Torn Discs
Causes, Symptoms, Treatments, & Other Resources
What is a torn disc? How do you fix or help it? Does it Heal? Is there a treatment? Let’s dig in.
What Is a Torn Disc?
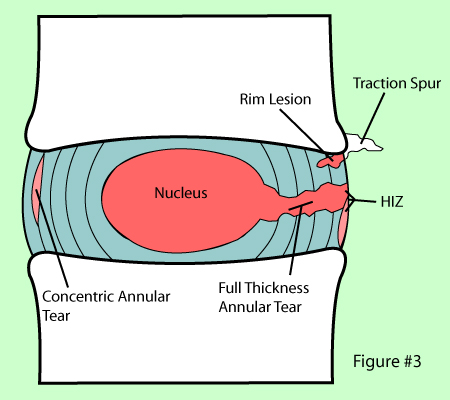
The spinal discs are shock absorbers that live at each level between the vertebral bones (1). They have a tough outer annulus part and a soft inner gel part (nucleus pulposis). The outer covering can get damaged which can sometimes be seen on MRI and other times requires additional testing to identify. These tears are called: a torn disc, a disc tear, an annular tear, and when seen on MRI a “High-Intensity Zone” or HIZ. They can cause pain, mostly through ingrown nerves (2).
What are the Symptoms?
There are torn disc findings that can be seen on MRI (HIZ) and these can be either asymptomatic (i.e. not painful) or can cause pain. Usually, the bigger and brighter they are on the MRI image, the more likely they are to cause pain (3). A reliable symptom of disc pain is an inability to sit. This is usually back pain with any sitting of more than 5-15 minutes (called sitting intolerance). While it’s possible to have a painful torn disc without sitting intolerance, this is one hallmark that many physicians look for. In addition, painful torn discs are also common in younger patients who are under 50 years of age.
Common Symptoms of a Torn Disc
Big Toe Numbness
Believe it or not, one of those significant issues that can present as numbness stems from the low back. In the lumbar spine, the nerve that exits the spine at the L5 level branches down through the hip, thigh, knee, lower leg, and, yes, all the way into the foot and toes. So a pinched or irritated nerve at that L5 level in the back can create problems, such as pain, numbness, tingling, and so on, anywhere along the nerve branch. So what can irritate the L5 spinal nerve? The list is long, but it includes disc issues, such as herniated…
Read More About Big Toe NumbnessButt Pain
Throwing this question out to the social-media masses is sure to bring out the cyber “comedians” among us, but the truth is when you really do have butt pain, it’s no laughing matter. So we’re glad you came here to ask because we actually do see many patients in our clinic with this problem. There are a number of issues that can cause butt pain, but the root causes we most often discover are hamstrings tendinopathy, a pinched low-back nerve, or sacroiliac joint syndrome. Let’s take a look at each of these individually. – Hamstrings Tendinopathy: The hamstrings are actually a collection of large muscles…
Read More About Butt PainCalf Muscle Twitching
A twitching calf muscle may seem like no big deal, and if it’s just a temporary annoyance that lasts a couple of days and then goes away, it may be. However, it can also be a warning sign of something bigger, especially if it continues. So, today, we’re going to explain a little about the calf and why it’s not a good idea to ignore calf muscle twitching. If there’s one muscle you’re likely familiar with, it’s the calf muscle. If you reach around and grab your calf and flex it, the muscle you are actually feeling just under the surface is called the gastrocnemius muscle.
Read More About Calf Muscle TwitchingCervicalgia / Neck Pain
Cervicalgia is also known as neck pain, which is an all-too-common, unpleasant pain. Read here to learn the symptoms, diagnosis, and treatment options. We will discuss other causes for cervicalgia. What symptoms are associated with cervicalgia? How is cervicalgia diagnosed? What are the treatment options for cervicalgia? Cervicalgia is a medical term used to describe neck pain. It is very common and affects approximately 2/3 of the population at some point in their life. Cervicalgia is the 4th major cause of disability. Risk factors include injury, prior history of neck and musculoskeletal pain, jobs that require a lot of desk work, low social support, job insecurity, physical weakness, and poor computer station setup.
Read More About Cervicalgia / Neck PainHip Pain that Radiates Down the Leg
Hip pain is miserable making walking across the room almost impossible at times. Hip labral tears are the most common cause, but there are more to consider. What is a hip labrum? Are there other causes of hip pain down the leg besides a hip labral tear? Does the presence of hip labral tear with pain down leg mean I need surgery? What are the treatment options for hip labrum tears? Given that labrum tears are present in patients without hip pain it is important to understand the other causes of anterior thigh and hip pain. SI Joint, muscles, irritation of low back nerves…
Read More About Hip Pain that Radiates Down the LegLeg Gives Out
Have you ever been walking and your leg gives out? It can be both surprising and alarming What would cause your leg to give out? Can sciatica cause your leg to give out? How do you treat weak legs? Let’s dig in.Weakness in the leg can arise from three principal sources: nerve problems, muscle weakness, and SI joint dysfunction. Weakness in the legs may indicate a significant nerve problem. In many cases, it may be the first indication of a nerve problem. There are three common causes of nerve injury: low back disorders, nerve compression as it descends down into the hip, thigh, and shin and medical conditions such as diabetes…
Read More About Leg Gives OutLower Back Pain When Sitting
After a long day on your feet sitting down is supposed to be way to relaxing. Unfortunately for some sitting for any length of time can be painful. Most people experience low back pain at some point in their life. The lifetime prevalence of low back pain is 85% (1). Let’s take a deeper look at the different types of pain and causes of low back pain when sitting. Pain can present in many different ways. It can be intermitent or constant. The quality of the low back pain can also vary depending upon the actual source of injury. Common examples include: Sharp and Stabbing, Dull and Aching, Throbbing/ Pulsating, Pins and Needles, Burning, Electrical
Read More About Lower Back Pain When SittingLower Back Pain When Standing
When you’re seated, the facet joints in your lower back are in an open and slightly flexed position. When you stand up, these joints compress. If they are painful or have arthritis, you’ll have pain as you stand up because this puts pressure on the painful joints. In addition, if there is any type of movement of one vertebra forward on another (called spondylolisthesis), then this shift will have occurred as you sit. This is called degenerative spondylolisthesis. When you get back up, the vertebrae will come back into position after a few seconds, leading to that awkward “walk it out period” that starts out painful and ends up more normal.
Read More About Lower Back Pain When StandingCauses of Torn Disc
Usually, it is one of these 3 scenarios:
- Injury to the disc
- Degeneration due to an orthopedic condition
- Combination of injury and degeneration (*most often the case)
How Is a Torn Disc Diagnosed?
There are two ways. The first and most common is MRI. The disc tear is seen as a bright spot in the darker disc annulus, called an HIZ or annular tear. Another major way these tears get diagnosed is by using discography (4). This is where the doctor places a needle into the disc by using x-ray guidance and injects contrast dye (that can be seen under x-ray) to pressurize the disc. The doctor is looking both to see if the patient’s typical back pain can be recreated (concordant) and whether the disc leaks (annular tear or torn disc).
Is a Torn Disc the Same as a Herniated Disc?
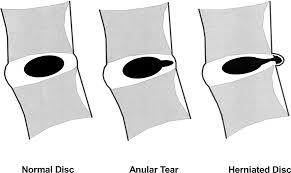
Not really. A herniated disc is when that soft inner gel squirts out a tear in the tough outer covering. A torn disc means that the outer covering is damaged (annulus) but the inner gel is still contained. In addition, a torn disc can be painful by itself, whereas a herniated disc is mostly painful because the gel that squirts out can irritate local spinal nerves.
How Long Does a Torn Disc Take to Heal?
A torn disc can take a few weeks to months to heal, but whether it heals at all depends on where it’s located. The outer part of the disc has a good blood supply, so tears here tend to heal (5). The inner parts of the disc annulus have a poor blood supply, so tears here tend not to heal well.
What Is the Treatment for a Torn Disc?
Many patients with a torn disc try physical therapy and if that fails they often try epidural steroid injections. However, none of this promotes healing, as the high dose steroids used can inhibit healing and cause disc degeneration. (6) If that doesn’t work, many surgeons will attempt to offer a low back fusion, which is where the disc is removed and hardware and/or bone is placed to make sure the level doesn’t move. However, large studies have shown this procedure to be ineffective and it can cause the levels above and below to begin to break down, leading to new problems (7,8). See my video below:
Another option is replacing the disc with a device (disc arthroplasty). However, the same ASD shown with fusion above is also a problem with this disc replacement surgery (9).
Perc-Orthobiologic Annuloplasty (POA) – A New Approach
What if it was possible to heal a torn disc? The patient’s own concentrated platelets, injected via x-ray guidance into the painful and torn disc have been shown to reduce pain (10). Similar research published by our group and others has also shown that the patient’s own bone marrow concentrate or stem cells can do the same (11-13). This procedure is called Percutaneous Orthobiologic Annuloplasty (POA).
How would this work? The goal of these injections is to heal the tear. If you take a look at the video below, you’ll see a disc tear before POA which is the bright spot in the dark disc annulus and then that same area on MRI after POA, which now shows no bright spot. This patient also reported significantly increased ability to sit for more than just 5-10 minutes and went back to working out.
Who is a candidate for POA? Patients with painful discs who have significant sitting intolerance. Generally, an MRI or discogram is performed. We also tend to use “Biologic Discography” which means that instead of injecting a bunch of contrast dye which has been shown to harm disc cells (14), we inject your own concentrated blood platelets to pressurize the disc. That way we’re combining a treatment that may heal the tears with a test.
The upshot? A torn disc can be a big concern but realize that steroid injections and surgery are no longer your only options. There are newer treatments for back pain that aim to heal the disc tear.
Doctors Who Help with Torn Disc

Christopher J. Centeno, MD
Christopher J. Centeno, M.D. is an international expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate in orthopedics.
Dr. Centeno is one of the few physicians in the world with extensive experience in the culture expansion of and clinical use of adult bone marrow concentrate to treat orthopedic injuries. His clinic incorporates a variety of revolutionary pain management techniques to bring its broad patient base relief and results. Dr. Centeno treats patients from all over the US who travel to Colorado to undergo innovative, non-surgical treatments. Dr. Centeno has chaired multiple international research-based conferences. He also maintains an active research-based practice, with multiple publications listed in the US National Library of Medicine. Dr. Centeno has also served as editor-in-chief of a medical research journal dedicated to traumatic injury.
Dr. Centeno trained at the Baylor College of Medicine, Texas Medical Center, and the Institute for Rehabilitation Research. He hails from both Florida and New York and currently resides in Boulder, Colorado with his wife and three children.

John Schultz, MD
John R. Schultz M.D. is a national expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate for orthopedic injuries. He is board certified in Anesthesiology and Pain Medicine and underwent fellowship training in both. Dr. Schultz has extensive experience with same day as well as culture expanded bone marrow concentrate and sees patients at the CSC Broomfield, Colorado Clinic, as well the Regenexx Clinic in Grand Cayman. Dr. Schultz emphasis is on the evaluation and treatment of thoracic and cervical disc, facet, nerve, and ligament injuries including the non-surgical treatment of Craniocervical instability (CCI). Dr. Schultz trained at George Washington School of…
Read more
John Pitts, M.D.
Dr. Pitts is originally from Chicago, IL but is a medical graduate of Vanderbilt School of Medicine in Nashville, TN. After Vanderbilt, he completed a residency in Physical Medicine and Rehabilitation (PM&R) at Emory University in Atlanta, GA. The focus of PM&R is the restoration of function and quality of life. In residency, he gained much experience in musculoskeletal medicine, rehabilitation, spine, and sports medicine along with some regenerative medicine. He also gained significant experience in fluoroscopically guided spinal procedures and peripheral injections. However, Dr. Pitts wanted to broaden his skills and treatment options beyond the current typical standards of care.
Read more
Jason Markle, D.O.
Post-residency, Dr. Markle was selected to the Interventional Orthopedic Fellowship program at the Centeno-Schultz Clinic. During his fellowship, he gained significant experience in the new field of Interventional Orthopedics and regenerative medicine, honing his skills in advanced injection techniques into the spine and joints treating patients with autologous, bone marrow concentrate and platelet solutions. Dr. Markle then accepted a full-time attending physician position at the Centeno-Schultz Clinic, where he both treats patients and trains Interventional Orthopedics fellows. Dr. Markle is an active member of the Interventional Orthopedic Foundation and serves as a course instructor, where he trains physicians from around the world.
Read more
Brandon T. Money, D.O., M.S.
Dr. Money is an Indiana native who now proudly calls Colorado home. He attended medical school at Kansas City University and then returned to Indiana to complete a Physical Medicine and Rehabilitation residency program at Indiana University, where he was trained on non-surgical methods to improve health and function as well as rehabilitative care following trauma, stroke, spinal cord injury, brain injury, etc. Dr. Money has been following the ideology behind Centeno-Schultz Clinic and Regenexx since he was in medical school, as he believed there had to be a better way to care for patients than the status quo. The human body has incredible healing capabilities…
Read moreOther Resouces for Torn Disc
The Spine Owner’s Manual: How to Avoid Back Pain & Life-Altering Surgery
This e-book from Dr. Chris Centeno focuses on the spine and how it functions within the human musculoskeletal system and the body as a whole. Everything in our bodies works together like a well-tuned symphony to support our well-being, and a strong spine (including all of its component parts, such as spinal nerves, ligaments, muscles, etc.) is critical to complete health.
Using the Regenexx SANS approach, The Spine Owner’s Manual provides a series of tests and clearly defined exercises that you can do on your own to measure and monitor your own spinal health. These musculoskeletal tests will allow you to monitor where your own body might be struggling to maintain proper stability, articulation, symmetry, and neuromuscular function.
-
What Happens If You Have Back Pain From Golf?
Back pain is a common complaint among golfers, impacting both amateur enthusiasts and professional athletes. Golf, while seemingly low-impact, involves repetitive, high-intensity movements that can stress the spine and surrounding structures. Understanding the causes, symptoms, and preventative measures for golf-related back pain can help maintain performance and long-term health. Golf And Back Pain The golf…
-
Spinal Fusion Recovery: What to Expect
Navigating spinal fusion recovery can be a daunting prospect, given its impact on daily life and mobility. Understanding what to expect during this process is crucial for individuals undergoing this procedure. In this article, we’ll explore the typical timeline, challenges, and strategies for managing recovery after spinal fusion surgery, providing insights to help individuals prepare…
-
Back Cracking: The Truth of What’s Actually Happening in Your Body
Back cracking is a phenomenon that many people experience, often eliciting both curiosity and concern. Whether it’s the satisfying pop from a morning stretch or the deliberate twist during a yoga session, the sound and sensation of cracking your back can be oddly gratifying. But what exactly is happening inside your body when you hear…
-
Back Fusion
Spinal fusion, also known as back fusion, is a surgical procedure designed to help severe spinal instability that causes severe pain or nerve injuries. It involves permanently connecting two or more vertebrae in your spine to eliminate motion between them. This article will delve into the intricacies of spinal fusion, exploring the reasons behind the…
-
Understanding the Normal Curvature of the Spine
The human spine, a marvel of engineering, is not a straight column but rather a structure with gentle curves. These natural curves are essential for maintaining balance, allowing flexibility, and absorbing the shock of movement. The spine’s curvature plays a critical role in overall health, influencing posture, mobility, and the function of the nervous system. …
-
Spinal Anterior Longitudinal Ligament Function
Have you had a neck injury or whiplash trauma? Do you have neck pain, especially when looking up, and you don’t know the cause? Then you may want to learn about the cervical anterior longitudinal ligament (ALL). Anatomy of the Anterior Longitudinal Ligament The ALL is a strong, wide ligament that runs along the front…
References:
(1) Nixon J. Intervertebral disc mechanics: a review. J R Soc Med. 1986;79(2):100–104. doi: 10.1177/014107688607900211.
(2) Ito K, Creemers L. Mechanisms of intervertebral disk degeneration/injury and pain: a review. Global Spine J. 2013;3(3):145–152. doi: 10.1055/s-0033-1347300.
(3) Teraguchi M, Yim R, Cheung JP, Samartzis D. The association of high-intensity zones on MRI and low back pain: a systematic review. Scoliosis Spinal Disord. 2018;13:22. Published 2018 Oct 20. doi:10.1186/s13013-018-0168-9
(4) Ito K, Creemers L. Mechanisms of intervertebral disk degeneration/injury and pain: a review. Global Spine J. 2013;3(3):145–152. doi: 10.1055/s-0033-1347300
(5) Grunhagen T, Wilde G, Soukane DM, Shirazi-Adl SA, Urban JP. Nutrient supply and intervertebral disc metabolism. J Bone Joint Surg Am. 2006 Apr;88 Suppl 2:30-5. https://www.ncbi.nlm.nih.gov/pubmed/16595440
(6) Aoki M, Kato F, Mimatsu K, Iwata H. Histologic changes in the intervertebral disc after intradiscal injections of methylprednisolone acetate in rabbits. Spine (Phila Pa 1976). 1997 Jan 15;22(2):127-31. https://www.ncbi.nlm.nih.gov/pubmed/9122791
(7) Bydon M, De la Garza-Ramos R, Macki M, Baker A, Gokaslan AK, Bydon A. Lumbar fusion versus nonoperative management for treatment of discogenic low back pain: a systematic review and meta-analysis of randomized controlled trials. J Spinal Disord Tech. 2014 Jul;27(5):297-304. doi: 10.1097/BSD.0000000000000072.
(8) Okuda S, Yamashita T, Matsumoto T, et al. Adjacent Segment Disease After Posterior Lumbar Interbody Fusion: A Case Series of 1000 Patients. Global Spine J. 2018;8(7):722–727. doi:10.1177/2192568218766488 torn disc
(9) Zigler JE, Blumenthal SL, Guyer RD, Ohnmeiss DD, Patel L. Progression of Adjacent-level Degeneration After Lumbar Total Disc Replacement: Results of a Post-hoc Analysis of Patients With Available Radiographs From a Prospective Study With 5-year Follow-up. Spine (Phila Pa 1976). 2018;43(20):1395–1400. doi: 10.1097/BRS.0000000000002647
(10) Tuakli-Wosornu YA, Terry A, Boachie-Adjei K, Harrison JR, Gribbin CK, LaSalle EE, Nguyen JT, Solomon JL, Lutz GE. Lumbar Intradiskal Platelet-Rich Plasma (PRP) Injections: A Prospective, Double-Blind, Randomized Controlled Study. PM R. 2016 Jan;8(1):1-10; quiz 10. doi: 10.1016/j.pmrj.2015.08.010.
(11) Pettine KA, Suzuki RK, Sand TT, Murphy MB. Autologous bone marrow concentrate intradiscal injection for the treatment of degenerative disc disease with three-year follow-up. Int Orthop. 2017 Oct;41(10):2097-2103. doi: 10.1007/s00264-017-3560-9.
(12) Elabd C, Centeno CJ, Schultz JR, Lutz G, Ichim T, Silva FJ. Intra-discal injection of autologous, hypoxic cultured bone marrow-derived mesenchymal stem cells in five patients with chronic lower back pain: a long-term safety and feasibility study. J Transl Med. 2016;14(1):253. Published 2016 Sep 1. doi: 10.1186/s12967-016-1015-5
(13) Centeno C, Markle J, Dodson E, et al. Treatment of lumbar degenerative disc disease-associated radicular pain with culture-expanded autologous mesenchymal stem cells: a pilot study on safety and efficacy. J Transl Med. 2017;15(1):197. Published 2017 Sep 22. doi: 10.1186/s12967-017-1300-y
(14) Chee AV, Ren J, Lenart BA, Chen EY, Zhang Y, An HS. Cytotoxicity of local anesthetics and nonionic contrast agents on bovine intervertebral disc cells cultured in a three-dimensional culture system. Spine J. 2014;14(3):491–498. doi: 10.1016/j.spinee.2013.06.095