Failed Back Syndrome
Chronic low back pain can have a severe effect on your life, get in the way of your daily activities, impact your work performance, and even lead to disability. It isn’t surprising that such a high number of patients choose to undergo back surgery – despite the risks, painful rehabilitation, and lengthy recovery times it comes with.
But what happens when back surgery, seemingly the answer to a pain-free life, fails to deliver the expected results? The consequences can be even more devastating. After all that you’ve been through, feeling like you are back to square one can be overwhelming. No wonder so many patients with failed back syndrome experience depression and declining quality of life.
Fortunately, there are alternatives to repeat surgery that can relieve your symptoms and tackle the root of your back pain without invasive procedures. Learn more below.
What Is Failed Back Surgery Syndrome?
Failed back surgery syndrome (FBSS), also called failed back, is a clinical condition in which patients who have undergone low back surgery continue to have pain and dysfunction. Said another way, the surgery that was intended to reduce pain and increase function has FAILED.
That’s right, the surgery failed. You had the surgery, struggled with the pain postoperatively, and diligently participated in physical therapy, and yet the pain and limitation are still there. Unfortunately, this occurs frequently. Estimates range from 20-40% of patients who undergo low back surgery will develop FBSS.
Is low back surgery the answer? Consider these facts.
Of patients who have lumbar disc surgery for disc herniation, 5-36% have a recurrence of their low back and leg pain within two years, while 29.2% of patients who have lumbar stenosis and undergo surgical decompression (laminectomy) have similar or increased pain at 12 months.
What Are the Symptoms of Failed Back Surgery Syndrome?
FBSS can manifest itself with a range of symptoms and complications, which can vary from one patient to another. The most common signs of a failed back surgery include pain, numbness, weakness, and tingling sensations that radiate from the lower back to the buttocks and lower body.
Other symptoms include slower recovery, back spasms, restricted mobility, and dependence on pain medications. From a mental health viewpoint, not seeing the desired results from your surgery can increase the risk of anxiety, depression, and social withdrawal.
Pain
Pain is the most common symptom of FBSS. It may be present immediately after surgery or gradually return over the following days to weeks. The severity of the pain may be the same or worse after surgery. It may be confined to the low back or can radiate into the buttock, posterior thigh, and down the leg.
You may also experience a different type of pain, or pain at a different level of your back than the location treated.
Numbness
Numbness indicates some degree of nerve compression. This can occur due to changes in the spine anatomy after surgery, as well as swelling, inflammation, or nerve injury – which are typical complications of back surgery. When your nerves are under persistent pressure, they become unable to effectively transmit signals relating to touch and sensation to the brain, leading to numbness.
If you’ve had spinal surgery that hasn’t entirely corrected the issue, numbness might be concentrated in the area that was surgically treated, such as your neck or lower back. However, if nerve roots, the spinal cord, or ganglia of nerves exiting the spine are impacted, you may experience this symptom in other parts of the body, as far as your hands and feet.
Weakness
Weakness in FBSS can occur due to a range of conditions. Entrapped or compressed nerves, for example, may fail to send signals relating to movement to the brain. This translates into muscle spasms, difficulty in gripping objects firmly with your hands, or keeping balance while walking (if the nerves that serve the muscles of the leg are affected).
You may also experience weakness and a sensation that your back will “give in” under loads and extreme fatigue.
Tingling Sensation
FBSS can also cause paresthesia, which refers to abnormal sensations of the skin, often described as tingling, numbness, or “pins and needles.” These sensations usually result from damage to peripheral nerves.
There may also be changes in the way you experience touch sensations. Improper transmission of nerve signals can cause you to feel extreme pain in response to stimuli that should be painless or only cause mild discomfort.
Causes of Failed Back Syndrome
Back surgery is considered to have failed if the outcome does not meet the pre-surgical expectations of both the patient and the healthcare provider. This definition leaves space for several different scenarios: you may not be as pain-free as you expected, your recovery may take longer, or the surgery may fail to address the underlying cause of your back condition.
Given the different possible ways in which this condition presents, it isn’t surprising that FBSS can occur for a number of reasons, which include preoperative, postoperative, and diagnostic factors.
Preoperative Factors
Pre-operative factors include:
- Obesity. Carrying excess body weight, as in cases of obesity, places significant stress on your spine and can complicate surgical recovery, increasing the risk of FBSS. Obesity is also a predictor of complications after lumbar spine surgery, including deep vein thrombosis, wound infection, urinary tract infection, embolism, acute renal failure, and sepsis.
- Smoking. Smoking is known to affect wound healing and blood flow, making it more likely for you to experience postoperative complications, including slow wound healing and FBSS.
- Workers’ compensation. Studies have found that compensation status may be a predictor of poor outcomes after lumbar spine surgery, with Workers’ Compensation patients having a delayed return to work.
- Ongoing litigation. The anxiety and stress often associated with ongoing litigation can inadvertently interfere with healing processes, exacerbating issues like FBSS after spinal surgery. What’s more, patients tend to not show significant improvements while litigation is still pending.
- Psychiatric disorders. Pre-existing psychiatric disorders like anxiety or depression can heighten pain perception and slow down recovery.
Postoperative Factors
Postoperative factors range from persistent pressure on the spinal cord, scar tissue pinching nerves, or improper healing after surgery. You can also consider mechanical instability following a procedure, which occurs if the spinal structure is disturbed or imbalanced.
Additionally, spine surgery involves removing important structural parts of the spine.
For example, a discectomy involves the removal of a portion or the entire intervertebral disc. Laminectomy is the removal of a bone (the lamina) from the backside of the spine that forms and protects the spinal canal. Supporting ligaments, tendons, and muscles are often damaged during these surgeries. The result is that the spine no longer functions the same.
Said another way, as a result of spine surgery, there is a change in the biomechanics of the spine. A classic example is spinal fusion. The diseased or injured disc is removed and the spinal bones are fused with screws and plates.
Remember that the disc acts like a shock absorber that absorbs and transfers the forces of daily living. After removing a given disc, the forces of daily living are redirected above and below the fusion. This places additional wear and tear on the discs and facet joints above and below the fusion. Over time, degeneration and injury occur, along with pain.
Diagnostic Factors
The successful outcome of low back surgery is dependent on the accurate diagnosis of the patient’s cause of pain. The misidentification of the original source of pain, such as blaming the discomfort on a disc issue when the real culprit is a nerve, is a common mistake.
This is especially true in the case of patients undergoing back surgery for nonspecific back pain (i.e.: back pain without an identifiable cause). Essentially, any missed or incorrect diagnoses can lead to failed back syndrome.
It is also important to keep in mind that surgeons are not objective, as their training and philosophy are biased toward surgery. They may only consider surgery as a solution to your problems where there are many other potential conservative treatment options that can help. If there is no surgical emergency, patients should always seek a non surgical opinion before seeing a surgeon or as a second opinion.
Common Myths About Surgery for Failed Back Syndrome
One of the greatest misconceptions about FBSS is that revision or repeat surgeries are the only way to fix the problem and improve symptoms. However, this choice isn’t free of risks.
According to studies, repeat spinal surgery offers diminishing results:
- Only around 50% of primary back surgeries are successful.
- No more than 30%, 15%, and 5% of the patients see successful outcomes after the second, third, and fourth surgeries, respectively.
In other words, the success rate of reoperation is low, and it will decline with additional procedures. At the same time, each primary or repeated intervention comes with risks and lengthy recovery times. Although most patients begin to feel better within 12 weeks of surgery, full recovery can take 6-12 months.
What’s more, given that most repeated surgeries aren’t successful, pain, discomfort, and instability can persist beyond these timelines.
Comprehensive Diagnostic Approaches to Failed Back Syndrome
Understanding FBSS – and designing non-invasive, effective treatment plans – requires a comprehensive diagnostic approach, focused on treating the spine as one functional spinal unit (FSU). An FSU refers to the smallest complete segment of the spine – i.e.: two adjacent vertebrae and their interconnecting tissues such as ligaments, facet joints, and muscles.
This concept is critical in the study and treatment of spinal disorders because it more accurately describes the intricate interplay among the spine’s various components, rather than viewing each component in isolation.
At the Centeno-Schultz Clinic (CSC), we recognize that zeroing in on just one problem within the spinal system (e.g.: lower back) and treating it as an isolated component can offset the system’s balance and create a cascade of complications.
For example, intervening to fix a degenerative intervertebral disc without addressing the underlying inflammation, posture, spinal stability, and lifestyle factors may not fix the problem and may cause changes in how loads are distributed in the spine. This can lead to pain and degeneration in other areas of the spine, ultimately feeding into the cycle of FBSS.
Our innovative diagnostic approach takes into account the interconnectedness of the spine’s components. This allows our specialists to design multidisciplinary, non-invasive interventions that bring the entire FSU – and the spine as a whole – into a harmonious balance, and prevent further episodes of chronic pain.
Common Treatment Options for Failed Back Syndrome
FBSS manifests in a variety, varying between patients. Some people may simply not see the results they were looking for, and others develop pain in other areas of the spine. In some cases, patients feel better for 5-10 years before experiencing pain again.
Nonetheless, when pain begins to interfere with your daily and social life, work, and health, it is important to find a treatment plan that tackles the root causes of this condition.
Below, we’ll look at the most common treatment options prescribed to manage the symptoms of FBSS, as well as their limitations. Being informed about the treatment options available can help you make decisions that will shield you from unnecessary side effects while being conducive to long-term health.
Physical Therapy
Physical therapy is often a component of a multidisciplinary algorithm of care for FBSS.
It focuses on enhancing posture, optimizing body mechanics, and reinforcing supporting muscular structures.
Guided by experts, strengthening and mobilization exercises can improve the stability of the spine, which can provide support to other musculoskeletal structures and relieve symptoms. Studies show that physical therapy can significantly improve the Visual Analog Scale and disability index in people with chronic back pain after one year.
Medication
Nonsteroidal anti-inflammatory drugs (NSAIDs), opioids, and even certain antidepressants may be utilized to ease pain temporarily. Similarly, nerve blocks and nerve pain medications like gabapentin and pregabalin can alleviate neuropathic discomfort.
Nonetheless, these should not be considered a long-term measure to regain your spinal function. These medications come with significant side effects, ranging from stomach ulcers, increased risk of heart failure, and somnolence to dependency and overdose.
What’s more, drugs fail to address the root cause of your condition, thus unnecessarily exposing you to risks and side effects without actually improving your clinical picture.
Surgery
Surgical interventions like spinal fusion, spinal cord stimulators, or even decompression surgery may all have a place in a comprehensive treatment for FBSS – but they should only be considered as a last resort.
As highlighted above, the benefits of these interventions can decline with repeated operations. Also, it is important not to dismiss the inherent risks associated with any surgical procedure.
Conservative Post-Operative Remedies for Failed Back Syndrome
Suffering from FBSS can have a detrimental effect on all aspects of your life – but there is a lot that you can do to relieve your symptoms and regain function without surgery. Below are some of the most common post-surgical remedies prescribed for patients with FBSS.
Rest
One of the simplest strategies for managing FBSS pain is through rest. When resting, the body can take care of essential functions such as managing energy production and use, healing damaged tissues, and strengthening the immune system. Not only does this speed up your recovery rate, but it can also prevent further injuries and reduce the risk of complications.
Be sure to rest as instructed by a specialist. Too much rest – such as ongoing bed rest and immobilization – may be detrimental to your spine health in that it can lead to muscle weakness, atrophy, and mental health conditions like depression.
Ideally, to strike the right balance between rest and physical activity, regular breaks and activity modification to reduce the strain on the spine should be preferred. In any case, you should listen to your body and never play through pain.
Activity Modification
Adjusting the way you perform daily activities or sports may help reduce strain on the spine, prevent further injuries, and speed up recovery. While it is important to work with a lifestyle counselor or occupational therapist to better understand how to modify your activities, some ways to get started include:
- Return to exercise gradually and stop if you experience pain.
- Switch to low-impact activities that safeguard your spine, like aquatic therapy, yoga, or swimming.
- Blend mindful disciplines, like tai chi or Pilates, into your routine to boost posture alignment, flexibility, and core strengthening.
- Prefer daily walks over sitting for prolonged periods to keep your spine flexibility and blood circulation in check.
- Redesign your work environment if needed, and opt for ergonomic furniture.
- Do chores mindfully – even simple tasks like lifting, bending, or gardening can aggravate your spine when done incorrectly.
Medication
Medications can be effective for symptom control. They work by blocking the pain signals sent to your brain, providing substantial – but, often, short-lived – relief. While they are often part of a multidisciplinary approach to pain management, it is important to use them wisely and within the limits recommended by a specialist (e.g.: for a short period, such as during flare-ups).
Common pain management medications include:
- NSAIDs. Non-steroidal anti-inflammatory drugs work by inhibiting the enzymes COX-1 and COX-2, thus reducing the production of pro-inflammatory prostaglandins. While NSAIDs are an affordable and accessible option to relieve inflammation and pain, they come with side effects like increased risk of heart failure, kidney failure, and stomach ulcers.
- Steroid injections. Corticosteroids are a type of anti-inflammatory medication designed to replicate the actions of cortisol, a hormone naturally produced by the adrenal glands responsible for controlling how the body responds to stress and inflammation. Taking corticosteroids regularly can lead to severe complications like cartilage damage (if injected into a joint), osteoporosis, bone death (osteonerosis), and adrenal insufficiency to name a few.
Complications from Spine Surgery on Failed Back Syndrome
FBSS has an array of potential complications, from neurophysiological changes to wound infections. Nearly 15% of patients begin to experience chronic back pain after spinal surgery. These complications can critically impact the quality of life and lead to physical limitations and emotional distress. Below, we’ll look at some of the most common ones.
Adjacent Segment Disease
The disc is an important shock absorber. Fusion surgery removes this important shock absorber, which places additional stress and forces on the discs and facet joints above and below the level of the fusion.
This additional force, in turn, can lead to injury of these facet joints and discs, leading to degeneration, arthritis, and pain. This is a real problem, with an incidence of 9%. This can lead to additional surgeries including fusions.
To learn more about this tragic complication please click on the video below.
Spinal Muscle Injury
The spinal muscles provide critical stability and support for the spine. The multifidus is a spinal muscle located deep in the low back. It is a major stabilizer of the spine.
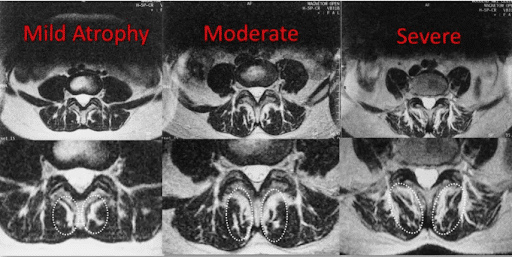
Unfortunately, lumbar fusion significantly compromises the health and integrity of this muscle (11). The multifidus muscle can actually shrink in size, which is called atrophy. This, in turn, can lead to spine instability, degeneration, arthritis, and pain. While this is easy to see on MRI, it is rarely commented on by the radiologist.
Below are MRI images of the lumbar spine in cross-section. Progressive atrophy is shown from left to right. The multifidus is identified by the white dashed ovals. As the muscle becomes more atrophied, the dark muscle is replaced by white fat.
This is minimal in the image on the left and is much more pronounced in the image to the far right. The atrophy of important spinal muscles leads to dysfunction and pain.
Instability
Surgery removes important structures in the spine. Surgery also can compromise ligaments, tendons, and muscles, all of which provide important support and stability. Spine surgery typically changes the architecture of the spine, which in turn can lead to instability, injury, and pain.
Infections
Surgical site infections (SSIs) are a common and serious complication that can occur post-operation. Researchers show that the incidence of SSIs is as high as 16.1% after spinal surgery, often caused by staphylococcus aureus and staphylococcus epidermidis.
SSIs can significantly impair recovery, worsen the patient’s condition, prolong hospital stay, and even lead to death. Risk factors for surgical infections include diabetes, a history of SSIs, obesity, and smoking.
Regenerative Options for Failed Back Syndrome
The doctors at the Centeno-Schultz Clinic are experts in the evaluation and treatment of low back pain and FBSS. In 2005, we were the first clinic in the world to inject stem cells into the lumbar disc.
Treatment options include platelet-rich plasma (PRP) and a patient’s own bone marrow-derived stem cells. All injections are performed under X-ray, or ultrasound guidance, or both. Damaged or weakened ligaments can be tightened. Muscles that are atrophied can be injected to stimulate growth.
Specialized platelet lysate made from PRP can reduce inflammation, improve blood flow, and accelerate repair and healing to spinal nerves. PRP or stem cells can help heal and protect damaged facet joint cartilage and reduce inflammation helping joint pain.
Injured discs can be injected with PRP and/or stem cells to fix annular tears and promote healing. Unlike other clinics, we track outcomes that are available here.
Release Yourself from Failed Back Syndrome
Suffering from failed back syndrome can be made exponentially worse by the prospect of having to undergo another surgery, face lengthy recovery times, and deal with long-lasting pain.
Fortunately, invasive interventions are no longer the only options to regain your spine function and quality of life. The non-invasive, non-drug approach pioneered by CSC can help you lay the foundations of long-term spine health without having to compromise your overall health.
Don’t let failed back syndrome get in the way of your life. Make an appointment with us today!

Christopher J. Centeno, MD
Christopher J. Centeno, M.D. is an international expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate in orthopedics.
Dr. Centeno is one of the few physicians in the world with extensive experience in the culture expansion of and clinical use of adult bone marrow concentrate to treat orthopedic injuries. His clinic incorporates a variety of revolutionary pain management techniques to bring its broad patient base relief and results. Dr. Centeno treats patients from all over the US who travel to Colorado to undergo innovative, non-surgical treatments. Dr. Centeno has chaired multiple international research-based conferences. He also maintains an active research-based practice, with multiple publications listed in the US National Library of Medicine. Dr. Centeno has also served as editor-in-chief of a medical research journal dedicated to traumatic injury.
Dr. Centeno trained at the Baylor College of Medicine, Texas Medical Center, and the Institute for Rehabilitation Research. He hails from both Florida and New York and currently resides in Boulder, Colorado with his wife and three children.

John Schultz, MD
John R. Schultz M.D. is a national expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate for orthopedic injuries. He is board certified in Anesthesiology and Pain Medicine and underwent fellowship training in both. Dr. Schultz has extensive experience with same day as well as culture expanded bone marrow concentrate and sees patients at the CSC Broomfield, Colorado Clinic, as well the Regenexx Clinic in Grand Cayman. Dr. Schultz emphasis is on the evaluation and treatment of thoracic and cervical disc, facet, nerve, and ligament injuries including the non-surgical treatment of Craniocervical instability (CCI). Dr. Schultz trained at George Washington School of…
Read more
John Pitts, M.D.
Dr. Pitts is originally from Chicago, IL but is a medical graduate of Vanderbilt School of Medicine in Nashville, TN. After Vanderbilt, he completed a residency in Physical Medicine and Rehabilitation (PM&R) at Emory University in Atlanta, GA. The focus of PM&R is the restoration of function and quality of life. In residency, he gained much experience in musculoskeletal medicine, rehabilitation, spine, and sports medicine along with some regenerative medicine. He also gained significant experience in fluoroscopically guided spinal procedures and peripheral injections. However, Dr. Pitts wanted to broaden his skills and treatment options beyond the current typical standards of care.
Read more
Jason Markle, D.O.
Post-residency, Dr. Markle was selected to the Interventional Orthopedic Fellowship program at the Centeno-Schultz Clinic. During his fellowship, he gained significant experience in the new field of Interventional Orthopedics and regenerative medicine, honing his skills in advanced injection techniques into the spine and joints treating patients with autologous, bone marrow concentrate and platelet solutions. Dr. Markle then accepted a full-time attending physician position at the Centeno-Schultz Clinic, where he both treats patients and trains Interventional Orthopedics fellows. Dr. Markle is an active member of the Interventional Orthopedic Foundation and serves as a course instructor, where he trains physicians from around the world.
Read more
Brandon T. Money, D.O., M.S.
Dr. Money is an Indiana native who now proudly calls Colorado home. He attended medical school at Kansas City University and then returned to Indiana to complete a Physical Medicine and Rehabilitation residency program at Indiana University, where he was trained on non-surgical methods to improve health and function as well as rehabilitative care following trauma, stroke, spinal cord injury, brain injury, etc. Dr. Money has been following the ideology behind Centeno-Schultz Clinic and Regenexx since he was in medical school, as he believed there had to be a better way to care for patients than the status quo. The human body has incredible healing capabilities…
Read moreOther Resources For Failed Back Syndrome
-
Spinal Fusion Complications Years Later – What You Should Know
Spinal fusion surgery, often performed to alleviate chronic back pain or spinal instability, can lead to complications years later. These may include adjacent segment disease, where nearby vertebrae deteriorate, chronic pain, or hardware failure. Patients might also experience limited mobility and nerve damage over time. Understanding these potential risks is crucial for long-term care and…
-
All You Need to Know about the L4 Vertebra
The L4 vertebra is one of the five vertebrae in the lower back, located just above the sacrum. It plays a crucial role in supporting the upper body’s weight and enabling movement. Injury or degenerative changes that affect the L4 vertebra can lead to chronic pain and mobility issues. Many patients often rely on medications…
-
Thoracic Spine Anatomy: What You Need To Know
What Is The Thoracic Spine? The thoracic spine refers to the section of the spinal column corresponding to the mid-back. It is between the cervical spine (neck) and the lumbar spine (low back). It consists of 12 boney building blocks called vertebral bodies that are labeled T1-T12. The T refers to the thoracic spine. The…
-
Craniocervical Instability & Ehlers Danlos Syndrome: Know the Facts
Gymnastics and yoga were easy as you were super flexible. With continued training your shoulders and knees kept popping out of place. A series of small but significant traumas left you sidelined both from athletics, academics and socially. Brain fog and fatigue were common themes. You have seen countless physicians with conflicting information. Your chiropractor…
-
What Is the Success Rate of C1-C2 Fusion?
The upper neck and head pain was unrelenting and did not responed to conservative care or medications. Your doctor wants to refer you to a surgeon for possible fusion. What is the C1? What is the C2? What is the Atlantoaxial (AA) Joint? What are the key components of the AA Joint? What is a…
-
How to Heal a Herniated Disc Naturally – Learn the Ways
A herniated disc can stop you in your tracks. Dr. Schultz reviews what a disc herniation is, how it is diagnosed, whether it can heal on its own, current treatments, and a natural way to treat a herniated disc.
-
Stem Cell Treatment for Foot Pain: Learn the Truth.
Foot pain can be debilitating. Dr. Schultz discusses the 7 major causes of foot pain, traditional treatment options, stem cell treatment options, the different types of stem cells, factors that will influence the specific stem cell treatment plan, and the advantages of stem cells over steroids and surgery.
-
9 Complications to Watch Out For After Cervical Fusion Surgery
A three-level cervical fusion is a major surgery with significant risks and complications. Dr. Schultz discusses what a cervical fusion is, its indications, different types, and the 9 key complications you need to know.
-
Rancher Returns To Work After Upper Cervical Procedure
Cranial Cervical Instability (CCI) is a medical condition where the strong ligaments that hold your head to your upper neck are loose or lax. Dr. Schultz discusses CCI, its causes, symptoms, treatment options, and a new, groundbreaking non-surgical treatment option.
-
Long-term Side Effects of Spinal Fusion
Spinal fusion is a major surgery where one or more of the spinal bones are fused together using screws, bolts, and plates. Dr. Schultz discusses spinal fusion complications long term and a novel approach to avoid fusion surgery.