Calcific Tendonitis
If you have ever experienced persistent shoulder pain, you know how detrimental it can be to your daily life. It can disrupt your ability to perform simple tasks such as reaching for a glass in a high cupboard or even just brushing your hair. One potential cause of such discomfort that isn’t as widely known as it should be, is a condition known as calcific tendonitis.
Today we are going to be focusing on a condition that deserves more spotlight than it usually gets – calcific tendonitis. This common yet often misunderstood condition can serve as a silent troublemaker, lying beneath the surface of unexplained shoulder pain.
Calcific tendonitis refers to a condition where calcium deposits form in the tendons of your body. While it can affect different parts of the body, it’s most commonly found within the rotator cuff tendons in the shoulder. These calcium deposits can cause inflammation and pain, often severe, leading to a considerable impact on the quality of life of those affected.
Despite its prevalence, many of us are not familiar with the condition. It’s a significant cause of shoulder pain, yet it often goes undiagnosed or misdiagnosed, resulting in ongoing discomfort and an unresolved root cause. The lack of awareness and understanding of calcific tendonitis among the general population only exacerbates this problem.
Today, we’ll dive into the details of calcific tendonitis. We will explore its causes, symptoms, the science behind how and why these calcium deposits form, diagnosis, treatment options, and some tips for managing this condition.
What is Calcific Tendonitis?
Calcific tendonitis, also known as calcifying tendonitis, is a condition characterized by the formation of calcium deposits in a tendon, most commonly in the rotator cuff tendons of the shoulder. These deposits are not due to injury or trauma but rather occur spontaneously.
Tendons, the thick connective tissues that link muscles to bones, aren’t usually calcified. However, in calcific tendonitis, calcium builds up in these tissues, which can result in inflammation and severe pain. This condition tends to occur more commonly in adults between 30 and 60 years old, and it’s more prevalent in women than in men.
While the exact cause of calcific tendonitis is unknown, it’s thought to occur in two phases: the pre-calcification stage, where the body undergoes cellular changes, and the calcific stage, where calcium is deposited, then resorbed, causing significant pain.
Where Can Calcific Tendonitis Occur?
Calcific tendinitis most commonly affects the tendons of the shoulder, specifically the rotator cuff tendons. The rotator cuff is a group of muscles and tendons that surround the shoulder joint, keeping the head of your upper arm bone within the shallow socket of the shoulder.
The most frequently affected tendon within the rotator cuff is the supraspinatus tendon, although the infraspinatus and the subscapularis tendons can also be affected. While the shoulder is the most common site, calcific tendinitis can occur in other tendons throughout the body.
Some of these areas include:
- Elbow: Particularly in the tendons surrounding the elbow joint, such as the biceps tendon.
- Wrist: The tendons in the wrist that extend or flex the wrist can sometimes develop calcification.
- Hip: The gluteus medius tendon, which is important for hip stability and movement, can occasionally be affected.
- Knee: Although less common, calcific tendinitis can sometimes occur in the tendons around the knee, such as the quadriceps tendon.
- Achilles Tendon: Calcific tendinitis may occur in the Achilles tendon, the tendon that connects the heel to the calf muscles.
It’s important to note that while these other sites can be affected by calcific tendinitis, it is much less common than in the shoulder.
Stages Of Calcific Tendonitis
The progression of calcific tendonitis generally occurs in three stages: the pre-calcification stage, the calcific stage, and the post-calcific stage.
Each stage has its own characteristics and symptoms.
Pre-calcification Stage
This is the initial stage of the condition where the body’s natural changes prepare the tendons for the deposition of calcium. The actual calcification hasn’t started yet, and no symptoms are usually apparent during this phase.
Cellular changes occur within the tendon that lead to the development of abnormal tendon cells (tenocytes), which are capable of forming calcium deposits.
Calcific Stage
This stage is characterized by the actual formation and deposition of calcium in the tendons and is further divided into two phases: the formative phase and the resorptive phase.
- Formative Phase: During this phase, the calcium is deposited within the tendon, resulting in the formation of calcium deposits. The deposits start as a chalky substance and later harden. This phase is usually asymptomatic, meaning that patients typically don’t experience pain or discomfort.
- Resorptive Phase: In this phase, the body begins to reabsorb the calcium deposit. This process results in increased blood flow and pressure within the tendon, leading to significant inflammation and pain.
The pain can be intense and is typically what drives individuals to seek medical attention. It’s during this phase that the calcific deposits appear the largest on imaging studies.
Post-calcification Stage
This is the final stage where the calcium deposit is completely resorbed and the tendon begins to heal and return to its normal state. The tendon tissue undergoes remodeling, essentially returning to its pre-calcification health. The pain generally reduces and ultimately disappears in this stage.
It’s important to note that these stages can vary in length from person to person and may not always follow a predictable course. Some people may not even be aware of the condition until they reach the painful resorptive phase of the calcific stage.
Others may have calcific deposits that are discovered incidentally on imaging studies for other issues but never experience significant pain or symptoms.
Causes Of Calcific Tendonitis
The exact cause of calcific tendonitis remains unknown, but it appears to be a result of the body’s natural, self-healing process gone awry.
There are, however, several theories and associated factors that may contribute to the development of this condition.
Cellular Transformation
One leading theory is that the tenocytes, the cells that compose tendons, undergo a transformation into cells that resemble bone cells (chondrocytes and osteocytes). This transformation is thought to be a response to injury or stress, leading these transformed cells to produce calcium deposits within the tendon.
Aging and Wear-and-Tear
Age-related changes and degenerative processes may play a role in the development of calcific tendonitis. The condition is most common in middle-aged and older adults, suggesting that wear-and-tear over time may contribute.
Genetic Factors
Some studies suggest that there may be a genetic predisposition to developing calcific tendonitis, although more research is needed in this area.
Metabolic Conditions
Certain metabolic conditions, such as diabetes, thyroid disorders, and abnormalities in calcium metabolism, may increase the risk of developing calcific tendonitis.
Vascular and Hypoxic Theories
Other theories suggest that poor blood supply to the tendons or hypoxia (a condition in which part of the body or a region of the body is deprived of adequate oxygen supply) can lead to tissue changes and ultimately calcification.
Overuse or Strain
While it is less clear, repetitive strain or overuse of the tendon could potentially trigger the process leading to calcific tendonitis.
Gender and Lifestyle
Calcific tendonitis is more common in women than in men, and a sedentary lifestyle may also increase risk.
Despite these theories and associations, it’s important to note that calcific tendonitis can also occur in individuals without any of these risk factors. Further research is needed to more fully understand the exact causes and risk factors for this condition.
Symptoms Of Calcific Tendonitis
The symptoms of calcific tendonitis can vary depending on the stage of the condition, and some people may not have any symptoms until the condition progresses significantly.
When symptoms do occur, they often include:
Pain
This is the most common symptom of calcific tendonitis. The pain can be mild to severe, often described as sharp or throbbing. It’s typically located in the shoulder but can radiate down the arm or up to the neck. The pain might be worse at night or with certain movements.
Limited Range of Motion
As the condition progresses, the affected shoulder might become stiff, leading to a reduced range of motion. Activities like lifting, reaching, or even simple movements like dressing or combing hair can become difficult.
Tenderness
The area around the affected tendon may be tender to touch.
Inflammation and Swelling
The shoulder may become swollen, and inflammation can sometimes be felt as warmth over the affected area.
Increased Pain with Activity
The pain often increases with activity or movement of the affected joint, especially movements that put stress on the involved tendon.
Calcific Crisis
In some cases, individuals may experience a sudden onset of severe pain, known as a calcific crisis. This is due to the acute inflammation caused when the body begins to reabsorb the calcium deposits.
These symptoms can significantly affect a person’s quality of life, interfering with daily activities and sleep. If you’re experiencing these symptoms, especially persistent shoulder pain that doesn’t improve with rest and over-the-counter pain medication, it’s important to seek medical advice for a proper diagnosis and treatment plan.
Who Is At Risk Of Developing Calcific Tendonitis?
While the exact cause of calcific tendonitis is unknown, several risk factors have been associated with an increased likelihood of developing the condition. It’s important to note that having one or more of these risk factors does not guarantee that you will develop calcific tendonitis, but it does increase your risk. These risk factors include:
Age
Calcific tendonitis most commonly affects people between the ages of 30 and 60. It’s thought that the natural aging process and the associated wear-and-tear on the body may contribute to the development of the condition.
Sex
Women are more likely than men to develop calcific tendonitis. The reasons for this are not fully understood, but it may relate to hormonal differences and other biological factors.
Metabolic Conditions
Certain metabolic disorders, such as diabetes, thyroid disorders, and abnormalities in calcium metabolism, are thought to increase the risk of developing calcific tendonitis.
Certain Occupations or Activities
Jobs or activities that involve repetitive shoulder movements or overuse of the shoulder can increase the risk. This includes sports like tennis or baseball, or occupations such as painting or construction work.
Genetic Factors
There may be a genetic component to developing calcific tendonitis. If family members have had the condition, your risk might be higher.
Sedentary Lifestyle
Lack of physical activity can lead to weaker muscles and reduced mobility in the shoulder, which may contribute to the development of calcific tendonitis.
While these risk factors can increase the likelihood of developing calcific tendonitis, the condition can also occur in individuals without any apparent risk factors. It’s also worth noting that having these risk factors does not guarantee that you’ll develop the condition; they simply increase the likelihood.
Calcific Tendonitis Diagnosis
The diagnosis of calcific tendonitis is typically made through a combination of clinical evaluation and imaging studies.
Here’s how the process usually goes:
- Medical History: The healthcare provider will start by asking about your symptoms, their duration and intensity, any previous shoulder injuries or conditions, your occupational and recreational activities, and your general health status.
- Physical Examination: During the physical exam, the provider will assess the range of motion of your shoulder, check for areas of tenderness, and may perform specific maneuvers to determine which tendon could be involved.
- Imaging Studies: To confirm the diagnosis and rule out other conditions, imaging studies are usually required:
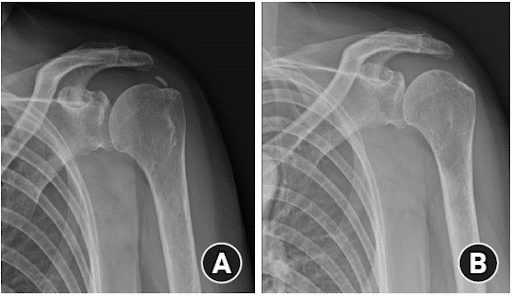
- X-rays: X-rays can show the presence of calcium deposits within the tendons, which is the hallmark of calcific tendonitis.
- Ultrasound: An ultrasound can provide a detailed view of the soft tissues and can help locate and measure the size of the calcific deposits. It’s also useful for guiding treatments like needling or injections.
- Magnetic Resonance Imaging (MRI): While an MRI isn’t typically necessary for diagnosing calcific tendonitis, it can be useful in cases where the diagnosis is uncertain or if other conditions are suspected.
An MRI provides detailed images of both bone and soft tissues, including the tendons and muscles.
The diagnosis of calcific tendonitis is usually straightforward once the calcium deposits are visualized on the imaging studies. However, it’s essential to differentiate it from other conditions that can cause similar symptoms, like rotator cuff tears, arthritis, bursitis, and other types of tendonitis.
Common Treatments For Calcific Tendonitis
Treatment of calcific tendonitis typically depends on the severity of symptoms and the size and location of the calcific deposits. The goal of treatment is to relieve pain, reduce inflammation, and improve shoulder function. Treatment options can be categorized as conservative (non-surgical) and surgical.
Rest and Activity Modification
Avoiding activities that cause shoulder pain can help reduce inflammation and prevent further injury.
Physical Therapy
Specific exercises can improve the range of motion and strengthen the muscles that support the shoulder. This can help to reduce pain and improve function.
Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)
Over-the-counter medications like ibuprofen and naproxen can help to reduce pain and inflammation.
Corticosteroid Injections
If symptoms are severe or do not improve with other treatments, your doctor may recommend a corticosteroid injection into the shoulder. This can provide rapid relief of inflammation and pain.
While the above is a simple and good start, most of these options fail because they are not addressing the issue of calcium deposits.
Direct and minimally invasive procedures have been shown to be the most effective:
- Extracorporeal Shock Wave Therapy (ESWT): This treatment uses sound waves to break up the calcium deposits, which can then be reabsorbed by the body. This is recommended by the NICE (National Institute of Health and Care Excellence) see more here.
- Ultrasound-guided Needling: This procedure uses a needle to break up the calcium deposits under ultrasound guidance. There are 2 ways to accomplish this
Needle barbotage – which consists of numbing the area and then using a large bore needle (18g) to manually break up the calcium and using the syringe plunger effect to aspirate the calcium – while this is very useful, it can take several treatments and each treatment can take a long time to accomplish its goal.
The best option is a newer device called TENEX. This is a device that utilizes vibration to break up the calcium and simultaneously flush and aspirate the calcium efficiently. The benefit is that it can quickly break up the calcium and aspirate within a few minutes.
Here, watch this video of Dr. Markle breaking up a small bone spur in an elbow that was pushing on a nerve:
Surgical Treatments
Surgery is usually considered only when conservative treatments have failed to relieve symptoms. The most common surgical procedure for calcific tendonitis is arthroscopic surgery.
During this procedure, the surgeon uses small instruments and a camera to remove the calcium deposits from the tendon. The procedure is minimally invasive and usually allows for a faster recovery compared to traditional open surgery.
Remember, the best treatment for calcific tendonitis varies depending on individual circumstances such as the patient’s overall health, the severity of the symptoms, and the patient’s personal preferences. Therefore, it’s crucial to have a discussion with a healthcare provider to determine the most appropriate treatment plan.
Regenerative Treatment Options
Once the calcium is removed from the tendon, there will be a defect or hole in the tendon. While these can then heal on their own, we can also add an ortho-biologic to the procedure to assist in accelerating the tendon recovery such as PRP, bone marrow concentrates, or prolotherapy:
Prolotherapy Injections
It has been successful in the treatment of many disorders including neck, shoulder, knee, and ankle pain. Dr. Centeno recently published an article in The Journal of Prolotherapy in which he discusses the use of x-ray guidance with prolotherapy. This ensures that the injection is in the correct place to maximize clinical results. Dr. Centeno discusses the use of prolotherapy for the treatment of neck, knee, sacroiliac joint, ankle, ischial tuberosity, and shoulder pain. At the Centeno-Schultz Clinic x-ray guided prolotherapy is just one of the therapies utilized in the successful treatment of pain. Regenerative injection therapy (RIT) or prolotherapy…
Read More About Prolotherapy InjectionsPRP Injections
PRP is short for platelet-rich plasma, and it is autologous blood with concentrations of platelets above baseline values. The potential benefit of platelet-rich plasma has received considerable interest due to the appeal of a simple, safe, and minimally invasive method of applying growth factors. PRP treatments are a form of regenerative medicine that utilizes the blood healing factors to help the body repair itself by means of injecting PRP into the damaged tissue. In regenerative orthopedics, it is typically used for the treatment of muscle strains, tears, ligament and tendon tears, minor arthritis, and joint instability. There have been more than 30 randomized controlled trials of PRP…
Read More About PRP InjectionsTenex Procedure
The Tenex Health TX® System is a minimally-invasive, percutaneous procedure using ultrasonic energy to treat pain-generating soft and hard tissue conditions. This treatment is clinically proven to remove tendon pain for over 85% of patients1,2,3,4,5. If conservative approaches such as physical therapy, cortisone injections, medication, and downtime do not provide relief, Tenex may be your next option.Using this technique, we help patients restore musculoskeletal function, may provide quick pain relief, and avoid invasive surgery and dangerous drugs. Tenex may also be effective if you have had a failed surgical procedure. Your doctor will use image-guidance to identify and target the…
Read More About Tenex ProcedureSurgery Is Not The Only Option
If you have been dealing with shoulder pain or pain in other areas caused by calcific tendonitis and not where you would like to be, before considering surgery, know there are multiple ways to address the calcium to relieve your pain!
Contact us today and we will set you up with one of our expert physicians who can evaluate and discuss best treatment options to get you back to full function without surgery!

Christopher J. Centeno, MD
Christopher J. Centeno, M.D. is an international expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate in orthopedics. He is board-certified in physical medicine and rehabilitation with a subspecialty of pain medicine through The American Board of Physical Medicine and Rehabilitation. Dr. Centeno is one of the few physicians in the world with extensive experience in the culture expansion of and clinical use of adult bone marrow concentrate to treat orthopedic injuries. His clinic incorporates a variety of revolutionary pain management techniques to bring its broad patient base relief and results. Dr. Centeno treats patients from all over the US who…
Read more
John Schultz, MD
John R. Schultz M.D. is a national expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate for orthopedic injuries. He is board certified in Anesthesiology and Pain Medicine and underwent fellowship training in both. Dr. Schultz has extensive experience with same day as well as culture expanded bone marrow concentrate and sees patients at the CSC Broomfield, Colorado Clinic, as well the Regenexx Clinic in Grand Cayman. Dr. Schultz emphasis is on the evaluation and treatment of thoracic and cervical disc, facet, nerve, and ligament injuries including the non-surgical treatment of Craniocervical instability (CCI). Dr. Schultz trained at George Washington School of…
Read more
John Pitts, M.D.
Dr. Pitts is originally from Chicago, IL but is a medical graduate of Vanderbilt School of Medicine in Nashville, TN. After Vanderbilt, he completed a residency in Physical Medicine and Rehabilitation (PM&R) at Emory University in Atlanta, GA. The focus of PM&R is the restoration of function and quality of life. In residency, he gained much experience in musculoskeletal medicine, rehabilitation, spine, and sports medicine along with some regenerative medicine. He also gained significant experience in fluoroscopically guided spinal procedures and peripheral injections. However, Dr. Pitts wanted to broaden his skills and treatment options beyond the current typical standards of care.
Read more
Jason Markle, D.O.
Post-residency, Dr. Markle was selected to the Interventional Orthopedic Fellowship program at the Centeno-Schultz Clinic. During his fellowship, he gained significant experience in the new field of Interventional Orthopedics and regenerative medicine, honing his skills in advanced injection techniques into the spine and joints treating patients with autologous, bone marrow concentrate and platelet solutions. Dr. Markle then accepted a full-time attending physician position at the Centeno-Schultz Clinic, where he both treats patients and trains Interventional Orthopedics fellows. Dr. Markle is an active member of the Interventional Orthopedic Foundation and serves as a course instructor, where he trains physicians from around the world.
Read more
Brandon T. Money, D.O., M.S.
Dr. Money is an Indiana native who now proudly calls Colorado home. He attended medical school at Kansas City University and then returned to Indiana to complete a Physical Medicine and Rehabilitation residency program at Indiana University, where he was trained on non-surgical methods to improve health and function as well as rehabilitative care following trauma, stroke, spinal cord injury, brain injury, etc. Dr. Money has been following the ideology behind Centeno-Schultz Clinic and Regenexx since he was in medical school, as he believed there had to be a better way to care for patients than the status quo. The human body has incredible healing capabilities…
Read moreMore Resources for Calcific Tendonitis
The Spine Owner’s Manual: How to Avoid Back Pain & Life-Altering Surgery
This e-book from Dr. Chris Centeno focuses on the spine and how it functions within the human musculoskeletal system and the body as a whole. Everything in our bodies works together like a well-tuned symphony to support our well-being, and a strong spine (including all of its component parts, such as spinal nerves, ligaments, muscles, etc.) is critical to complete health.
Using the Regenexx SANS approach, The Spine Owner’s Manual provides a series of tests and clearly defined exercises that you can do on your own to measure and monitor your own spinal health. These musculoskeletal tests will allow you to monitor where your own body might be struggling to maintain proper stability, articulation, symmetry, and neuromuscular function.
Relevant Articles
-
10 Best Shoulder Physical Therapy Exercises to Ease the Pain
Physical therapists often recommend specific exercises to alleviate shoulder pain, recognizing their effectiveness in both treating and preventing shoulder issues. These exercises, designed to enhance strength, flexibility, and mobility, can be a key component of a pain management strategy. Moreover, the ability to perform these exercises at home makes them a convenient option for patients…
-
Knee Pain Location Chart: What The Pain In Your Knee Means
The knee joint is the largest compound synovial joint of the human body. The joint has bones, cartilage, muscles, and bursae that are held together by ligaments and tendons. Damage to any of these structures can give rise to knee pain. The location of knee pain can be very telling, and can help narrow down…
-
Understanding Knee Pain Symptoms To Get The Best Treatments
Knee pain affects about 25% of the population (1). The knee joint involves three bones, namely the patella, the femur, and the tibia. Knee pain can be a sign of damage to the ligaments, bones, bursae, or muscle tendons because there are so many structures within the knee joint. In this post, we’ll discuss the…
-
KT Tape For Hamstring Tendonitis
Hamstring tendinosis is a condition that causes pain and inflammation in the hamstring tendons. The hamstring tendons are the tough bands of tissue that attach the hamstring muscles to the bones in the back of the thigh. Hamstring tendinosis is a degenerative condition, meaning that it is a condition that causes the tissue to break…
-
Treatment For A Torn Rotator Cuff Without Surgery: Exploring Your Options
Welcome to the Guide for Rotator Cuff Tear Relief Without Surgery. Rotator cuff injuries affect millions of people globally (1). The incidence vastly increases with age. Irrespective of the cause, there are many treatment options for rotator cuff injuries apart from surgery. If you want to avoid rotator cuff surgery, you’re in the right place!…
-
7 Untreated Whiplash Symptoms You Need to Watch For
Whiplash is a significant injury that is commonly associated with motor vehicle accidents. Dr. Schultz discusses what whiplash is, the structures that can be injured, the 7 untreated whiplash symptoms that you need to watch for, and the major long-term consequences of not treating whiplash symptoms.
Unsure about which treatment path to follow? Consult us and get a second opinion!
References:
- Chianca, V., Albano, D., Messina, C., Midiri, F., Mauri, G., Aliprandi, A., Catapano, M., Pescatori, L.C., Monaco, C.G., Gitto, S. and Mainini, A.P., 2018. Rotator cuff calcific tendinopathy: from diagnosis to treatment. Acta Bio Medica: Atenei Parmensis, 89(Suppl 1), p.186.
- Huisstede, B.M., Gebremariam, L., van der Sande, R., Hay, E.M. and Koes, B.W., 2011. Evidence for effectiveness of Extracorporal Shock-Wave Therapy (ESWT) to treat calcific and non-calcific rotator cuff tendinosis–a systematic review. Manual therapy, 16(5), pp.419-433.
- Pakos, E., Gkiatas, I., Rakkas, G., Papadopoulos, D., Gelalis, I., Vekris, M. and Korompilias, A., 2018. Calcific deposit needling in combination with extracorporeal shock wave therapy (ESWT): A proposed treatment for supraspinatus calcified tendinopathy. SICOT-J, 4.
- Schmitz, C., Császár, N.B., Milz, S., Schieker, M., Maffulli, N., Rompe, J.D. and Furia, J.P., 2015. Efficacy and safety of extracorporeal shock wave therapy for orthopedic conditions: a systematic review on studies listed in the PEDro database. British medical bulletin, 116(1), p.115.
- Lee JP, Kim DS, Han JY, Baik SH, Kwak JW, Kim SH. Clinical and radiological outcomes of ultrasound-guided barbotage using a spinal needle and subacromial steroid injection for calcific tendinitis of the shoulder. Clin Shoulder Elb. 2022 Jun;25(2):140-144. doi: 10.5397/cise.2021.00724. Epub 2022 May 31. PMID: 35698783; PMCID: PMC9185114.