Surgery for a Herniated Disc
Am I a Candidate?A disc herniation is a medical condition in which the thick outer fibers of the disc are injured, allowing the gelatinous center to push outward, creating pain, restriction in range of motion, and dysfunction.
When unresponsive to conservative care and injections, surgery is often recommended. There are several different types of surgery for herniated discs, which are discussed below.
Causes of a Herniated Disc
The disc is composed of two principal parts: the annulus fibrosus, which is the thick outer fibers of the disc, and the nucleus pulposus is the gelatinous center, which acts as a shock absorber during movement.
A disc herniation occurs when there is weakness or injury of the thick outer fibers (annulus fibrosus), thereby allowing the gelatinous center to push outward. The disc material can extend into the spinal canal, causing pain and narrowing.
It can also irritate or compress a nerve, causing radiating pain down the arm or leg. The contents of the disc are very toxic, causing pain and inflammation.
The incidence of a herniated disc is approximately 5-20 cases per 1000 adults. It is most common in individuals in the third to fifth decade of life.1 Men are more likely to suffer a herniated disc than women.
The most common cause of disc herniation is degeneration, where the disc becomes less hydrated and weakens. Other biologic factors thought to contribute to the disc herniation include:
- Less water retention in the disc2
- Increased type 1 collagen3
- Degradation of the collagen and extracellular matrix material
The second most common cause of disc herniation is trauma. A sudden injury or trauma to the spine such as a fall, car accident or lifting a heavy object incorrectly can lead to disc herniation.
These events can cause excessive pressure on the discs, leading to tears and herniation.
Other factors that can cause disc herniation are:
Repetitive strain: activities that involve repetitive movements or heavy lifting can increase the risk of disc herniation. Over time, the cumulative stress can lead to degeneration and disc herniation.
Genetics: Some individuals may be genetically predisposed to disc problems.
Obesity: Increased body weight can place additional stress on the spine and increase the risk of disc degeneration, spinal stenosis and disc herniation.5
Smoking: Smoking has been associated with increased risk of disc degeneration and disc herniation. It is thought to reduce blood flow and increase stress response on the disc.6
Types of Herniated Discs and Associated Surgery
Disc herniation can occur in various parts of the spine. The major types of disc herniations are based upon their location within the spine.
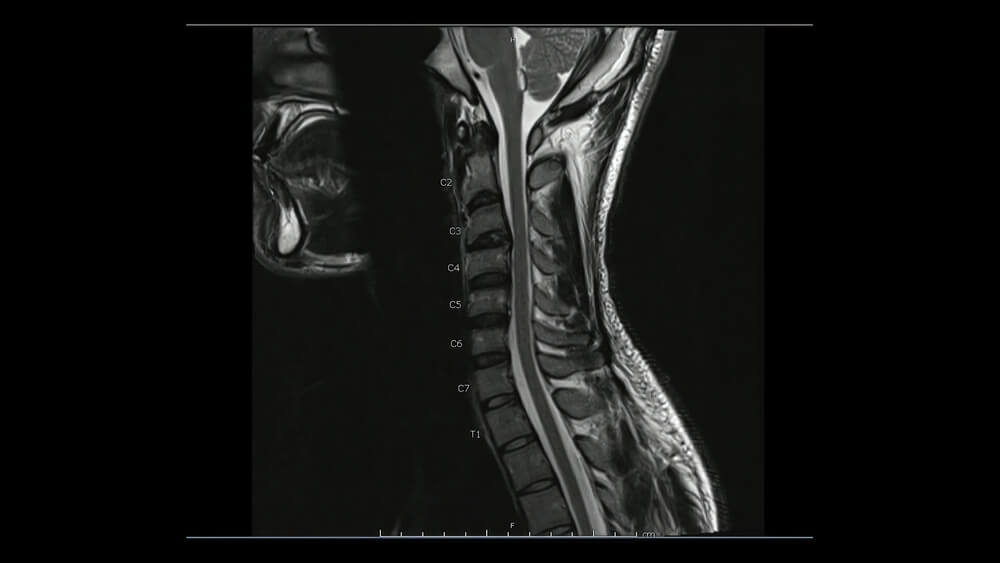
- Cervical disc herniation: This type of herniation occurs in the neck. Symptoms can vary depending upon the size and location of the disc herniation.
- Thoracic disc herniation: The thoracic spine, also known as the mid back, is that portion of the spine that is below the neck but above the low back. Thoracic disc herniations are relatively uncommon compared to lumbar and neck disc injuries. It is estimated that only 0.25-1% of all disc herniations take place in the thoracic region.7
- Lumbar disc herniation: Lumbar refers to low back and is the most common type of disc herniation.

- Central disc herniation: In a central disc herniation, the disc material is extruded towards the midline (center) of the spinal canal. This type of herniation can exert pressure on the spinal cord and potentially result in symptoms such as impaired mobility, balance issues, and dysfunction of the bowel or bladder.
- Lateral disc herniation: A lateral disc herniation occurs when the disc material protrudes to the side of the spinal column instead of the midline, which is the case with a central disc protrusion.
- Posterolateral disc herniation: This particular type of herniation takes place towards the posterior and lateral aspects of the spinal canal, potentially impacting both the spinal cord and the nerve roots.
Several factors determine the specific type of surgery for a herniated disc, including the location, size of the herniation, presence or absence of compression on the spinal cord or exiting nerve root, and the patient’s symptoms. The following are the most commonly performed surgical procedures for herniated discs:
Discectomy
Discectomy is a surgical procedure where a portion of the injured disc is removed. The procedure is performed for a number of indications, including herniated disc. There are different surgical approaches that include:
- Microdiscectomy: Through a small incision, the injured portion of the disc is removed with the aid of a microscope.
- Endoscopic discectomy: The disc is removed through a thin, flexible tube with a camera.
Open discectomy: This traditional approach utilizes a larger incision such that the surgeon can clearly visualize the herniated disc.
Laminotomy
The vertebrae are the boney building blocks that stack one upon another to make up the cervical, thoracic and lumbar spine. The vertebrae are composed of the body and the posterior arch. The posterior arch is composed of the pedicles and the laminae.
The laminae are thin flat bones that arise from pedicles and create a bony central canal. This central canal contains and protects the spinal cord and spinal nerves.
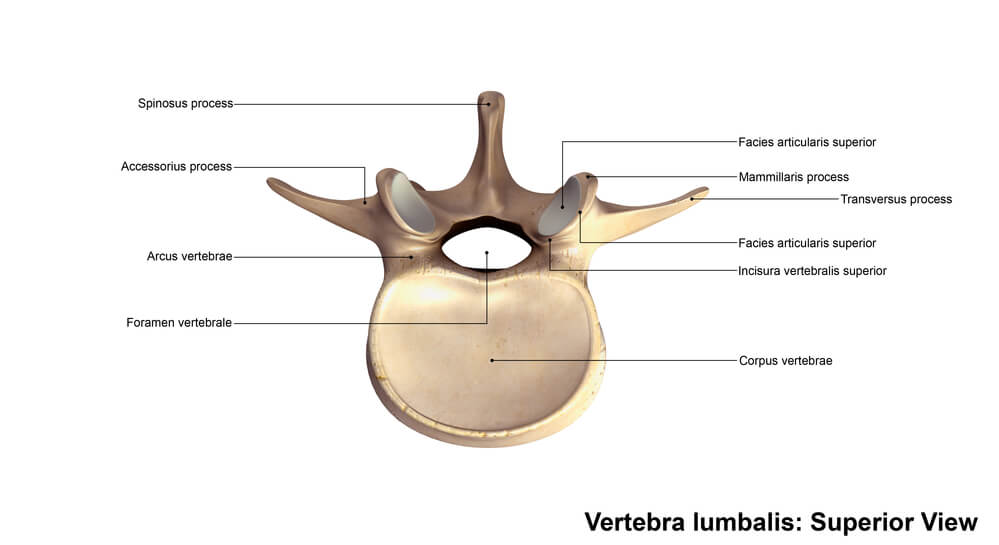
Conceptually, the laminae can be thought of as the bony roof that protects the spinal cord and nerves. A laminectomy is a surgical procedure where the lamina is removed.
A hemilaminectomy is a surgical procedure where only one of the lamina is removed. Recall that there is a right and left lamina at each level of the spine. A laminectomy involves removal of both the right and left lamina.
Spinal Fusion
A spinal fusion is a major surgery that involves the removal of one or more discs, which are then replaced with either bone graft and or spacers. The spine is then stabilized with screws, plates and rods. The hardware can be inserted posteriorly or anteriorly through the abdomen. There are many indications for spinal fusion, which include disc herniation.

Artificial Disc Surgery
Artificial disc surgery (ADR), also known as total disc replacement (TDR) is a major surgery where one or more of the discs is removed. Rather than insert bone grafts and spacers, as is the case in spinal fusion, an artificial disc is inserted between the vertebral bodies.
The primary objective of this procedure is to retain the natural motion and flexibility in the spine, thereby minimizing the occurrence of adjacent segment degeneration. By doing so, it aims to enhance the overall functionality and longevity of the spine.8
Recovering from Surgery
Recovery from surgery for herniated disc varies significantly depending upon the location and size of the disc herniation, past medical history, level of activity and the surgery performed.
In general, a discectomy and laminectomy require shorter hospitalizations, recovery and rehabilitation than fusion or artificial disc replacement.
Dedicated rehabilitation is critical for best clinical outcomes.
Complications After Surgery
All spinal surgeries have significant complications that include bleeding, infection, failure, escalation in pain, nerve damage, spinal cord injury, dural puncture and death.
Spinal fusion has unique set of complications that have been discussed in this previous blog:(https://centenoschultz.com/long-term-side-effects-of-spinal-fusion/).
The major complications associated with spinal fusion surgery are:
- Failed fusion: Also known as non-union, this is a clinical condition where the two bones fail to fuse.
- Hardware breaking: The implanted screws, rods and plates can break.
- Hardware loosening: The screws can back out.
- Adjacent segment disease (ASD): Fusion surgery involves removing vital shock absorbers known as discs. Unfortunately, this removal subsequently increases stress and strain on the discs and facet joints surrounding the fusion site. As a result, it can lead to degeneration and arthritis, posing a significant concern. The incidence rate of this issue stands at 9%,9 underscoring its significance.
Non-surgical Alternatives for Herniated Disc
In many cases, disc herniation responds to conservative, non-surgical treatment.
The three possible mechanisms of disc herniation reabsorption include:10
- Retraction of the protrusion
- Gradual dehydration and contraction of nucleus pulposus, which in turn causes the protrusions to retract into the annulus fibrosus
- Fragments of the herniated disc enter the epidural space, triggering an autoimmune response
When appropriate, surgery is best avoided as it forever changes the biomechanics of the spine. Discectomy removes the supportive outer side wall, whereas a laminectomy removes bone, tendon and important ligament that provides stability for the spine.
Fusion removes the disc, which is an important shock absorber and redirects the forces of daily living onto the discs, facet joints and ligaments above and below the fusion, leading to breakdown and injury.
At the Centeno-Schultz Clinic, treatment options for herniated discs include both PRP (platelet-rich plasma) and bone marrow concentrate. Both can be effective as they increase the blood flow and reduce inflammation around the injured disc. This in turn can accelerate healing and recovery.
PRP epidural injections have been demonstrated to be superior to steroids injections in terms of pain and improved function in patients with lumbar sciatica symptoms.11
To learn more please check out the video below:
Surgery May Not Always Be the Answer for a Herniated Disc
A disc herniation is a medical condition in which the thick outer fibers of the disc are injured, allowing the gelatinous center to push outward creating pain, restriction in range of motion and dysfunction. The two most common causes are degeneration and trauma. Other factors that can be associated with disc herniation include repetitive strain, genetics, obesity, and smoking.
There are different types of disc herniations that are based upon their location in the spine. They include cervical, thoracic, and lumbar disc herniations, central disc, lateral disc, and posterolateral disc herniations.
The specific type of surgery of herniated disc will depend upon many different factors. The most common types of surgeries for herniated disc include discectomy, laminectomy, fusion, and artificial disc replacement.The specific type of surgery of herniated disc will depend upon many different factors. The most common types of surgeries for herniated disc include discectomy, laminectomy, fusion, and artificial disc replacement.
Spinal surgery is a major surgery associated with significant risks that include bleeding, infection, failure, escalation in pain, nerve damage, spinal cord injury, dural puncture, and death. Spinal fusion has additional risks that include failure to fuse, hardware breaking, hardware loosening, adjacent segment disease and spinal muscle atrophy.
Disc herniation often responds to conservative, non-surgical treatment. When appropriate, surgery is best avoided as it forever changes the biomechanics of the spine. PRP and bone marrow concentrate are regenerative treatment options that can increase blood flow and reduce inflammation thereby accelerating healing and recovery.
If you or a loved one continues to suffer the pain and restriction in motion from a herniated disc, consider an in-office or telemedicine consultation at the Centeno-Schutlz Clinic. A board certified, fellowship trained physician will review your history, current symptoms, and imaging to determine whether you are a good candidate for regenerative treatments.
There’s always a non-surgical solution for your chronic pain.
There’s always a non-surgical solution for your chronic pain. Make an appointment with us today!

Christopher J. Centeno, MD
Christopher J. Centeno, M.D. is an international expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate in orthopedics. He is board-certified in physical medicine and rehabilitation with a subspecialty of pain medicine through The American Board of Physical Medicine and Rehabilitation. Dr. Centeno is one of the few physicians in the world with extensive experience in the culture expansion of and clinical use of adult bone marrow concentrate to treat orthopedic injuries. His clinic incorporates a variety of revolutionary pain management techniques to bring its broad patient base relief and results. Dr. Centeno treats patients from all over the US who…
Read more
John Schultz, MD
John R. Schultz M.D. is a national expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate for orthopedic injuries. He is board certified in Anesthesiology and Pain Medicine and underwent fellowship training in both. Dr. Schultz has extensive experience with same day as well as culture expanded bone marrow concentrate and sees patients at the CSC Broomfield, Colorado Clinic, as well the Regenexx Clinic in Grand Cayman. Dr. Schultz emphasis is on the evaluation and treatment of thoracic and cervical disc, facet, nerve, and ligament injuries including the non-surgical treatment of Craniocervical instability (CCI). Dr. Schultz trained at George Washington School of…
Read more
John Pitts, M.D.
Dr. Pitts is originally from Chicago, IL but is a medical graduate of Vanderbilt School of Medicine in Nashville, TN. After Vanderbilt, he completed a residency in Physical Medicine and Rehabilitation (PM&R) at Emory University in Atlanta, GA. The focus of PM&R is the restoration of function and quality of life. In residency, he gained much experience in musculoskeletal medicine, rehabilitation, spine, and sports medicine along with some regenerative medicine. He also gained significant experience in fluoroscopically guided spinal procedures and peripheral injections. However, Dr. Pitts wanted to broaden his skills and treatment options beyond the current typical standards of care.
Read more
Jason Markle, D.O.
Post-residency, Dr. Markle was selected to the Interventional Orthopedic Fellowship program at the Centeno-Schultz Clinic. During his fellowship, he gained significant experience in the new field of Interventional Orthopedics and regenerative medicine, honing his skills in advanced injection techniques into the spine and joints treating patients with autologous, bone marrow concentrate and platelet solutions. Dr. Markle then accepted a full-time attending physician position at the Centeno-Schultz Clinic, where he both treats patients and trains Interventional Orthopedics fellows. Dr. Markle is an active member of the Interventional Orthopedic Foundation and serves as a course instructor, where he trains physicians from around the world.
Read more
Brandon T. Money, D.O., M.S.
Dr. Money is an Indiana native who now proudly calls Colorado home. He attended medical school at Kansas City University and then returned to Indiana to complete a Physical Medicine and Rehabilitation residency program at Indiana University, where he was trained on non-surgical methods to improve health and function as well as rehabilitative care following trauma, stroke, spinal cord injury, brain injury, etc. Dr. Money has been following the ideology behind Centeno-Schultz Clinic and Regenexx since he was in medical school, as he believed there had to be a better way to care for patients than the status quo. The human body has incredible healing capabilities…
Read moreReferences:
- Fjeld OR, Grøvle L, Helgeland J, Småstuen MC, Solberg TK, Zwart JA, Grotle M. Complications, reoperations, readmissions, and length of hospital stay in 34 639 surgical cases of lumbar disc herniation. Bone Joint J. 2019 Apr;101-B(4):470-477. doi: 10.1302/0301-620X.101B4.BJJ-2018-1184.R1. PMID: 30929479.
- Kalb S, Martirosyan NL, Kalani MY, Broc GG, Theodore N. Genetics of the degenerated intervertebral disc. World Neurosurg. 2012 Mar-Apr;77(3-4):491-501. doi: 10.1016/j.wneu.2011.07.014. Epub 2011 Nov 7. PMID: 22120330.
- Adams MA. Mechanical properties of aging soft tissues. 2015. Intervertebral disc tissues; pp. 7–35. [Google Scholar]
- Mayer JE, Iatridis JC, Chan D, Qureshi SA, Gottesman O, Hecht AC. Genetic polymorphisms associated with intervertebral disc degeneration. Spine J. 2013 Mar;13(3):299-317. doi: 10.1016/j.spinee.2013.01.041. PMID: 23537453; PMCID: PMC3655694.
- Sheng B, Feng C, Zhang D, Spitler H, Shi L. Associations between Obesity and Spinal Diseases: A Medical Expenditure Panel Study Analysis. Int J Environ Res Public Health. 2017 Feb 13;14(2):183. doi: 10.3390/ijerph14020183. PMID: 28208824; PMCID: PMC5334737.
- Rajesh N, Moudgil-Joshi J, Kaliaperumal C. Smoking and degenerative spinal disease: A systematic review. Brain Spine. 2022 Aug 7;2:100916. doi: 10.1016/j.bas.2022.100916. PMID: 36248118; PMCID: PMC9560562.
- Sarsılmaz A, Yencilek E, Özelçi Ü, Güzelbey T, Apaydın M. The incidence and most common levels of thoracic degenerative disc pathologies. Turk J Phys Med Rehabil. 2018 May 16;64(2):155-161. doi: 10.5606/tftrd.2018.1302. PMID: 31453506; PMCID: PMC6657757.
- Medical Advisory Secretariat. Artificial discs for lumbar and cervical degenerative disc disease -update: an evidence-based analysis. Ont Health Technol Assess Ser. 2006;6(10):1-98. Epub 2006 Apr 1. PMID: 23074480; PMCID: PMC3379529.
- Okuda S, Yamashita T, Matsumoto T, et al. Adjacent Segment Disease After Posterior Lumbar Interbody Fusion: A Case Series of 1000 Patients. Global Spine J. 2018;8(7):722-7.
- Yu P, Mao F, Chen J, Ma X, Dai Y, Liu G, Dai F, Liu J. Characteristics and mechanisms of resorption in lumbar disc herniation. Arthritis Res Ther. 2022 Aug 23;24(1):205. doi: 10.1186/s13075-022-02894-8. PMID: 35999644; PMCID: PMC9396855.
- Centeno C, Markle J, Dodson E, Stemper I, Hyzy M, Williams C, Freeman M. The use of lumbar epidural injection of platelet lysate for treatment of radicular pain. J Exp Orthop. 2017 Nov 25;4(1):38. doi: 10.1186/s40634-017-0113-5. PMID: 29177632; PMCID: PMC5701904.
Am I a Candidate?
To answer this question, fill out the candidate form below to request a new patient evaluation, and a patient advocate will reach out to you to determine your next steps. Your one-hour, in-office or telemedicine evaluation will be with one of the world’s experts in the field of Interventional Orthopedics.