Surgery for Bulging Disc – Is There an Alternative Option?
Am I a Candidate?A bulging disc, a common cause of back or neck pain, is often treated with invasive surgeries such as discectomy or spinal fusion. However, these surgical options come with their share of risks and long recovery periods. Is there a safer, less invasive alternative? Let’s explore the promise of regenerative medicine in treating bulging disc symptoms.
What Is a Bulging Thoracic Disc?
A bulging disc is a medical condition in which one of the intervertebral discs bulges outwardly. It can also be referred to as a protruding disc. It occurs due to damage or weakness in the disc fibers that provide support.
The thoracic spine is that portion of the spine that is below the neck but above the low back. Often it is referred to as the mid back. A bulging thoracic disc is a condition in which one of the thoracic discs bulges outward.
The disc is composed of two principal parts: annulus fibrosus and nucleus pulposus.
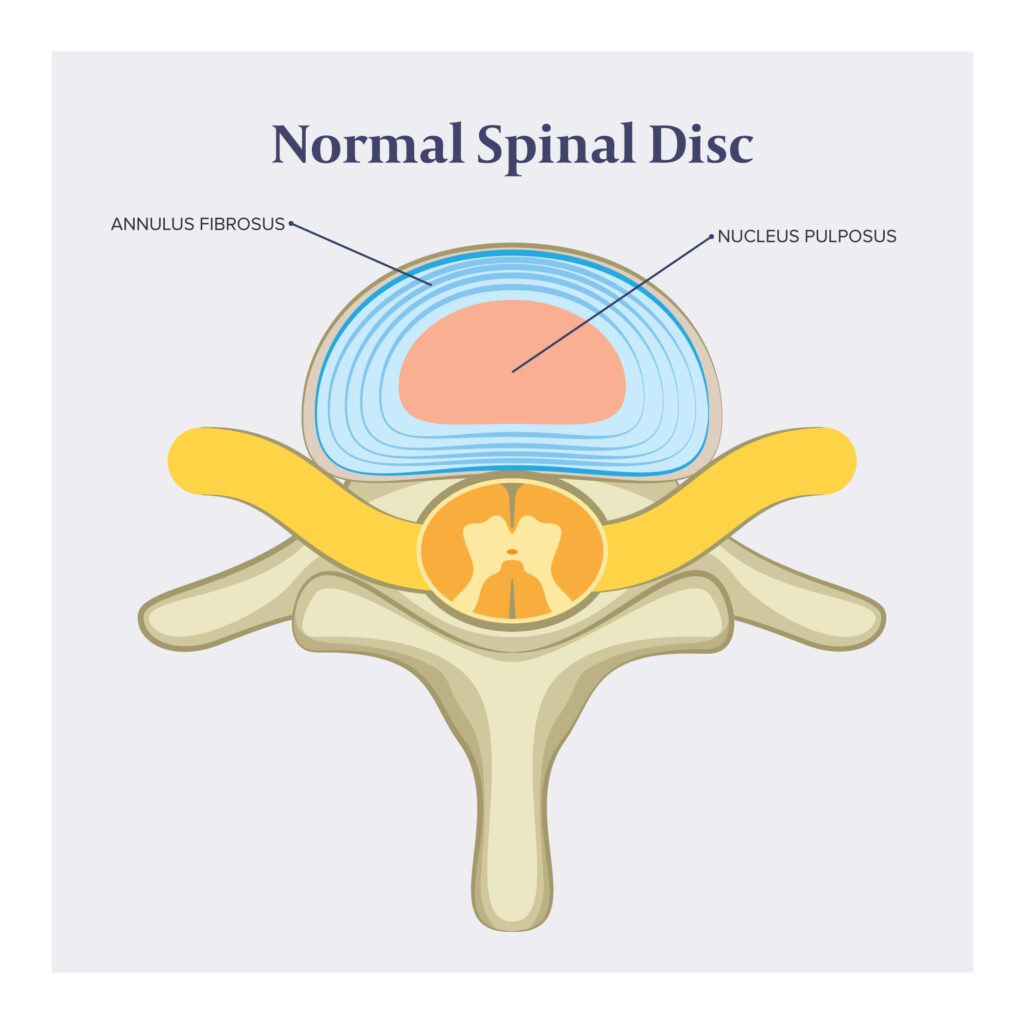
The annulus fibrosus is the thick, outer layer of the disc. It is composed of concentric layers of fibrous tissue that provide strength and stability to the disc. The inner core of the disc is called the nucleus pulposus and has a gel-like consistency. It is composed of water, collagen fibers, and proteoglycans. The nucleus pulposus functions as a shock absorber.
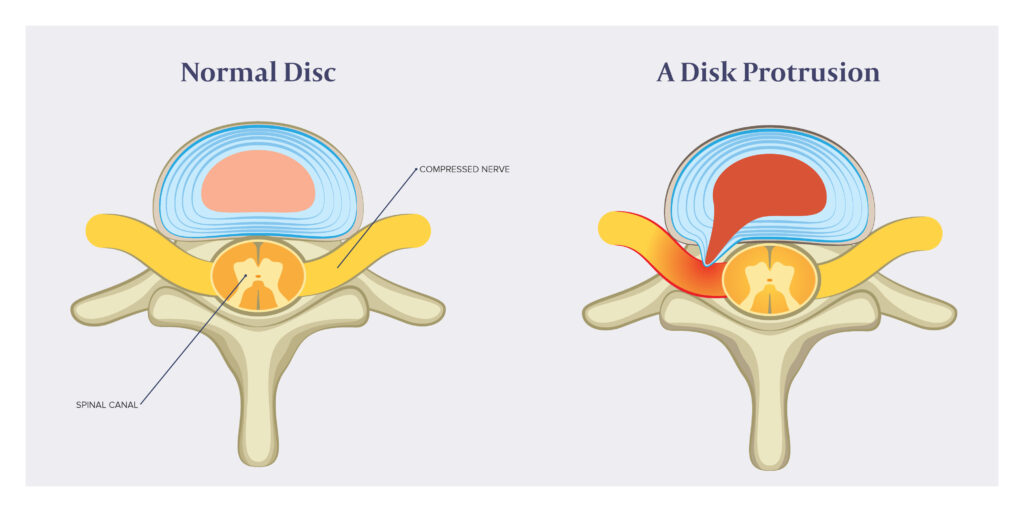
A bulging disc occurs when the outer layer of the disc is damaged or weakened, allowing the inner portion of the disc to push outward. It is important to note that while the gel-like core pushes outward, it is still contained by the annulus fibrosis.
This is in contrast to a disc herniation where the nucleus pulposus pushes outward and extends beyond outer disc fibers and into the spinal canal.
Causes Of Bulging Discs
Bulging discs are typically the result of aging and the gradual wear and tear of your spinal discs over time. However, certain behaviors and conditions can make you more susceptible to developing this condition. Here are some common causes:
- Poor posture: Continuous poor posture can place undue pressure on your spinal column, contributing to bulging discs over time.
- Heavy lifting: Regularly lifting heavy objects, particularly without proper form, can put an excessive amount of pressure on the lower back and spine, leading to disc damage.
- Obesity: Excess body weight puts more pressure on the discs in your lower back, increasing your risk of a bulging disc.
- Sedentary lifestyle: Lack of exercise can lead to weak muscles, which can result in poor support for your spine and a higher risk of bulging discs.
- Genetics: Some people may be genetically predisposed to developing bulging discs.(1)
- Smoking: Smoking reduces the oxygen supply to the discs, causing them to deteriorate more quickly.
- Occupational hazards: Jobs that require repetitive lifting, bending, standing, or driving often contribute to poor spinal health, including bulging discs.
- Aging: As we age, the intervertebral discs lose water content and elasticity, making them more prone to degeneration and bulging.
- Trauma: trauma such as motor vehicle collisions, falls, or contact sports can injure a thoracic disc, resulting in disc protrusions.
Bulging Disc Symptoms
The symptoms of a bulging disc can vary greatly, depending on the location and severity of the condition. Some people may not experience any symptoms at all, while others may experience significant discomfort or pain. Here are some common symptoms:
- Pain: This is often felt in the area of the bulging disc but may also radiate to other areas of the body.
- Numbness or tingling: These sensations can occur in the area of the body served by the affected nerves.
- Muscle weakness: Weakness can occur in the thoracic spine as well as in the upper and lower extremities, depending upon the severity of the thoracic disc bulge.
- Loss of bladder or bowel control: In severe cases, a bulging disc can cause spinal cord irritation or compression, resulting in bowel or bladder dysfunction.
- Stiffness or tightness: This can occur in the neck, back, or limbs.
- Limited mobility: People suffering from a bulging disc may find it difficult to move or bend certain parts of their bodies.
Conventional Thoracic Disc Bulge Surgical Procedures
When conservative treatments for a thoracic disc bulge have failed to provide significant or sustained benefit, patients are often referred for surgical consultation. The goal of surgery is to reduce symptoms and improve overall function.
There are a number of different thoracic spine surgeries. The most common surgeries for the treatment of thoracic disc bulges include:
Discectomy
Discectomy is a commonly performed surgical procedure for a thoracic disc bulge. In this procedure, the protruding portion of the thoracic disc is removed. The goal is to reduce the irritation or compression of the spinal cord or nerves by the thoracic disc bulge.
The surgery can be performed using a traditional open method, or a minimally invasive technique. The open method involves a larger incision and greater disturbance of the surrounding tissues but offers a more direct view and access to the problem area.
Conversely, the minimally invasive technique involves smaller incisions and less tissue disturbance, potentially resulting in quicker recovery times and less postoperative discomfort.
Laminectomy
A laminectomy is another surgical procedure commonly used to treat a thoracic disc bulge. The operation involves removing part or all of the vertebral bone (lamina) to create more space for the nerves and alleviate pressure. This can reduce symptoms such as pain, numbness, or weakness that result from the bulging disc impinging on the nerves.
A laminectomy can be performed using either an open or minimally invasive approach, similar to a discectomy. The spinal ligaments are compromised with the removal of the lamina.
Thoracic Corpectomy
A thoracic corpectomy is a surgical procedure that involves the removal of a vertebral body, along with the adjoining discs, to relieve pressure on the spinal cord and nerves. This procedure is a complex surgery that is rarely utilized for thoracic disc bulges.
It is a complicated, major surgery that often requires the surgeon to access the thoracic vertebrae from the front (anterior) side of the body, which involves navigating around vital organs such as the heart and lungs.
After removing the affected vertebrae and discs, the surgeon will usually replace the removed bone with a bone graft or a metal cage and will insert screws and rods to maintain spinal stability.
Thoracic Fusion
Thoracic fusion is a major surgical procedure often employed when other less invasive methods have proven ineffective. It involves the fusion of two or more vertebrae in the thoracic spine to limit movement and reduce pain. During the procedure, the degenerative or damaged thoracic disc is removed and a bone graft is inserted into the space between the affected vertebrae.
Posterior screws are then inserted into the vertebrae and then connected by rods to stabilize the spine. Over time, the graft and vertebrae grow together, forming a single, solid bone structure. This surgery can effectively eliminate the painful motion caused by the affected discs, providing long-term relief.
There are significant risks and complications associated with thoracic fusion, which include failure to fuse, infection, nerve injury, damage to the heart and lungs, and increased pain.(2)
Endoscopic Thoracic Discectomy
Endoscopic thoracic discectomy is a minimally invasive surgical procedure designed to treat thoracic disc bulges. The surgery involves the use of an endoscope, a thin, flexible instrument equipped with a camera, which allows the surgeon to visualize the area without having to make large incisions.
The procedure helps to reduce recovery times, lessen postoperative pain, and decrease the risks associated with more invasive surgeries. It aims to remove the portion of the bulging disc that is pressing on the nerves, thereby alleviating symptoms.
Why Is Surgery Often Recommended?
Surgical intervention for thoracic disc bulge, despite its inherent risks and complications, presents several potential advantages that can significantly enhance a patient’s quality of life.
Here are some of the prominent benefits of considering surgical options:
- Effective symptom relief: Surgical procedures, such as discectomy and laminectomy, aim to alleviate the pressure exerted on the spinal cord or nerves, thereby reducing pain, numbness, and other associated symptoms.
- Prevention of further damage: By addressing the root cause of the symptoms, surgical intervention can potentially prevent further degeneration and damage to the spinal cord and surrounding nerves. This proactive approach can potentially help safeguard a patient’s long-term health and well-being.
- Improved mobility and functionality: Surgical procedures may improve a patient’s mobility and ability to perform daily tasks. This can lead to enhanced productivity and an overall improved quality of life.
- Faster recovery: Minimally invasive surgical options, such as endoscopic thoracic discectomy, offer shorter recovery times compared to traditional open surgery.
- Customized surgical approaches: Surgical treatments for thoracic disc bulges are not one-size-fits-all. Surgeons consider various factors, including the location and size of the disc bulge, the patient’s overall health, and the presence of other medical conditions, to determine the most suitable surgical plan for each patient.
Potential Risk and Complications of Bulging Disc Surgery
Surgery for thoracic disc bulges is a major surgery that is associated with significant risks and complications. Surgery forever changes the biomechanics of the spine. In many cases, important bones, muscles, ligaments, and tendons are removed, weakening the overall function of the spine.
The most common risks include:
- Nerve damage: nerve damage is a potential risk in thoracic spine surgery, given the complex anatomy and limited space in the thoracic spine. Nerve injury may be transient or permanent.
- Pain and discomfort: Postoperative pain and discomfort are common side effects of surgery. While most patients experience a reduction in their preoperative symptoms, some might have residual pain or develop new pain due to surgical trauma.
- Limited range of motion: Following surgery, patients might experience a limited range of motion, particularly in surgeries like spinal fusion, where two or more vertebrae are joined together.
- Psychological impact: The psychological impact of undergoing surgery should not be underestimated. The stress and anxiety associated with surgery, the recovery period, and the potential for changes in one’s lifestyle can contribute to mental health issues such as depression or anxiety disorders.
- Hardware failure: Surgical hardware may crack or break, in many cases requiring additional surgeries.
- Adjacent segment disease (ASD)(3): Adjacent segment disease is a serious medical condition in which the discs and facet joints above and below a fusion become injured, degenerative, and potentially painful as a result of the original fusion.
How Long Is the Recovery Time for Surgical Procedures?
The recovery timeline following thoracic disc surgery can vary significantly, depending on the specific surgical procedure performed and the individual patient’s overall health.
- Thoracic discectomy: After a thoracic discectomy, patients typically stay in the hospital for one to two days. They may return to light activities within a couple of weeks, but complete recovery can take several months.
- Thoracic corpectomy: This is a more extensive procedure, and patients often require a longer hospital stay—around three to seven days. The pain can be quite high, due to the fact that one or more ribs need to be removed. The recovery period is usually longer than a discectomy, often taking up to six months or more for a complete recovery. A thoracic corpectomy requires posterior fusion to ensure stability of the thoracic spine.
- Thoracic fusion: Following thoracic fusion surgery, patients usually need to stay in the hospital for three to five days. They may need to wear a brace for several weeks to months afterward, to stabilize the spine. Light activities can be resumed in a few weeks, but full recovery often takes six months to a year.
- Endoscopic thoracic discectomy: As a minimally invasive procedure, patients typically have a shorter hospital stay—usually just one to two days—and can return to light activities within several weeks. Full recovery typically takes one to three months.
Please note these are general timelines. Individual recovery can vary based on factors such as age, overall health, medical history, prior surgeries, and adherence to postoperative care instructions. Always consult with your healthcare provider for a more personalized recovery timeline.
Life After Bulging Disc Surgery
Navigating the journey post-surgery is as crucial as the procedure itself. The healing process involves more than just the physical aspects—it’s a holistic progress that encompasses emotional well-being, maintaining spine health, and establishing a robust support network.
Is Surgery the Only Option?
When conservative measures prove ineffective, surgery is not the only option. There are less invasive and risky approaches to promote self-healing of bulging disks, such as injections of orthobiologics. These methods stimulate healing without compromising on safety and efficacy.
PRP Treatment
PRP, or platelet-rich plasma, is a popular regenerative medicine treatment option that utilizes the healing factors in the blood to promote tissue repair. PRP is rich in a number of different growth factors that can improve blood flow and reduce inflammation.
PRP injections have been demonstrated to be superior to steroid injections in the treatment of sciatica.(3) PRP injected into the thoracic spine can potentially reduce the disc protrusion and improve patient function.(4)
Not all PRP injections are the same. At the Centeno-Schultz Clinic, we are committed to the best outcome for our patients. PRP concentration is critical for maximal healing. Patients less than 30 years of age can obtain good clinical and in vitro results from low-concentration PRP (2-3x).
Patients older than 30 years of age require much higher concentrations of PRP (7-20x). This concentration of PRP is only possible due to the flexible lab platform at the Centeno-Schultz Clinic. High concentrations of PRP are not possible at most regenerative clinics, as they utilize bedside centrifuge machines, which are not capable of creating high-concentration PRP.
Bone Marrow Concentrate
BMAC, short for bone marrow aspirate concentrate, is a rich source of stem cells obtained safely and comfortably from the iliac crest, which is the hip bone. Through a specialized process, the bone marrow is carefully concentrated to maximize the presence of healing cells, with stem cells considered the most powerful among them.
Here at the Centeno Schultz Clinic, we take pride in pioneering the use of stem cell injections for orthopedic injuries, making us the first doctors worldwide to do so.
Explore Alternatives Beyond Surgery
In conclusion, while surgery can often provide relief for patients with thoracic disc bulges, it’s essential to bear in mind that it is not the only treatment available. Alternatives like PRP treatment and bone marrow concentrate offer less invasive methods that leverage your body’s healing capabilities.
Both PRP and bone marrow concentrate treatments are without the significant risks, complications, and extensive downtime associated with thoracic spine surgery. Your health journey is personal and unique, and we’re here every step of the way to ensure you make the most informed decision.
John Schultz, MD
John R. Schultz M.D. is a national expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate and PRP for orthopedic injuries. He is board certified in Anesthesiology and Pain Medicine and underwent fellowship training. Dr. Schultz has extensive experience with same day as well as culture expanded bone marrow concentrate and sees patients at the CSC Broomfield, Colorado Clinic, as well the Regenexx Clinic in Grand Cayman. Dr. Schultz emphasis is on the evaluation and treatment of thoracic and cervical disc, facet, nerve, and ligament injuries including the non-surgical treatment of Craniocervical instability (CCI).
References:
- Amin RM, Andrade NS, Neuman BJ. Lumbar Disc Herniation. Curr Rev Musculoskelet Med. 2017 Dec;10(4):507-516. doi: 10.1007/s12178-017-9441-4. PMID: 28980275; PMCID: PMC5685963.
- Prablek M, McGinnis J, Winocour SJ, Reece EM, Kakarla UK, Raber M, Ropper AE, Xu DS. Failures in Thoracic Spinal Fusions and Their Management. Semin Plast Surg. 2021 Feb;35(1):20-24. doi: 10.1055/s-0041-1723832. Epub 2021 May 10. PMID: 33994874; PMCID: PMC8110356.
- Centeno C, Markle J, Dodson E, Stemper I, Hyzy M, Williams C, Freeman M. The use of lumbar epidural injection of platelet lysate for treatment of radicular pain. J Exp Orthop. 2017 Nov 25;4(1):38. doi: 10.1186/s40634-017-0113-5. PMID: 29177632; PMCID: PMC5701904.
- Ling JF, Wininger AE, Hirase T. Platelet-Rich Plasma Versus Corticosteroid Injection for Lumbar Spondylosis and Sacroiliac Arthropathy: A Systematic Review of Comparative Studies. Cureus. 2021 Mar 23;13(3):e14062. doi: 10.7759/cureus.14062. PMID: 33898145; PMCID: PMC8061754.
Am I a Candidate?
To answer this question, fill out the candidate form below to request a new patient evaluation, and a patient advocate will reach out to you to determine your next steps. Your one-hour, in-office or telemedicine evaluation will be with one of the world’s experts in the field of Interventional Orthopedics.