PRP for Nerve Damage
Platelet-Rich Plasma for Nerve Damage in Denver and Broomfield, CO
Am I a Candidate?Nerve injuries
Peripheral nerves are comprised of various combinations of motor, sensory, and autonomic neurons. Nerve injuries are a common condition with a broad range of symptoms depending on the severity of nerve damage which presents various challenges to patients, ranging from mild discomfort to life-long impairment. PRP for nerve damage has been shown to be effective. Let’s dig in.
Nerve injuries can be classified based on the severity of damage and which structures in the nerve have been damaged. The most severe case is the complete transection of the nerve, called neurotmesis.
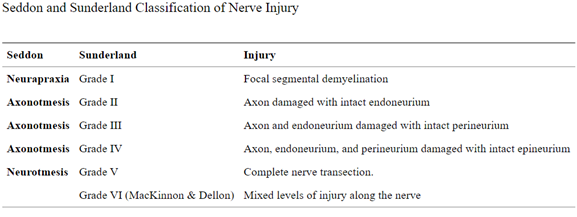
Most common is neuropraxia from acute or chronic compression of the nerve.
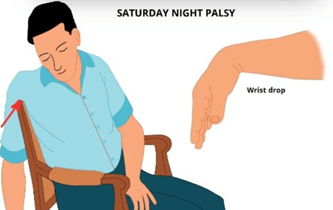
An example of acute compression creating neuropraxia is called “Saturday night palsy.” Typically after a night out and fall asleep with your arm draped over an armrest and in the morning you cannot lift your wrist. This is due to the fact you compressed your radial nerve and now have an acute wrist drop. While recovery can be good once the compression is resolved, symptoms can take weeks, months, and even years to recover!
An example of chronic compression is Carpal Tunnel Syndrome (CTS). Symptoms typically start slow with intermittent numbness but progress to eventually weakness if the nerve continues to be under compression.
Natural nerve recovery and regeneration typically occur at a rate of 1-3mm per day.
Treatment of Nerve Injuries?
Many treatment options exist such as:
- Physical Therapy to help mobilize the nerve tissues. Maximize range of motion, strength and muscular endurance that can facilitate nerve healing
- Other modalities PT can help with
- TENS (transcutaneous electrical nerve stimulation)
- PENS (percutaneous electrical nerve stimulation ) — also called electro-acupuncture
- rTMS (repetitive transcranial magnetic stimulation) uses magnets to send electrical impulses into the brain.
- Other modalities PT can help with
- Medication Management
- Anticonvulsants examples: Gabapentin / Neurontin / Lyrica
- Serotonin and Norepinephrine Reuptake Inhibitors (SNRIs) examples: Cymbalta or Effexor
- Painkillers examples: NSAIDS or Opioids
- Topicals example: lidocaine patches
- Supplementation utilization
- See series
- Oral or Injectable corticosteroids
- Surgical Decompression /Transposition / Nerve Graft
- Less than 50% of such individuals undergo nerve repair surgery, and of those who do, only 40–50% recover good function (1)
BUT the main problem with all these treatment options is, none target or assist in the nerve regeneration process specifically. They are designed to help you tolerate the symptoms while the natural nerve regeneration occurs…None of these treatments actually help the regeneration process of the nerve. That leads us to the question: can PRP help with nerve damage? How does PRP for nerve damage work?
Can Platelet Rich Plasma (PRP) Help Nerves Recover and Repair?
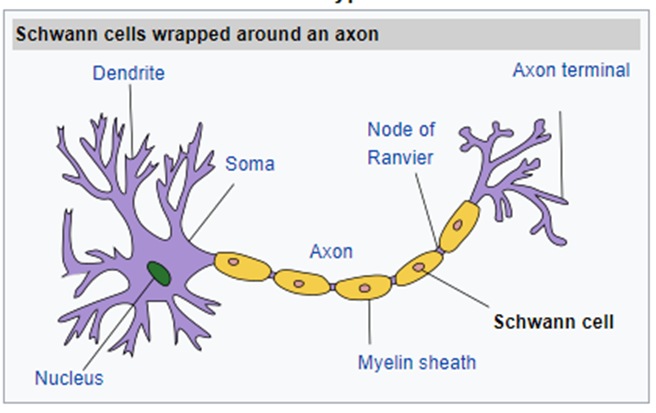
The main cells responsible for coordinating normal nerve recovery after injury are called Schwann cells. After a nerve injury, they release a host of proteins, cytokines, and growth factors to stimulate repair. Over the past 20 years, researchers have been searching for ways to enhance and accelerate the bodies natural healing of peripheral nerves.
Platelets contain a host of factors that promote wound healing, growth, axon regeneration, angiogenesis, and other functions. To understand more about how PRP is made and differences in PRP go here!
Inside platelets, they house a complex cocktail of platelet-released factors is referred to as platelet-derived wound healing factors (PDWHF) and includes:
- Platelet-derived growth factors (PDGF)
- ADP
- Calcium
- Serotonin platelet factor 4
- Fibronectin
- B-thromboglobulin
- Von Willebrand factor (vWF)
- Fibrinogen
- Coagulation factors V and XIII,
- TGF-beta
- Vascular endothelial growth factor (VEGF)
- Epidermal growth factor (EGF)
- Fibroblast growth factor -2 (FGF-2)
- FGF-2, platelet factor 4 (PF4)
- CNTF
- Insulin-like growth factor-1 (IGF-1)
- Platelet derived angiogenesis factor (PDAF)
The highlighted factors are those that have been shown to help enhance and accelerate the natural healing of nerve regeneration (4-10)!
PDGF
Damage nerve cells increase PDGF receptors, PDGF is then able to stimulate release neurotrophic factors = promote the regeneration and enhances nerve axon growth
IGF-1
IGF-1 acts directly on IGF-1 receptors of injured peripheral axons which in turn stimulates myelination, and the degree of neurological recovery – Schwann cells to synthesize of two fatty acids that are the first step in the process of myelination. Also stimulates Schwann cells to promote their proliferation, synthesis and release of axon regeneration-promoting neurotrophic factors.
** The simultaneous application of IGF-1 and PDGF neurons induces more extensive axon regeneration than either = simultaneous release from platelets would enhance the distance axons regenerate across nerve gaps and their myelination.
FGF-2
This influence is in part due to FGF-2 increasing angiogenesis within the conduit bridging the nerve gap, which is essential for axon regeneration.
TGF-beta
TGF-beta is part of a superfamily of multifunctional cytokines and trophic factors. Administration of TGF-beta to dopaminergic neurons in vitro increases neurite outgrowth and in vivo promotes peripheral axon regeneration by triggering the proliferation of nerve Schwann cells, as well as their differentiation and release of neurotrophic factors
TGF-beta can reactivate long-term denervated Schwann cells, triggering them to synthesize and release neurotrophic factors and thus promote axonal regeneration following their long-term denervation. TGF-beta also promotes neurological recovery by inducing synapse formation
VEGF
Angiogenesis is induced by vascular endothelial growth factor (VEGF), a sub-family of growth factors of the PDGF family. Vascularization is critical for and precedes axon regeneration.
EGF
Enhances Schwann cell proliferation, migration and myelination of axons when applied to a damaged peripheral nerve. Its administration also leads to the development of larger diameter axons and enhanced neurological recovery.
Nerve Injuries / Conditions that Can Be Treated with PRP
Baxter’s Neuropathy
It is an entrapment syndrome, like carpal tunnel syndrome in your hand. This is an entrapment of a nerve in your foot, right around your heel, on the inside part compressing a branch of your tibial nerve called your inferior calcaneal nerve, and that is the Baxter’s nerve. Now, the inferior calcaneal nerve is the first branch of the lateral plantar nerve, which is a branch off your tibial nerve. It lives between a muscle belly called your abductor hallucis muscle, as well as the medial calcaneal tuberosity, which is a small bump where a common heel spur occurs in the foot.
Read More About Baxter’s NeuropathyGuyon’s Canal
Guyon canal syndrome is a condition caused by the compression of the ulnar nerve as it passes through the Guyon canal, a narrow passageway located on the palm side of the wrist. This syndrome is commonly seen in people who perform repetitive tasks with their hands or use tools that vibrate, such as jackhammers or drills. Other causes of Guyon canal syndrome may include trauma or injury to the wrist, arthritis, or tumors. Treatment for Guyon canal syndrome may include immobilization of the wrist, anti-inflammatory medications, physical therapy, or– in severe cases– surgery. If left untreated, Guyon canal syndrome can lead to permanent nerve damage, muscle weakness, and loss of function in the affected hand and wrist.
Read More About Guyon’s CanalPeroneal Nerve Injury
The common peroneal nerve branches behind the knee and this could be irritated from any overuse activity, surgery, instability, or any compression on the outside of the knee. Typically, this will present as pain on the outside of the knee radiating towards the baby toe, the calf, and the lateral shin towards the lateral ankle. What Causes Peroneal Nerve Compression? There are many potential causes of peroneal nerve compression, such as overuse activities, surgery, instability, or any compression on the outside of the knee. Trauma and nerve compression, especially caused by a fractured or dislocated ankle, can all cause injury to the peroneal nerve. Causes include:
Read More About Peroneal Nerve InjuryTarsal Tunnel Syndrome (TTS)
Carpal tunnel syndrome is compression of the median nerve at the level of the wrist with resultant hand and wrist pain. Tarsal tunnel syndrome (TTS) is the equivalent in the ankle. What is Tarsal Tunnel Syndrome (TTS)? Also called tibial neuralgia, TTS is compression of the tibial nerve as it passes through the tarsal tunnel at the ankle. The tarsal tunnel is located behind the medial malleolus, the bump on the inside of the ankle.
Read More About Tarsal Tunnel Syndrome (TTS)Thoracic Radiculopathy
Thoracic radiculopathy is a painful medical condition that affects both men and women alike. Pain, paresthesia, decreased sensation, and weakness are the major symptoms. Radiculopathy refers to the whole complex of symptoms that can be caused by irritation or compression of a nerve root in the spine. Thoracic radiculopathy is irritation or compression of a thoracic spinal nerve. Causes of radiculopathy in the thoracic region are thoracic disc injuries, thoracic facet arthritis, ligament thickening, facet cyst, unstable rib attachments, and bone spurs. Diagnosis of thoracic radiculopathy can be difficult….
Read More About Thoracic RadiculopathyTrigeminal Neuralgia
Trigeminal Nerve is a cranial nerve that originates in the brain stem. It has 3 main branches (V1, V2, and V3) that innvate the faces. All have sensory fibers except V3 which has both sensory fibers and motor fibers that go to the muscles of the jaw that allow you to chew and talk. Vascular theory = Artery or vein is compressing the Trigeminal Nerve near the pons, or anywhere along the course of the nerve, injuring myelin sheath and causing erratic hyperactive functioning of the nerve! Symptoms typically occur along the V2 or V3 distribution. Symptoms can be variable with moments of extreme pain.
Read More About Trigeminal NeuralgiaUpside
PRP has a host of growth factors that can stimulate, accelerate and assist in nerve regeneration. At Centeno Schultz Clinic we have invented much of the field of orthobiologics. We have been utilizing PRP for nerve regeneration for last 15 years and if you have been dealing with a peripheral nerve injury and would like to see if you are a candidate for treatment, contact us today! Dr. Pitts explains how we use PRP to treat carpal tunnel syndrome.
Our Doctors that Perform Nerve Hydrodissection with PRP
PRP injection procedures in Denver and Broomfield, Colorado clinics are performed by the following Interventional Orthopedics doctors:

Christopher J. Centeno, MD
Christopher J. Centeno, M.D. is an international expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate in orthopedics. He is board-certified in physical medicine and rehabilitation with a subspecialty of pain medicine through The American Board of Physical Medicine and Rehabilitation. Dr. Centeno is one of the few physicians in the world with extensive experience in the culture expansion of and clinical use of adult bone marrow concentrate to treat orthopedic injuries. His clinic incorporates a variety of revolutionary pain management techniques to bring its broad patient base relief and results. Dr. Centeno treats patients from all over the US who…
Read more
John Schultz, MD
John R. Schultz M.D. is a national expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate for orthopedic injuries. He is board certified in Anesthesiology and Pain Medicine and underwent fellowship training in both. Dr. Schultz has extensive experience with same day as well as culture expanded bone marrow concentrate and sees patients at the CSC Broomfield, Colorado Clinic, as well the Regenexx Clinic in Grand Cayman. Dr. Schultz emphasis is on the evaluation and treatment of thoracic and cervical disc, facet, nerve, and ligament injuries including the non-surgical treatment of Craniocervical instability (CCI). Dr. Schultz trained at George Washington School of…
Read more
John Pitts, M.D.
Dr. Pitts is originally from Chicago, IL but is a medical graduate of Vanderbilt School of Medicine in Nashville, TN. After Vanderbilt, he completed a residency in Physical Medicine and Rehabilitation (PM&R) at Emory University in Atlanta, GA. The focus of PM&R is the restoration of function and quality of life. In residency, he gained much experience in musculoskeletal medicine, rehabilitation, spine, and sports medicine along with some regenerative medicine. He also gained significant experience in fluoroscopically guided spinal procedures and peripheral injections. However, Dr. Pitts wanted to broaden his skills and treatment options beyond the current typical standards of care.
Read more
Jason Markle, D.O.
Post-residency, Dr. Markle was selected to the Interventional Orthopedic Fellowship program at the Centeno-Schultz Clinic. During his fellowship, he gained significant experience in the new field of Interventional Orthopedics and regenerative medicine, honing his skills in advanced injection techniques into the spine and joints treating patients with autologous, bone marrow concentrate and platelet solutions. Dr. Markle then accepted a full-time attending physician position at the Centeno-Schultz Clinic, where he both treats patients and trains Interventional Orthopedics fellows. Dr. Markle is an active member of the Interventional Orthopedic Foundation and serves as a course instructor, where he trains physicians from around the world.
Read more
Brandon T. Money, D.O., M.S.
Dr. Money is an Indiana native who now proudly calls Colorado home. He attended medical school at Kansas City University and then returned to Indiana to complete a Physical Medicine and Rehabilitation residency program at Indiana University, where he was trained on non-surgical methods to improve health and function as well as rehabilitative care following trauma, stroke, spinal cord injury, brain injury, etc. Dr. Money has been following the ideology behind Centeno-Schultz Clinic and Regenexx since he was in medical school, as he believed there had to be a better way to care for patients than the status quo. The human body has incredible healing capabilities…
Read moreReferences for PRP for Nerve Damage:
1. Bozkurt A, Lassner F, O’Dey D, Deumens R, Böcker A, Schwendt T, Janzen C, Suschek CV, Tolba R, Kobayashi E, Sellhaus B, Tholl S, Eummelen L, Schügner F, Damink LO, Weis J, Brook GA, Pallua N. The role of microstructured and interconnected pore channels in a collagen-based nerve guide on axonal regeneration in peripheral nerves. Biomaterials. 2012 Feb;33(5):1363-75. doi: 10.1016/j.biomaterials.2011.10.069. Epub 2011 Nov 13. PMID: 22082619.
2. Menorca RM, Fussell TS, Elfar JC. Nerve physiology: mechanisms of injury and recovery. Hand Clin. 2013;29(3):317-330. doi:10.1016/j.hcl.2013.04.002
10. Li Q, Yao D, Ma J, Zhu J, Xu X, Ren Y, Ding X, Mao X. Transplantation of MSCs in combination with netrin-1 improves neoangiogenesis in a rat model of hind limb ischemia. J Surg Res. 2011 Mar;166(1):162-9. doi: 10.1016/j.jss.2009.08.031. Epub 2009 Sep 23. PMID: 20070983.
Am I a Candidate?
To answer this question, fill out the candidate form below to request a new patient evaluation, and a patient advocate will reach out to you to determine your next steps. Your one-hour, in-office or telemedicine evaluation will be with one of the world’s experts in the field of Interventional Orthopedics.