Has Your ACL Ruptured?
Roughly 200,000 people report a tear or sprain of the anterior cruciate ligament (ACL) (1). That’s about 1 in every 3500 individuals. Of all the ligament injuries of the knee, the ACL is the most common. It occurs due to non-contact or rotational forces as opposed to a direct hit to the knee joint.
Has your ACL ruptured? Read on to understand the symptoms, common causes, and treatment options for those with an ACL tear.
What Happens When The ACL Ruptures?
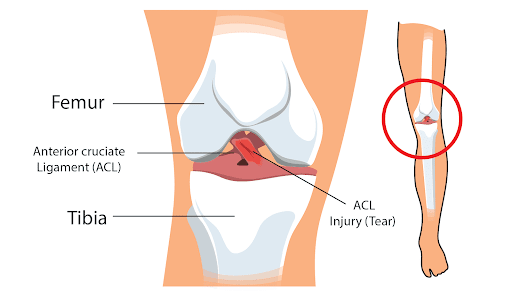
The anterior cruciate ligament stabilizes the knee joint. It is made of connective tissue and collagen. This strong band of fibers extends from the femur to the tibia. It forms an x as it crosses over the posterior cruciate ligament. Hence, they are known as “cruciate” ligaments.
The main function of these ligaments is to prevent excess forward or backward movement of the tibia while the knee flexes or extends. It also provides rotation stability when the knee turns inwards or outwards.
When the knee twists or undergoes too much stress from a sudden jump, fall, or accident, the ACL ruptures. This could be a partial rupture or a complete rupture. There are four grades of ACL tears, and the grades are helpful for doctors as they can guide the treatment.
These grades are:
- Grade I: rupture of individual layers at different levels with hemorrhage that extends to the joint capsule.
- Grade II: rupture with individual layers at different levels with hemorrhage extended from the posterolateral capsule (back and side of the knee).
- Grade III: complete transverse tear of the ligament.
- Grade IV: avulsion of the bone also known as Segond fracture
Symptoms Of A Ruptured ACL
How can you tell if you have a ruptured ACL? Typically, ACL ruptures occur during physical activity where there are sudden changes in the direction of motion.
For example, abrupt stopping, jumping, landing awkwardly, rapid deceleration while running, or a direct blow to the side of the knee. Most individuals report the following signs and symptoms when they rupture their ACL.
Popping In The Knee
Many people who have ruptured their ACL have reported hearing a “pop” right before it happened. The popping sound is followed by the knee giving away or the shun simply buckling, unable to sustain the weight of the femur on top.
Knee popping is not characteristic of a ruptured ACL alone. Other injuries like a meniscal tear or a loose piece of cartilage can also produce this symptom. It’s important to keep in mind that a pop in the knee can be due to a ruptured ACL and needs to be seen immediately by an orthopedic doctor especially if it’s accompanied by pain and swelling.
Pain And Swelling
You will experience sharp pain at first when the ligament ruptures. The knee joint will swell within 24 hours of the injury. Walking will worsen the pain. The pain is continuous and may be slightly relieved at rest. The joint will be warm and tender to touch. This pain may extend along the shin downwards and upwards along the femur.
Range Of Motion Is Lost
Due to the ACL rupture, the knee joint is extremely unstable. Any attempt to bear weight will cause the knee to give out. Depending on the degree of the tear, the knee may not have a complete range of motion. In complete ACL ruptures, the loss of motion in total. This means that the individual cannot flex, extend or rotate the knee joint at all.
Common Causes Of Ruptured ACL
ACL ruptures commonly occur during sports activities. However, three mechanisms result in ACL injuries. These are:
- Direct contact
- Indirect contact
- Noncontact
Direct Contact Injuries
Direct contact injuries occur when either someone or something strikes the knee directly. This could be during a motor vehicle accident or contact sports.
Indirect Contact Injuries
Indirect contact injuries happen when someone or something strikes another part of the body like the tibia or the femur. This transfers excessive force across the knee joint leading to a rupture of the ACL. An example of this would be a direct high-velocity hit to the thigh or a blow to the shin.
Non Contact Injuries
Noncontact injuries occur when there’s a deceleration or directional change. This causes a pivoting force to be applied to the knee. However, because the knee is moving in a different direction, there is a mismatched neuromuscular firing of the structures around the knee.
This leads to the translation of the tibia on the femur, which is very characteristic of ACL failure. Noncontact mechanisms account for 60%–70% of injuries to the ACL (2).
Examples of this would be sudden stop while running or running forwards and then abruptly switch to sideways.
Examination And Diagnosis
After taking a complete history to understand how you sustained the injury and the timing of the injury, the doctor will do a thorough physical exam.
Physical Exam
The physical exam will evaluate the mechanism of injury and how it affects your daily functioning. The doctor will also assess your knee for joint stability, mobility, and strength, via palpation.
He or she will also check for the possibility of other associated injuries such as fractures and dislocations. The doctor will also check the contralateral knee to compare the difference between the two joints.
Special Maneuvers
The physical exam also involves the use of special maneuvers to isolate and diagnose injury to the ACL. These tests include the anterior drawer test, the pivot shift test, and the Lachman test. These tests are usually done for any injury to the ACL.
- The anterior drawer test: To do this test, the patient must lie down supine and flex the injured knee to 90 degrees. The foot is planted on a flat surface. If the patient is unable to do so, the clinician may surprisingly sit on the foot to keep it planted.
He or she will then hold the tibia with both hands and pull it gently anteriorly. The test is positive if there is instability and the joint moves too much anteriorly signifying a tear of the ACL. They will repeat this test on the other knee as this test is also positive in people with lax ACLs. This test is very good to diagnose chronic ACL injuries. - The pivot shift test: For this test, the patient lies down in a supine position. The doctor will hold the patient’s lower leg. He or she then extends the knee and flexes the hip to 20 degrees.
This is done gradually. The doctor then rotates the tibia internally with one hand and starts adding external pressure from the outside of the knee using the other hand. In the case of the ACL tear, the external pressure destabilizes the affected knee causing it to give way.
If the tibia moves backward or the doctor feels a clunk, the test is positive. As you can tell, this is a very difficult test. Some patients are too guarded and will prevent the doctor from doing it because of the pain and the feeling of instability. However, if this test is positive, it is very diagnostic for an ACL tear. - Lachman test: In this maneuver, the patient lies down supine and flexes the knee to 30 degrees. The doctor will stabilize the femur with one hand and pull the tibia towards them with the other hand. If there is too much anterior motion, then the test is positive. This is also a very characteristic test for ACL rupture.
In addition to this, there are other special maneuvers performed to rule out injuries to other knee ligaments such as the medial or lateral collateral ligament, posterior collateral ligament, or injuries to the meniscus. Doctors may perform these additional tests, if they suspect concomitant injuries to other ligaments as well.
Imaging
ACL injuries are diagnosed clinically with a good history and physical examination. However, imaging is necessary to confirm the diagnosis and rule out any other associated injuries or fractures.
- MRI: MRI is the most important modality to diagnose ACL ruptures. On an MRI, the presence of primary signs like edema, discontinuous fibers, an increased signal of the ACL, and alteration of Blumensaat’s line which is the expected course of the ACL point to a tear.
A fracture, bone marrow edema, tears to other ligaments, and the movement of the tibia more than 7mm away from the femur are secondary signs of an ACL tear. - Arthrography: Knee arthrography is also used to diagnose ACL ruptures. It can differentiate complete ruptures from partial tears and chronic tears. It is considered the gold standard test. However, it is not used as often because it requires anesthesia and is invasive.
- Xray’s: X-rays are not generally used to diagnose ACL ruptures. They are helpful to rule out fractures. In younger patients, X-rays can reveal where the tibial attachment of the ligament has been torn or avulsed.
Avulsion fractures at the fibula and joint effusions can also be seen on an X-ray. One characteristic sign known as the deep lateral sulcus sign can be seen on an X-ray. It is a notch on the lateral femur and can aid in the diagnosis of ACL injury. - Computed tomography: CT is not helpful to diagnose ACL injuries, but it can confirm the presence of an intact ACL.
Common Treatments For Ruptured ACL
The treatment of a ruptured ACL depends on the severity of the injury. The decision to treat this operatively or non-operatively depends on how severe the injury is. The treatment options and rehabilitation course are discussed with the orthopedic doctor and the physiotherapist after the diagnosis is confirmed.
RICE Rule
All acute injuries are treated with R.I.C.E. That stands for Rest, Ice, Compression, and Elevation. The rest is to prevent any weight-bearing activity which can exacerbate the pain and worsen the injury. Ice will constrict the blood vessels and lessen blood flow for a brief period.
Compression is helpful to decrease the swelling and elevation can allow the blood to return to the heart easily without being pooled in the leg. This should be done as soon as you sustain a knee injury irrespective of the cause.
Rehabilitation
The rehabilitation during the acute stage irrespective of whether surgery will be done or not focuses on regaining range of movement, strength, stability, and proprioception. Crutches or a knee immobilizer are given to some individuals.
Some exercises of the rehab program include passive knee extension where the physiotherapist can provide a passive knee extension both manually and with knee exercises to achieve full extension. This can also be achieved by heel props, patellar self-mobilizations, and prone hang exercise.
Flexion of the knee is obtained by doing the passive knee bend, gentle kicking exercises, wall slides, and heel slides. Other exercises include glute exercises while lying on the side and ankle flexions.
Young active adults experience recurrent instability and development of meniscal injuries when they undergo conservative management with rehabilitation only. Structured rehab is usually done during the acute stage of the injury or post-surgery.
A Cochrane review of trials of adult patients using structure rehab alone versus ACL reconstruction (ACLR) followed by rehab showed that the majority of patients needed ACLR within a few years (3).
Surgery
There are many ways to repair an ACL tear surgically. In fact, surgery is considered to be about 95% successful. Some of them are listed below.
Reconstruction
ACLR is now done by debriding the torn ends of the ACL and using a graft to reconstruct the ligament. Graft reconstruction can use the hamstring tendon (HT), bone-patellar tendon-bone (BPTB), or quadriceps tendon (QT). These tendons can anatomically and functionally serve as the ACL.
The graft can come from the patient (autograft) or a cadaver (allograft). There are many types of reconstruction including anatomic, nonanatomic, single, and double-bundle techniques.
Traditional ACLRs are nonanatomic where doctors place the graft outside of the normal insertion of the ACL. Currently, the anatomic ACLR is performed where doctors try to restore the exact insertion of the graft on both the tibia and the femur. The type of surgery varies based on the anatomy of the person, the pattern of injury, and the physical demands of the person.
Tunnel Drilling
This surgical technique is falling out of practice. Here, the reconstruction is done by drilling femoral tunnels. Outcomes are better when surgeons use an outside technique or use guides through a portal.
A few things to know about Grafts:
- Fixation types: Graft surgery also differs based on how the graft is fixed. Is it via an aperture, button graft, or screw? There are many types of screws. The two main types are metal and bioabsorbable screws. Each of them has its pros and cons.
Biologic screws can widen the femoral tunnel. Metallic screws prevent advanced imaging of the knee postoperatively. - Graft Choice: The graft is chosen based on the age of the patient, their level of activity, and their skeletal maturity. The failure rate is higher when using cadaveric grafts. For athletes, an autograft is best. Cadaveric grafts work well in individuals who are older and less active, provided they follow a strict rehab program over 8-12 months.
Primary Anterior Cruciate Ligament RepairOn the flip side, the HT autograft has a higher rate of infection, and BPTB autografts are accompanied by knee pain. Quadriceps autografts have also shown to be a good alternative since they have good strength and reliable long-term outcomes.
Primary Anterior Cruciate Ligament Repair
Primary ACL repair has been associated with poor outcomes. However, there’s been a growing push to preserve the ACL. With advances in regenerative medicine and tissue engineering, it is now possible to have more success with this form of surgical repair. Early mobilization in rehab can also help improve recovery after this procedure.
In primary ACL repair, arthroscopic repair is possible with newer devices. The stiffness of the joint is mitigated by a structured rehabilitation program. The only problem is that it comes with a 15% failure rate.
Choosing the right surgery is very important. A skilled orthopedic surgeon can assess the tear and quality of the tissue before proceeding. Those patients with excellent tissue quality can be good candidates for primary ACL repair. Those with distal teras and concomitant ligament injuries should be treated with ACLR.
Internal Bracing
While ACLR and primary ACL repair are treatment options, another emerging alternative is the use of an internal brace. This internal brace protects the graft during the early stages of rehab so a person can return to activity without the risk of re-injury.
Doctors use collagen coated; ultrahigh molecular weight polyethylene/polyester suture tape as an internal brace. It provides stability and protects the graft. It functions as a load-sharing device while still allowing the graft to experience enough stress to become a ligament.
There have been concerns about its safety, but clinical trials have shown that after an internal brace, patients had near normal knee function.
In general, when it comes to surgery, primary ACL repair is better when it comes to revision. A failed repair is treated like a primary ACLR.
However, a failed reconstruction is fraught with complications such as mispositioning of the tunnel, a widened tunnel, issues with the screws, and the need for bone grafting. 6% of individuals will need a revision procedure.
Those who need re-revision also have concomitant internal derangement of the menisci. Therefore, surgery needs to be thought through by the patient before they sign up for it.
Recovery Time
It takes anywhere between eight to twelve months to fully recover after ACLR. For those who want to return to competitive sport, it can take anywhere between six to twelve months. This is because the graft still needs time to replicate the native ligament by getting accustomed to neurosensory function, regional bone mineral density, and physiology.
Physiotherapists need to re-establish strength, power, and functional performance. This needs to be balanced with the contralateral knee, especially in athletes. The rehab is probably the most time-consuming but integral part of the recovery process. It reestablishes balances, proprioception, and strength. Additionally, it can take about 18 months for the graft to fully incorporate.
Pain Management
Unfortunately, surgery is accompanied by pain. This pain can be controlled with NSAIDs like diclofenac, ketorolac, celecoxib, and ibuprofen. Studies have shown that ketorolac and ibuprofen were the most effective for pain control and also reduce opioid consumption.
It’s important to remember that certain pain medicines like celecoxib can also inhibit tendon-to-bone blood healing. However, NSAIDs are safer and reduce nausea and vomiting as well.
Other pain medicines are ketamine, tranexamic acid, gabapentin, sedatives like zolpidem, and corticosteroids.
Reinjury Risk
There is a very high risk for re-injury with surgery that requires another revision procedure. This risk is higher in younger female athletes. It also depends on the type of surgery and the concomitant ligament damage sustained. Premature return to activity can lead to failure of the graft.
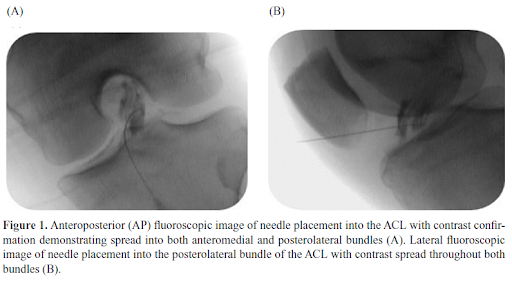
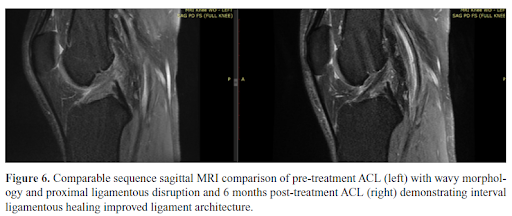
Regenexx
At Centeno-Schultz Clinic (clinical headquarter for Regenexx), we invented a way to inject an injured ACL under xray guidance. Over the last 15 years, have perfected this injection and then researched the effectiveness of bone marrow concentrate injection into torn ligaments to see if we were able to heal the ligament without the need for more invasive surgery. Started with a small case series of 10 patient (5) and then expanded to 29 patients (6). Based on our results over 70% of patients were able to heal their ACL. Next, we conducted a higher level research study, randomized control trial placing ACL tears in either treatment groups or physical therapy (7). We were able to definitively demonstrate that >70% are able to heal without surgery!
Being able to heal your ACL injury without surgery is a big deal! See below on all the advantages of being able to save your ACL.
Advantages Of Non-Surgical Alternatives
There are many advantages of choosing non-surgical alternatives. Half the patients who do choose them tend to fare well for life without the need for surgery. Early rehabilitation before and after treatment is a key component of this.
Non-surgical treatment options spare patients a lot of pain and dependence on pain medication. There are also fewer risks for reinjury since the person is using their native ligaments.
Biologic agents can work on the repair and healing of the native ligament without the need for a complicated procedure. 77% of patients have demonstrated better ligament integrity with bone marrow concentrate injections (40).
Being able to save your own ACL will prevent the development of osteoarthritis that happens in 70-80% of those with traditional ACL-reconstruction as well as prevent future injuries such as meniscus tears or ACL tears to the other knee!
Risk Factors
Certain people are at greater risk for ACL ruptures. This includes:
- Females: Women are at greater risk for ACL tears primarily due to anatomical and physiological reasons. Women tend to have weaker hamstrings. They also use the quadriceps muscle to decelerate.
This places a lot of stress on the ACL as these muscles are less effective in preventing the forward movement of the tibia when compared to the hamstring muscles. Female athletes also tend to place their knees outwards when they change directions which stretch the ACL ligament.
It has been postulated that estrogen can also affect the flexibility of the ligaments. Although, how this happens is unclear and has never been scientifically proven. - Higher BMI: Overweight and obese patients tend to be more susceptible as the increased weight places extra stress on the ACL.
- Organized sportspersons: People involved in sports and martial arts tend to jump, run and stop abruptly at high speed which can place additional stress on the ACL.
- Medical conditions: Individuals with medical conditions like subtalar joint overpronation, generalized ligamentous laxity, and decreased neuromuscular control of the knee tend to have more risk of an ACL rupture. This is because the ligaments are weak and proprioception (the sensation of knowing where the join is) is poor.
Prevention For ACL Ruptures
Knowing the risk factors, is there a way to prevent ACL ruptures? Yes. You can prevent rupture of the ACL. Two important ways to do this are neuromuscular training and proprioceptive training.
Neuromuscular training can lead to a 27% reduction in the rate of a knee injury. Proprioceptive training can reduce knee injury rates by 51%. This is highly recommended for young female athletes.
- Neuromuscular training: This is a program that includes general (fundamental) and specific (sports-directed) movements, and strength and conditioning exercises. Some of them are resistance exercises, dynamic stability movements, exercises for balance, core strength, plyometric, and agility exercises.
- Proprioceptive training: This is a program that focuses on improving proprioceptive function. It uses somatic and sensory signals like vision to improve sensorimotor function. This includes balance exercises, tai chi, active movement, and somatosensory stimulation.
- Targeted and Balances Strength training: If you are building muscle, it’s very important to develop all muscle groups evenly. Target each muscle group without neglecting a major group.
- Posture and Technique: Practice good form and technique in sports. This will stabilize your knee and evenly distribute your weight no matter what activity you are involved in.
- Always warm up: Warm up and stretch before any physical activity. This stretched the muscles and ligaments and prepared them for what was to come. It also improves circulation and blood flow. Never perform any strenuous activity when the muscles are tired. It makes them susceptible to injury.
- Use Proper Footwear The right footwear can give you good balance and prevent any falls. Always plant your feet on the ground while you are doing sports or doing any physical activity.
Further Complications If Left Untreated
If ACL tears are left untreated, then there is a very high likelihood of developing osteoarthritis. Without the supportive ACL, the cartilage between the tibia and the femur begins to break down. The ACL protects the menisci. Without this protection, the menisci also break down. Blood can also pool within the joint following the acute injury.
Partial tears will worsen and become full tears. The knee will lose its range of motion and will be extremely painful. The knee stiffness and instability can worsen the joint’s condition.
Eventually, you will need a total joint replacement if this is not addressed on time.
Which Doctors To Consult With
If you or a loved one has been diagnosed with a ruptured ACL, chances are you have been referred to a surgeon. Surgery may have been the best recommendation. As you have seen, there are many non-surgical options when it comes to an ACL tear.
Surgery has many long-term risks including corrective or remedial surgeries. Additionally, it is not a permanent solution. Before you decide to undergo surgery, schedule a telemedicine consultation with one of our board-certified, fellowship-trained doctors.
Our physicians will explain to you the non-surgical, regenerative treatment options available.

Christopher J. Centeno, MD
Christopher J. Centeno, M.D. is an international expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate in orthopedics. He is board-certified in physical medicine and rehabilitation with a subspecialty of pain medicine through The American Board of Physical Medicine and Rehabilitation. Dr. Centeno is one of the few physicians in the world with extensive experience in the culture expansion of and clinical use of adult bone marrow concentrate to treat orthopedic injuries. His clinic incorporates a variety of revolutionary pain management techniques to bring its broad patient base relief and results. Dr. Centeno treats patients from all over the US who…
Read more
John Schultz, MD
John R. Schultz M.D. is a national expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate for orthopedic injuries. He is board certified in Anesthesiology and Pain Medicine and underwent fellowship training in both. Dr. Schultz has extensive experience with same day as well as culture expanded bone marrow concentrate and sees patients at the CSC Broomfield, Colorado Clinic, as well the Regenexx Clinic in Grand Cayman. Dr. Schultz emphasis is on the evaluation and treatment of thoracic and cervical disc, facet, nerve, and ligament injuries including the non-surgical treatment of Craniocervical instability (CCI). Dr. Schultz trained at George Washington School of…
Read more
John Pitts, M.D.
Dr. Pitts is originally from Chicago, IL but is a medical graduate of Vanderbilt School of Medicine in Nashville, TN. After Vanderbilt, he completed a residency in Physical Medicine and Rehabilitation (PM&R) at Emory University in Atlanta, GA. The focus of PM&R is the restoration of function and quality of life. In residency, he gained much experience in musculoskeletal medicine, rehabilitation, spine, and sports medicine along with some regenerative medicine. He also gained significant experience in fluoroscopically guided spinal procedures and peripheral injections. However, Dr. Pitts wanted to broaden his skills and treatment options beyond the current typical standards of care.
Read more
Jason Markle, D.O.
Post-residency, Dr. Markle was selected to the Interventional Orthopedic Fellowship program at the Centeno-Schultz Clinic. During his fellowship, he gained significant experience in the new field of Interventional Orthopedics and regenerative medicine, honing his skills in advanced injection techniques into the spine and joints treating patients with autologous, bone marrow concentrate and platelet solutions. Dr. Markle then accepted a full-time attending physician position at the Centeno-Schultz Clinic, where he both treats patients and trains Interventional Orthopedics fellows. Dr. Markle is an active member of the Interventional Orthopedic Foundation and serves as a course instructor, where he trains physicians from around the world.
Read more
Brandon T. Money, D.O., M.S.
Dr. Money is an Indiana native who now proudly calls Colorado home. He attended medical school at Kansas City University and then returned to Indiana to complete a Physical Medicine and Rehabilitation residency program at Indiana University, where he was trained on non-surgical methods to improve health and function as well as rehabilitative care following trauma, stroke, spinal cord injury, brain injury, etc. Dr. Money has been following the ideology behind Centeno-Schultz Clinic and Regenexx since he was in medical school, as he believed there had to be a better way to care for patients than the status quo. The human body has incredible healing capabilities…
Read moreMore Resources For This Condition
-
ACL Tear Treatment Without Surgery: Our New Publication!
It all happened so suddenly. You were running down the field and made a quick cut. You heard an audible pop followed by searing knee pain and then collapsed to the ground. Your doctor thinks your tore your ACL and has referred you to a surgeon. What is the Anterior Cruciate Ligament? What is the…
-
How Likely Is a Second ACL Tear On the Same Knee?
Anterior Cruciate Ligament Injuries and Treatments The ACL (anterior cruciate ligament) is an important knee stabilizing ligament. It prevents the tibia from moving too much frontward (anterior translation) and twisting too much (internal rotation). It is under most stress with landing from a jump, or a planted foot with twisting, and this is how it…
-
Regenexx ACL Repair vs Reconstruction Surgery for Knee ACL
Regenexx ACL Repair vs Reconstruction Surgery for Knee ACL Today I’d like to highlight a patient named Joe’s story. Joe is unique in that he has had the non-surgical Regenexx Perc-ACLR procedure which uses your own cells injected via a small needle, and a surgical ACL reconstruction, so he can compare the two. So let’s…
-
ACL Tear Treatment Without Surgery
The Anterior Cruciate Ligament (ACL) is a key stabilizer in the knee that is frequently injured. Dr. Schultz discusses what an ACL is, the major causes of tears, symptoms associated with a tear, what ACL surgery is, its risk, and effective ACL tear treatment without surgery. He shares a recent clinical success with a 14y/o…
-
ACL MRI Evidence for the Perc-ACLR
Dr. Centeno goes through 23 examples of ACL MRI that show the superiority of the Regenexx Perc-ACLR. Transcript Hi, it’s Dr. Centeno. And today we’re going to go over MRI evidence that the Regenexx Perc-ACLR procedure heals ACL tears. So, we invented ACL stem cell injections at the Centeno-Schultz Clinic, which is the headquarters of…
-
How to Tell if You Tore Your ACL?
Knee pain can stop you in your tracks, and a common cause of knee pain and instability is an ACL tear. What is an ACL? What causes an ACL to tear? How to tell if you tore your ACL? What are the signs and symptoms of an ACL tear? Can you still walk if you…
References:
- G. Moulton, Travis Lee Turnbull, Nicholas I. Kennedy, Robert F. LaPrade, 112 -Functional Bracing for Anterior Cruciate Ligament Injuries: Current State and Future Direction, Editor(s): Chadwick C. Prodromos, The Anterior Cruciate Ligament (Second Edition), Elsevier, 2018, Pages 459-461.e1, ISBN 9780323389624, https://doi.org/10.1016/B978-0-323-38962-4.00112-0.
- Boden BP, Dean GS, Feagin JA Jr, Garrett WE Jr. Mechanisms of anterior cruciate ligament injury. Orthopedics. 2000;23(6):573-578. doi:10.3928/0147-7447-20000601-15.
- Monk AP, Davies LJ, Hopewell S, Harris K, Beard DJ, Price AJ. Surgical versus conservative interventions for treating anterior cruciate ligament injuries. Cochrane Database Syst Rev. 2016;4(4): CD011166. Published 2016 Apr 3. doi: 10.1002/14651858.CD011166.pub2
- Hevesi M, LaPrade M, Saris DBF, Krych AJ. Stem Cell Treatment for Ligament Repair and Reconstruction. Curr Rev Musculoskelet Med. 2019 Dec;12(4):446-450. doi: 10.1007/s12178-019-09580-4. PMID: 31625113; PMCID: PMC6942090.
- Centeno CJ, Pitts J, Al-Sayegh H, Freeman MD. Anterior cruciate ligament tears treated with percutaneous injection of autologous bone marrow nucleated cells: a case series. J Pain Res. 2015 Jul 31;8:437-47. doi: 10.2147/JPR.S86244. PMID: 26261424; PMCID: PMC4527573.
- Centeno C, Markle J, Dodson E, Stemper I, Williams C, Hyzy M, Ichim T, Freeman M. Symptomatic anterior cruciate ligament tears treated with percutaneous injection of autologous bone marrow concentrate and platelet products: a non-controlled registry study. J Transl Med. 2018 Sep 3;16(1):246. doi: 10.1186/s12967-018-1623-3. PMID: 30176875; PMCID: PMC6122476.
- Centeno, C., Lucas, M., Stemper, I., & Dodson, E. (2022). Image Guided Injection of Anterior Cruciate Ligament Tears with Autologous Bone Marrow Concentrate and Platelets: Midterm Analysis from A Randomized Controlled Trial. Biologic Orthopedics Journal, 3(SP2), e7-e20. https://www.biologicortho.com/index.php/BiologicOrtho/article/view/24