Herniated Thoracic Disc
A herniated thoracic disc is a serious medical condition where the disc contents are extruded into the spinal canal. This can cause debilitating localized thoracic pain, lancinating pain across the chest wall, or injury to the spinal cord. Herniated thoracic discs are especially difficult because there aren’t as many treatments available as there are for disc herniations in other areas of the spine. To better understand herniated thoracic discs we first need to cover thoracic spine anatomy and function.
What is a Thoracic Herniated Disc?
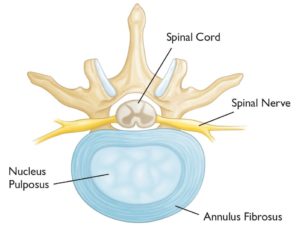
A disc is an important structure in the spine that acts as a shock absorber. It is composed of a thick fibrous sidewall called the annulus fibrous (sidewall of the disc) and an inner gelatinous center called the nucleus pulposus. Discs are sandwiched between the boney building bones of the spine and are present in the cervical, thoracic, and lumbar spine. The sidewall of the disc is susceptible to injury. A disc herniation involves the rupture of the disc sidewall with the inner gelatinous center being extruded into the spinal canal. The gelatinous center is very inflammatory and can cause debilitating pain. The extruded disc can also irritate or compromise exiting nerves causing burning pain across the chest wall. A large herniated thoracic disc can injure the spinal cord. A herniated thoracic disc is an injury of a disc in the thoracic spine that can cause significant pain, dysfunction, and potential spinal cord injury. It has an estimated frequency of 1 case per 1,000,000 people (1).
Symptoms of Thoracic Herniated Disc?
Big Toe Numbness
Believe it or not, one of those significant issues that can present as numbness stems from the low back. In the lumbar spine, the nerve that exits the spine at the L5 level branches down through the hip, thigh, knee, lower leg, and, yes, all the way into the foot and toes. So a pinched or irritated nerve at that L5 level in the back can create problems, such as pain, numbness, tingling, and so on, anywhere along the nerve branch. So what can irritate the L5 spinal nerve? The list is long, but it includes disc issues, such as herniated…
Read More About Big Toe NumbnessCalf Muscle Twitching
A twitching calf muscle may seem like no big deal, and if it’s just a temporary annoyance that lasts a couple of days and then goes away, it may be. However, it can also be a warning sign of something bigger, especially if it continues. So, today, we’re going to explain a little about the calf and why it’s not a good idea to ignore calf muscle twitching. If there’s one muscle you’re likely familiar with, it’s the calf muscle. If you reach around and grab your calf and flex it, the muscle you are actually feeling just under the surface is called the gastrocnemius muscle.
Read More About Calf Muscle TwitchingKnee Twitching & Spasms
Knee twitching and or spasms are common occurrences that can be caused by a variety of factors. In most cases, it is not a cause for concern and does not require treatment. However, in some instances, knee twitching may be a sign of a more serious condition. Knee twitching is often accompanied by a feeling of pins and needles or tingling in the knee. It may also be accompanied by a burning sensation. The twitching usually occurs intermittently and lasts for a few seconds. There are a number of things that can cause knee twitching. Some of the most common…
Read More About Knee Twitching & SpasmsNerve Pain in Knee
Nerve pain in the knee can be very irritating and life-altering during normal activities as well as leisurely pursuits. Nerve pain in the knee can radiate from the lumbar spine, the pelvis, or the small nerves in the knee. It also can begin after surgery from surgical nerve irritation from the incision or can be the type of pain related to knee arthritis. At the Centeno-Schultz Clinic, we are experts in spine, pain management, and non-surgical orthopedics. We perform a thorough physical examination and musculoskeletal ultrasound of your knee to identify the root cause of your pain and how to treat it appropriately….
Read More About Nerve Pain in KneeNerve Pain in the Thoracic Spine
The thoracic spine is the part of the spine below the neck (cervical spine) and above the low back (lumbar spine). It is often referred to as the mid back. Nerves exit the thoracic spine at each level and can become irritated, compressed or injured, resulting in pain and dysfunction. This is commonly referred to as thoracic radiculopathy or pinched nerve.
Read More About Nerve Pain in the Thoracic SpineReferred Pain From The Thoracic Spine
Pain is the body’s way of signaling distress or injury. But what if your body manifests pain in a certain area of your body and yet the actual source of the discomfort is a completely different part of your body? In this article, we will explore the intricacies of referred pain, specifically referred pain from the thoracic spine. We’ll explore what this typically feels like, what conditions commonly cause referred pain, and the treatment options available to treat the root cause of this symptom.
Read More About Referred Pain From The Thoracic SpineThoracic Spine Pain
Simply put thoracic spine pain is pain that arises from the thoracic spine. It may be acute or chronic. It may be constant or intermittent. It may be mild or can be so severe as to take your breath away. To better understand thoracic spine pain please review the sections below. The thoracic spine is that part of the spine that is sandwiched between the neck and low back. Many refer to it as the middle section of your spine. It starts at the base of your neck and ends at the bottom of your ribs. The thoracic spine is the longest region in the spine.
Read More About Thoracic Spine PainTight Hamstrings & Calves
The hamstrings are a group of muscles in the upper leg. They are located on the backside of the upper leg and are comprised of three muscles: biceps femoris, semitendinosus, and semimembranosus. The calf muscles are located on the backside of the lower leg and are comprised of two muscles: the gastrocnemius and soleus. Tight hamstring and calf muscles can be painful, limiting someone mobility. They also make lower extremity muscles more vulnerable to injuries. Tight hamstrings and calves can arise from different sources which include: medication, muscle and tendon injury, overuse, muscle imbalance, dehydration, poor posture, low back injury…
Read More About Tight Hamstrings & CalvesWeak in Knees
Weakness in the knee can be a symptom of many different knee conditions. Some of the most common causes of weakness in the knee include ligament tears, meniscus tears, and arthritis. Another important but often overlooked cause of knee weakness is irritation or injury of the nerves in the low back. If you are experiencing any type of weakness in your knee for long durations of time (3 weeks), it is important to see a doctor to determine the cause. Some of the most common symptoms of knee weakness include difficulty standing up from a seated position, difficulty walking, climbing or descending stairs…
Read More About Weak in KneesThere can be significant variability in symptoms in patients with thoracic herniated discs. The severity and symptoms often correlate with the size and location of the disc herniation. Thoracic herniated discs mostly affect the lower part of the thoracic spine. 75% of thoracic disc herniations occur below T7/8 and are common in adults between 30-50 years of age (2).
Pain
Pain is the most common symptom associated with a thoracic herniated disc or bulging disc in the thoracic spine. The pain may be sharp and stabbing in nature, or a generalized ache. It may be localized to a specific region of the thoracic spine or can radiate across the chest wall, arms, and stomach. The pain may have abrupt onset after a traumatic injury or may start as a mild discomfort that progresses to constant, unrelenting pain.
Headaches
Thoracic herniated discs can trigger headaches as a result of muscle spasms and tension. The headaches can be mild to moderate involving the base of the skull (occiput) as well as in the forehead and behind the eyes.
Weakness and Motion Difficulties
A thoracic disc herniation involves the rupture of the disc sidewall with the inner gelatinous center being extruded into the spinal canal. The extruded disc material may irritate or cause injury to the spinal cord. Symptoms vary depending upon the severity of the spinal cord injury but include leg weakness and problems with balance or walking. Symptoms that suggest spinal cord injury and require medical attention include:
- Bowel or bladder incontinence
- Difficulty breathing
- Numbness and weakness in legs, ankles, and feet.
Common Causes of Thoracic Herniated Disc
Thoracic discs can be damaged in many different ways. The most common include:
Traumatic
A common cause of thoracic disc herniation is trauma such as a motor vehicle accident or fall. The abrupt forces disrupt the thoracic disc sidewall resulting in disc herniation.
Genetic Issues
A number of studies have shown an association between genetic influences and disc degeneration (3).
Age-Related Changes
The aging process involves gradual wear and tear on the discs in the spine. These degenerative changes make them more susceptible to injuries such as disc protrusion or thoracic herniated disc.
Poor Posture
Neural spinal alignment is key for the health and vitality of the spine. Poor posture can cause excessive pressure and force on the thoracic discs and facets resulting in injury and pain. The aging process can also contribute to poor posture as a result of a condition called kyphosis. This is an exaggerated forward curve and rounding of the spine. It is often times referred to as hunchback. It occurs in part due to the disc becoming stiffer and less flexible with age. The exaggerated forward curve places additional pressure on the front portion of the disc (anterior) making them susceptible to injury including disc protrusion and herniation.

Common Treatments for Thoracic Herniated Disc
Disc Replacement Surgery
The surgeon first accesses the spinal column (for example, in the cervical spine, the surgeon would access the spine through an incision in the front of the neck). From here the surgery is quite aggressive as the disc is scraped and chiseled out of the disc space. Pins are screwed into the vertebrae above and below the disc space that will anchor the space in place as the surgeon works. A tool is inserted into the disc space and used to further separate the upper and lower vertebrae, enlarging the space. The vertebrae surfaces within the disc space are prepared…
Read More About Disc Replacement SurgeryPerc-FSU – Trusted Alternative to Spinal Fusion
The Perc-FSU Procedure is an injection-based treatment that utilizes the patients’ own blood platelets to bring stability to the spine without the need for the rods, nuts, bolts, and hardware of fusion surgery. “Perc” stands for percutaneous, and “FSU” stands for “Functional Spinal Unit,” which means that the spine is treated as one functioning unit. Up and down the spine, the discs, facet joints, ligaments, and muscles that assist in stabilizing the spine are treated with image-guided injections of PRP and Platelet Lysate to help bring stability to the spine as a whole. It is the trusted alternative to spinal fusion.
Read More About Perc-FSU – Trusted Alternative to Spinal FusionProlotherapy For Thoracic Pain
Prolotherapy is an injection based regenerative therapy used in the treatment of ligament, tendon, muscle and spine injuries. It is minimally invasive and involves the injection of an irritant such as dextrose into the damaged or painful area. The injected irritant stimulates a delayed or frozen healing cycle thereby increasing blood flow and tissue healing. The thoracic spine is that section of the spine that is below the neck and above the low back. It is also referred to as the mid back. It has multiple components that include: Vertebral Bodies: Boney building blocks that stack one upon another…
Read More About Prolotherapy For Thoracic PainProlotherapy Injections
It has been successful in the treatment of many disorders including neck, shoulder, knee, and ankle pain. Dr. Centeno recently published an article in The Journal of Prolotherapy in which he discusses the use of x-ray guidance with prolotherapy. This ensures that the injection is in the correct place to maximize clinical results. Dr. Centeno discusses the use of prolotherapy for the treatment of neck, knee, sacroiliac joint, ankle, ischial tuberosity, and shoulder pain. At the Centeno-Schultz Clinic x-ray guided prolotherapy is just one of the therapies utilized in the successful treatment of pain. Regenerative injection therapy (RIT) or prolotherapy…
Read More About Prolotherapy InjectionsPRP Injections
PRP is short for platelet-rich plasma, and it is autologous blood with concentrations of platelets above baseline values. The potential benefit of platelet-rich plasma has received considerable interest due to the appeal of a simple, safe, and minimally invasive method of applying growth factors. PRP treatments are a form of regenerative medicine that utilizes the blood healing factors to help the body repair itself by means of injecting PRP into the damaged tissue. In regenerative orthopedics, it is typically used for the treatment of muscle strains, tears, ligament and tendon tears, minor arthritis, and joint instability. There have been more than 30 randomized controlled trials of PRP…
Read More About PRP InjectionsThoracic Herniated Disc Surgery
Disc herniation is a painful medical condition in which the central portion of the disc is pushed outside of the disc and into the spinal canal. This occurs due to a weakness or injury to the outer sidewall of the disc. Pain, muscle spasm, muscle weakness, and numbness can occur. It can occur in the neck, low back, and thoracic spine. When conservative treatments fail, patients are often referred for thoracic herniated disc surgery. The goal of thoracic herniated disc surgery is to remove that portion of the herniated disc that is responsible for the ongoing pain and compression of the nerves.
Read More About Thoracic Herniated Disc SurgeryThoracic Spine Surgery
Thoracic spine surgery is a major surgery aimed at treating injuries in the thoracic spine. Because of the complex anatomy and close proximity to the heart and lungs, there are significant surgical risks and complications. Surgery on the thoracic spine can take hours and may require deflating the lung in order to gain access to the thoracic injury. Recovery can be lengthy depending upon the specific thoracic spine surgery performed. There are several different types of thoracic spine surgery. The specific thoracic spine performed depends upon the underlying thoracic injury and a symptoms of the patient. For example, a thoracic disc herniation…
Read More About Thoracic Spine SurgeryThe management and treatment for thoracic herniated discs vary depending upon the size of the herniated disc, its location, and proximity to exiting nerve roots and the spinal cord. Symptoms can also vary from mild discomfort to severe pain with leg weakness and numbness. Treatment when appropriate should always start with conservative care. When this fails pain medication and injections are often recommended. Thoracic surgery is typically reserved for thoracic herniated discs that have failed conservative and injection therapy and are causing significant neurologic symptoms.
Conservative Options
When appropriate conservative therapy should always be the first step. Depending upon symptoms this may include a short period of rest and observation or physical therapy, acupuncture, laser, and ultrasound. Gentle exercises, such as walking are a good way to return to activity when tolerated.
Medications
When conservative care has failed to provide significant and sustained results, medications are often recommended. These are typically in 4 distinct groups. It is important to note that the medications do nothing to treat the actual disc herniation. Rather the medications help with reducing the symptoms associated with the injury.
Anti-inflammatory agents
Common examples include ibuprofen, diclofenac and naproxen. The medications aim to reduce inflammation and pain. There are significant side effects..
Muscle Relaxants
Common examples include Flexeril, Robaxin, and Zaniflex. These medications reduce the muscle spasm and pain associated with thoracic herniated discs and bulging thoracic discs.
Nerve Medications
Common examples include Neurontin, Lyrica, and Cymbalta. These medications aim to reduce nerve-related symptoms and pain.
Narcotics/ Opioids
Narcotics are powerful pain medications that aim to reduce moderate to severe pain, and stiffness. Common examples include Percocet ( oxycodone), Vicodin (hydrocodone), and Dilaudid (hydromorphone). All narcotics have significant addiction risks and should be closely monitored and minimized.
Corticosteroid Epidurals
When conservative and medication management has failed, many patients are referred for corticosteroid epidural injections. Corticosteroids are powerful anti-inflammatory agents. Common examples include hydrocortisone, triamcinolone, and methylprednisolone. An epidural is a medical procedure where a needle is placed into the potential space that surrounds the spinal cord and exiting nerves. It is most commonly associated with childbirth where the goal is to reduce the pain associated with labor and childbirth. Epidural injections are also used extensively to treat disc injuries such as herniated thoracic discs.
Corticosteroids are associated with significant long-term side effects…
a quick video outlining why corticosteroids actually have negative long-term detrimental side effects.
Surgical Options
The are many different approaches and surgeries for thoracic disc injuries. Specific treatment will depend upon many factors that include:
- Size and location of a thoracic herniated disc
- Proximity to exiting nerves and spinal cord
- A patient’s symptoms
- Response to conservative therapy
- Presence or absence of significant medical problems including lung disease, heart disease, and increased BMI.
The three major surgical options for thoracic herniated discs are:
Laminectomy
A major surgical procedure where a portion of the vertebra, the boney building block of the spine is removed in an attempt to open the spinal canal. The lamina is located on the backside of the spine and is the portion of the vertebral body that is surgically removed in a laminectomy. The surgery is commonly performed in cases of spinal canal narrowing which is called stenosis. There are significant risks associated with thoracic laminectomy surgery which include dural tear, dural leaks, infection, bleeding, and compromised neurologic function (4).
Discectomy
Thoracic discectomy is a major surgical procedure where a portion of the affected thoracic disc is surgically trimmed or removed. The goal of the surgery is to relieve the pressure, irritation, and injury to the exiting nerve or spinal cord caused by the thoracic herniated disc. Risks are significant and include dural tears, dural leaks, bleeding, paralysis, loss of bowel and bladder, blood clot to the lungs (pulmonary embolism), pneumonia, and punctured lung (5).
Fusion
Thoracic fusion is a major surgery where the thoracic disc is removed and the adjacent bones ( vertebral bodies) are joined together using hardware. Risks as similar to those associated with thoracic laminectomy and discectomy. An additional risk is called adjacent segment disease (ASD). This is a condition following fusion surgery where the discs and facet joints above and below the fusion break down as a result of the additional forces applied. To learn more about adjacent segment disease please click on the video below.
Regenexx
Regenexx is a nonsurgical treatment option for herniated thoracic discs. It uses proprietary, research-based methods, and patented protocols to treat common orthopedic conditions that include the thoracic facet and disc injuries. These are highly skilled injections that your PCP, orthopedist, or pain physician can not perform. Treatment options include PRP (platelet-rich plasma) and bone marrow-derived stem cells which can aid in the healing process. To learn more about how Regenexx procedures are very different please click on the video below.
Thoracic Spine Anatomy and Function
Your thoracic spine is the section of the spine that connects your neck (cervical spine) to your low back (lumbar spine). It is made up of bones called vertebrae (boney building blocks) that are stacked on top of each other. Sandwiched between each boney building block is a disc. The disc is a very important structure as it acts as a shock absorber and allows the spine to be flexible. Each disc is compromised a thick fibrous sidewall that surrounds a gelatinous center. The sidewall is called the annulus fibrous and the soft center is called the nucleus pulposus. The annulus is susceptible to injury and degeneration which can result in a bulging disc in the thoracic spine. A herniated disk in the thoracic spine is when the gelatinous center is pushed out through the fibrous side wall (annulus fibrosis) and into the spinal canal causing inflammation and potential injury to the exiting spinal nerves and spinal cord.
There are 12 vertebral bodies and 11 discs in the thoracic spine.
The thoracic spine has many important functions that include:
- Protection of the heart, lungs, and other internal organs.
- Protects the spinal cord and exiting nerves
- Attachment sites for many muscles in the body. Examples include latissimus dorsi and rhomboids.
- Provides attachments for the ribs
- Allow flexibility and movement
- Aids in respiration
- Supports the chest and torso
.
Managing Thoracic Herniated Disc Pain
A herniated thoracic disc is a serious medical condition in which the contents of the thoracic disc are extruded into the spinal canal. The most common symptom of a thoracic herniated disc is pain. Other symptoms include headaches, stiffness, leg weakness, and difficulty walking. Symptoms of a herniated disk in the thoracic spine that require immediate medical attention include bowel and bladder incontinence, difficulty breathing, and abrupt onset of leg numbness and weakness.
The most common causes of thoracic herniated discs include trauma, genetic predisposition, age-related changes, and poor posture. Treatment varies depending upon the size and location of the herniation, and patient symptoms. When appropriate conservative therapy should always be the first step. Medications are often utilized and include anti-inflammatory agents, muscle relaxants, nerve medications, and narcotics. Corticosteroid epidural injections are a medical procedure where high-dose steroids are injected near the thoracic disc injury aiming to reduce inflammation and pain.
Surgery treatments include laminectomy, discectomy, and thoracic spinal fusion. All are associated with significant risks and complications.
Regenexx offers nonsurgical treatments utilizing PRP and bone marrow-derived stem cells that are injected under x-ray or ultrasound guidance into the areas of tissue injury.
The pain and dysfunction of a herniated disc in the thoracic spine can keep you on the sidelines and erode your quality of life. Narcotics do not address the underlying problem and carry the risk of addiction. Surgery is no guarantee that the pain will decrease and is associated with significant long-term complications.
At the Centeno-Schultz Clinic, we are experts in the evaluation and nonsurgical treatment of thoracic spine pain. If you or a loved one suffers from persistent thoracic pain that has not responded to conservative care please a new patient evaluation. For those not in the Denver Boulder area we offer telemedicine appointments. A board-certified, fellowship-trained physician will compassionately review your history, symptoms, and radiographic studies and discuss possible treatment options. To schedule please contact Jen at 720-287-7196 or [email protected] or Vanessa at [email protected]. It is time to stop suffering and start living life to its fullest.
Our Doctors That Assist With Thoracic Herniations
John Schultz, MD
John R. Schultz M.D. is a national expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate and PRP for orthopedic injuries. He is board certified in Anesthesiology and Pain Medicine and underwent fellowship training. Dr. Schultz has extensive experience with same day as well as culture expanded bone marrow concentrate and sees patients at the CSC Broomfield, Colorado Clinic, as well the Regenexx Clinic in Grand Cayman. Dr. Schultz emphasis is on the evaluation and treatment of thoracic and cervical disc, facet, nerve, and ligament injuries including the non-surgical treatment of Craniocervical instability (CCI).
More Resources
-
Understanding the Thoracic and Lumbar Spines
The thoracic spine and lumbar spine make up a vital nexus of stability and mobility in the human body. In this exploration, we delve into the biomechanics and complexities that define these regions, unraveling their significance in posture, movement, and overall well-being. Understanding the thoracic and lumbar spine not only illustrates the mechanics of our…
-
Understanding the Role Of The Thoracic Spine Muscles
The thoracic spine plays a critical role in the stability and mobility of the upper body. Comprised of twelve vertebrae and an intricate network of muscles and ligaments, it serves as a central pillar supporting the structure and movement of the body. Understanding the role and function of thoracic spine muscles is pivotal for anyone…
-
Degenerative Changes Of The Thoracic Spine
Degenerative changes of the thoracic spine involve the gradual loss of normal structure and function over time. There are several different causes which are discussed in detail below. The thoracic spine is composed of many different and important components that are susceptible, both to injury and generalized wear and tear. The degeneration can occur in…
-
The Ultimate Guide To Thoracic Spine Exercises
Thoracic spine exercises are important for several reasons. First, they can help improve thoracic mobility, reducing the risk of spinal injuries and improving posture. Second, they can help to strengthen the muscles of the upper back and shoulders. Finally, thoracic spine exercises can help improve breathing mechanics. What Is Thoracic Spine? The thoracic spine, also…
-
Where Is The Thoracic Spine?
The thoracic spine is a region of the spine that is located in the middle back. It is located below the cervical spine and above the lumbar spine. It is composed of 12 vertebrae that are numbered T1-12. The T denotes the thoracic spine. It has many important functions which are discussed below. Location Of The…
-
Symptoms of Thoracic Herniated Disc
Your mid back pain has been unrelenting since the accident. Rest, medications, and physical therapy have failed to provide significant or sustained benefits. Your doctor thinks you have a thoracic disc herniation and thinks you have a thoracic herniated disc. What are the symptoms? And what can you do? Let’s dig in. What Is A…
1.Quint U, Bordon G, Preissl I, Sanner C, Rosenthal D. Thoracoscopic treatment for single level symptomatic thoracic disc herniation: a prospective followed cohort study in a group of 167 consecutive cases. Eur Spine J. 2012 Apr;21(4):637-45. doi: 10.1007/s00586-011-2103-0. Epub 2011 Dec 10. PMID: 22160099; PMCID: PMC3326138.
2.Kim YJ, Bridwell KH, Lenke LG, Rhim S, Cheh G. Sagittal thoracic decompensation following long adult lumbar spinal instrumentation and fusion to L5 or S1: causes, prevalence, and risk factor analysis. Spine (Phila Pa 1976). 2006 Sep 15;31(20):2359-66. doi: 10.1097/01.brs.0000238969.59928.73. PMID: 16985465.
3.Sambrook PN, MacGregor AJ, Spector TD. Genetic influences on cervical and lumbar disc degeneration: a magnetic resonance imaging study in twins. Arthritis Rheum. 1999 Feb;42(2):366-72. doi: 10.1002/1529-0131(199902)42:2<366::AID-ANR20>3.0.CO;2-6. PMID: 10025932.
4.Osman NS, Cheung ZB, Hussain AK, Phan K, Arvind V, Vig KS, Vargas L, Kim JS, Cho SK. Outcomes and Complications Following Laminectomy Alone for Thoracic Myelopathy due to Ossified Ligamentum Flavum: A Systematic Review and Meta-Analysis. Spine (Phila Pa 1976). 2018 Jul 15;43(14):E842-E848. doi: 10.1097/BRS.0000000000002563. PMID: 29940604; PMCID: PMC6252088.
5.Fessler RG, Sturgill M. Review: complications of surgery for thoracic disc disease. Surg Neurol. 1998 Jun;49(6):609-18. doi: 10.1016/s0090-3019(97)00434-5. PMID: 9637620.