has been following the ideology behind Centeno-Schultz Clinic and Regenexx since he was in medical school, as he believed there had to be a better way to care for patients than the status quo. The human body has incredible healing capabilities…
Read moreOther Resources
-
Everything You Need to Know about Hip Ligaments
The hip joint is a large ball and socket joint that’s important for lower extremity movement. The joints consist of the articulation of the femur (upper thigh bone/ball) and the acetabulum (the socket). The bones are lined with cartilage and the acetabulum is lined with a fibrocartilage called the labrum. The hip joints, as with…
-
Biceps Femoris Tendonitis Stem Cell Treatment: aka Hamstring Treatment Options
Hamstring injuries are a common sports injury. Dr. Schultz describes what the biceps femoris is, what tendonitis is, what biceps femoris tendonitis is, what causes it, the symptoms, treatment, and biceps femoris tendonitis stem cell treatment options.
-
Pelvic Ligaments: The Uncomfortable Truth You Need to Know!
The pelvis is held together by three principal ligaments: the iliolumbar, sacrotuberous and sacrospinous. Dr. Schultz discusses the causes of pelvic ligament injuries, symptoms, and novel new treatment options.
-
Groin Pain after Hip Replacement: What Is Being Missed?
Your hip replacement surgery was 6 months ago and you are still having pain. Is it normal to have groin pain after total hip replacement? What are the causes of groin pain after total hip replacement? What are the signs of a failing hip replacement? What treatment options exist? Let’s dig in. Is it Normal…
-
8 Reasons for Hip Replacement Failure
Hip replacement surgery replaces a worn out or damaged hip joint with an artificial joint called a prosthesis. The symptoms of hip replacement failure are pain and limited mobility. Dr. Schultz discusses the 8 major causes of hip replacement failure and important treatment options.
-
Levator Scapulae Massage: Options When It Doesn’t Work
The Levator Scapulae is an important neck muscle that lifts and rotates the scapulae. Dr. Schultz discusses the causes of levator scapulae pain and tightness and new, natural treatment options.
References:
(1) Lentz SS. Osteitis pubis: a review. Obstet Gynecol Surv. 1995 Apr;50(4):310-5.
(2) Topol GA, Reeves KD, Hassanein KM. Efficacy of dextrose prolotherapy in elite male kicking-sport athletes with chronic groin pain. Arch Phys Med Rehabil. 2005 Apr;86(4):697-702.
(3) Mehin R, Meek R, O’Brien P, Blachut P. Surgery for osteitis pubis. Can J Surg. 2006;49(3):170–176.
(4) Kraeutler MJ, Garabekyan T, Mei-Dan O. The use of platelet-rich plasma to augment conservative and surgical treatment of hip and pelvic disorders. Muscles Ligaments Tendons J. 2016;6(3):410–419. Published 2016 Dec 21. doi: 10.11138/mltj/2016.6.3.410
(5) Schöberl M, Prantl L, Loose O, et al. Non-surgical treatment of pubic overload and groin pain in amateur football players: a prospective double-blinded randomised controlled study. Knee Surg Sports Traumatol Arthrosc. 2017;25(6):1958–1966. https://www.ncbi.nlm.nih.gov/pubmed/30613167
(6) Masala S, Fiori R, Raguso M, et al. Pulse-dose radiofrequency in athletic pubalgia: preliminary results. J Sport Rehabil. 2017;26(3):227–233. https://www.ncbi.nlm.nih.gov/pubmed/27632851