Degenerative changes of the thoracic spine involve the gradual loss of normal structure and function over time. There are several different causes which are discussed in detail below.
- How Degenerative Changes Occur
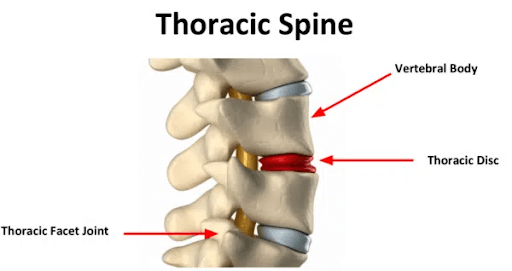
The thoracic spine is composed of many different and important components that are susceptible, both to injury and generalized wear and tear. The degeneration can occur in one section of the thoracic spine or can involve the entire spine. Degenerative changes in one section of the spine can lead to degeneration in other areas.
The most common areas that are susceptible to degeneration include:
- Thoracic Disc
- Thoracic Facet Joints
- Thoracic Costotransverse Joints
- Thoracic Ligaments
Four Conditions That May Cause Degenerative Changes In The Thoracic Spine
The gradual loss of normal structure and function in the thoracic spine can occur for many reasons. The four most common conditions that may cause degeneration in the thoracic spine are discussed below.
1. Degenerative Joint Disease
There are 3 major joints in the thoracic spine that are susceptible to injury and degeneration:
- Thoracic Facet Joint: A paired joint on the backside of the spine that is lined with cartilage. It functions to limit movement, provide stability, and absorb the forces of daily living (8).
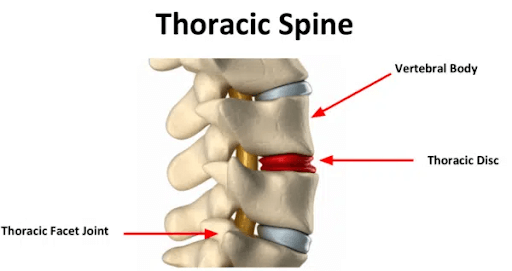
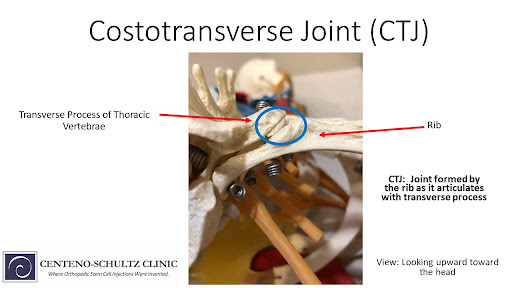
- Thoracic Costotransverse Joint: This joint is formed where the rib connects with the transverse process of the spine. There is a costotransverse joint on the left and the right at each level of the thoracic spine. It is lined with cartilage and surrounded by a thick capsule. It is susceptible to injury and degeneration causing pain and restriction in range of motion.
Thoracic Costovertebral Joint: This joint is formed where the rib head meets with the vertebral body. It is lined with cartilage and surrounded by a thick capsule.
Symptoms
Most common symptoms associated with thoracic degenerative joint disease are pain, stiffness, and restriction in range of motion. The pain can be mild, moderate, or severe depending upon the severity of the injury. It can be unilateral or bilateral and onset is typically gradual.
If thoracic degenerative joint disease is progressive in nature it can also irritate or compress the existing nerves causing radiating pain across the chest wall, around the ribs or into the abdomen. If the spinal cord is compromised, patients may complain of lower extremity numbness, weakness, and difficulty walking.
Risk Factors
Common risk factors for thoracic degenerative joint disease include:
- Thoracic degenerative disc disease: Reduction in disc height and function places additional stress on the thoracic facet and costotransverse joints leading to potential injury and degeneration.
- Repetitive Stress Injuries: This can include repeated strenuous activity such as heavy lifting.
- Scoliosis: A sideways curve of the spine can overload the thoracic joints leading to injury and degeneration
Conventional Treatment
When appropriate, conservative care should always be the first line of treatment. This would include rest, lifestyle modification, gentle stretching, physical therapy, massage, acupuncture, chiropractic care, and oral anti-inflammatory medications.
If conservative care fails, some providers will provide oral steroids in an attempt to reduce inflammation, pain, and restriction in range of motion.
If pain persists, despite conservative treatment and oral steroids, patients may be referred to steroid pain injections. Thoracic facet and costotransverse joint injections are not common due to the potential complications including collapse of the lung. Steroid injections should be avoided given the significant side effects.
2. Degenerative Disc Disease
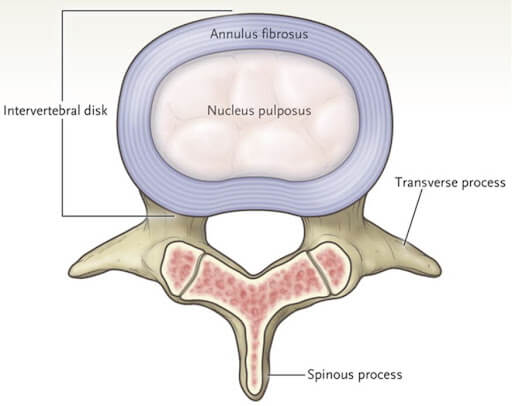
The thoracic spine is composed of 12 boney building blocks that stack one upon another. They are called vertebral bodies. Sandwiched between the vertebral bodies is the disc which allows for motion and flexibility in addition to acting as shock absorber (7).
The disc is composed of two principal structures: annulus fibrous and nucleus pulpous. The annulus is composed of the strong outer fibers that provide support. The nucleus pulpous is the gelatinous center.
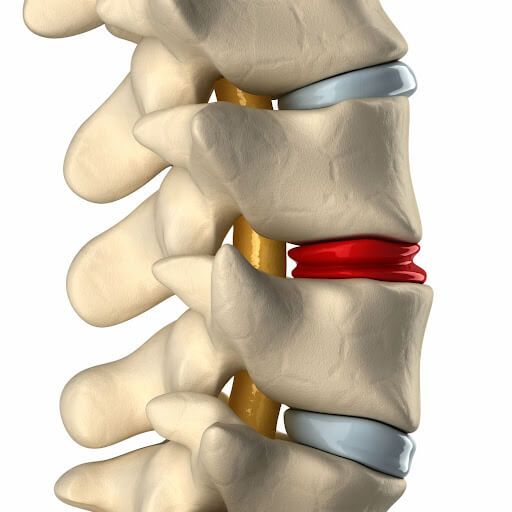
The disc has very little blood supply and is susceptible to injury and degeneration. The main factor in the degeneration of the disc is the loss of proteins which affect the amount of water within the disc and its ability to absorb the forces of daily living.
It is estimated that only 0.25-1% of all disc herniations occur in the thoracic region (7). Injury occurs most frequently in the lower levels in the thoracic spine ( T7-11).
Symptoms
The major symptoms associated with thoracic degenerative disc disease include:
- Pain: Can be constant or intermittent with varying intensity. The quality of the pain can be aching and throbbing like a toothache or burning and electrical. It may be confined to a discrete area or may be diffuse and involve the entire thoracic spine. It can radiate across the chest or into the abdomen if a nerve is being irritated or compressed.
- Stiffness and restriction in range of motion: Restriction may be most evident in early morning upon awakening
- Muscle spasm: May be localized to one side or can involve the entire thoracic spine.
- Numbness and Weakness: Irritation or compression of nerves or the spinal cord can lead to weakness and numbness making walking difficult at times.
Risk Factors
Factors influencing disc degeneration include:
- Mechanical Stress: Lifting, carrying or pushing heavy loads can lead to thoracic disc degeneration (7).
- Trauma
- Genetic Factors: There may be family history of thoracic disc degeneration.
- Nutritional Disorders: The disc has a very poor blood supply and is dependent upon diffusion for nutrients. Nutrient disorders can lead to disc degeneration (8).
Conventional Treatment
When appropriate conservative care should always be the first line treatment. Natural treatments include rest, ice, heat, exercise, and support. Medications can help with pain and restriction in range of motion and include NSAIDs and muscle relaxants.
Steroids are a common treatment for thoracic degenerative disc disease when conservative treatment fails. Steroids can be administered orally or injected. Oral steroids are commonly referred to as dose packs and include 21 tablets that are tapered over several days.
Steroids, when injected into the muscle and absorbed by the bloodstream, provide widespread reduction in inflammation. Common examples include Solumedrol, Betamethasone, and Decadron.
When conservative therapy fails to provide significant or sustained benefit, patients may be referred for thoracic epidural steroid injections. This is a medical procedure in which powerful anti-inflammatory agents are injected through a needle into the area of tissue injury or damage. The procedures are typically performed in an ambulatory surgery center or pain clinic. Thoracic spine steroid injections are complex procedures that your local orthopedic doctor or PCP can not perform. There are risks which include bleeding, infection, failure, and injury to the lung. To learn more about steroid injections, please click here.
Alternative Treatment Options for Thoracic Degenerative Disc Disease
You can click this page to gain a better understanding of your options for alternative treatments for thoracic degenerative disc disease.
3. Herniated Disc
A herniated disc and a degenerative disc are not the same and it is important to understand the differences. A brief review of anatomy is important.
A disc in the spine acts as a shock absorber. It is composed of a thick fibrous sidewall called the annulus fibrosus and the inner gelatinous center is called the nucleus pulposus.
A disc herniation is a painful medical condition in which the gelatinous center is pushed out of the disc and into the spinal canal due to tear or rupture in the thick sidewall. It contains a large number of inflammatory agents which can cause significant pain and dysfunction. A disc herniation is abrupt in nature and can take your breath away.
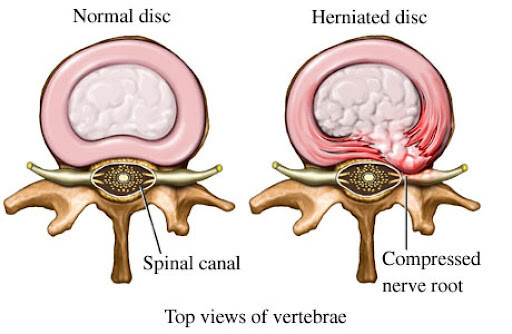
In contrast, a degenerative disc is a disc that has lost its structure and function. It is typically a gradual process and starts with only mild structural changes. Overtime, the degeneration progress continues with loss of structure, function and an increase in pain and restriction in range of motion.
Symptoms
There can be significant variability in symptoms in patients with thoracic herniated discs. The severity of the symptoms often correlate with the size and location of the disc herniation. Disc herniations in the thoracic spine most frequently occur in the lower part of the thoracic spine. 75% of thoracic disc herniations occur below T7/6 and are common in adults between 30-50 years of age (7).
Risk Factors
The most common causes of thoracic disc herniation are:
Trauma.
- Genetic Issues: A number of studies have shown an association between genetic influences and disc injuries (8).
- Poor Posture: Neural spinal alignment is key for the health and vitality of the spine. Poor posture can cause excessive pressure and force on the thoracic discs and facets resulting in injury including disc protrusions and herniation.
- Age-related changes: The aging process involves gradual wear and tear on the discs in the spine. These degenerative changes make them more susceptible to injuries such as disc protrusion or thoracic herniated disc.
Conventional Treatment
Please see thoracic herniated disc post where all treatments are discussed.
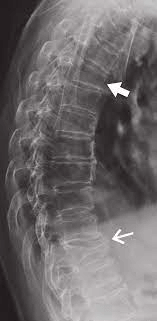
4. Thoracic Spondylosis
Spondylosis is a medical term that refers to a degenerative condition that affects the joints and discs in the spine. It is a common condition that occurs due to cumulative wear and tear in the spine. This can also be due to aging and or injury. Thoracic spondylosis is a degenerative process that affects the thoracic spine.
Symptoms
Symptoms can vary from patient to patient but may include:
Pain in the mid back. It can be intermittent or constant.
Stiffness with restriction in range of motion.
Numbness and tingling may occur and are due to nerve irritation. As the condition progresses, the numbness may spread to the other parts of the body such as the arms, legs and hands. In severe cases, thoracic spondylosis can also lead to muscle weakness, loss of balance and difficulty walking.
Risk Factors
Please see this page for further information. The major causes of thoracic spondylosis is
- Aging: With age, there is a generalized wear and tear on the thoracic spine
- Poor Posture: Poor posture for extended periods can cause excessive stress on the thoracic vertebrae, discs, facet joints, and ligaments and can lead to the development of thoracic spondylosis.
- Repetitive Strain: Activities that involve repetitive movement or heavy lifting can cause wear and tear on the spine, leading to spondylosis.
- Trauma: Trauma to the spine, such as a fall or car accident, can cause damage to the thoracic disc, facet joints, and ligaments and this can lead to spondylosis.
Find The Right Treatment For Degenerative Changes In Your Thoracic Spine
Degenerative changes of the thoracic spine involve the gradual loss of normal structure and function over time. The thoracic spine is composed for 5 principal components all of which are susceptible to degenerative changes. These include:
- Thoracic Discs
- Thoracic Facet joints
- Costotransverse joints
- Thoracic Ligaments
- Thoracic Tendons
The most common causes of degenerative changes in the thoracic spine are:
- Degenerative joint disease
- Degenerative Disc Disease
- Herniated Disc
Thoracic Spondylosis: Spondylosis is a medical tear that refers to a degenerative condition that affects the joints and discs in the spine. It is a common condition that occurs due to cumulative wear and tear in the spine. It can also occur due to aging or traumatic injury.
To minimize degenerative changes in the thoracic spine it is important to stay active, maintain good posture and treat small injuries in the disc, facet joints, ligaments, and tendons when they are small. If left untreated, these injuries can progress–leading to significant and potentially permanent degenerative changes in the thoracic spine.
At the Centeno-Schultz Clinic, we are the experts in the evaluation and treatment of thoracic spine injuries. Our board certified and fellowship trained physicians can provide an accurate diagnosis based upon history, examination, and radiographic information.
An appropriate treatment plan can be designed that will address the injuries and guard against significant degeneration of the spine. Treatment of small problems prevents larger problems down the line.
It’s never too late to treat degenerative changes in the thoracic spine. Schedule an appointment today to discuss your options.
References:
- Urban JP, Smith S, Fairbank JC. Nutrition of the intervertebral disc. Spine (Phila Pa 1976). 2004 Dec 1;29(23):2700-9. doi: 10.1097/01.brs.0000146499.97948.52. PMID: 15564919.
- Jaumard NV, Welch WC, Winkelstein BA. Spinal facet joint biomechanics and mechanotransduction in normal, injury and degenerative conditions. J Biomech Eng. 2011 Jul;133(7):071010. doi: 10.1115/1.4004493. PMID: 21823749; PMCID: PMC3705911.
- Erwin WM, Hood KE. The cellular and molecular biology of the intervertebral disc: A clinician’s primer. J Can Chiropr Assoc. 2014 Sep;58(3):246-57. PMID: 25202152; PMCID: PMC4139773.
- Roughley PJ. Biology of intervertebral disc aging and degeneration: involvement of the extracellular matrix. Spine (Phila Pa 1976). 2004 Dec 1;29(23):2691-9. doi: 10.1097/01.brs.0000146101.53784.b1. PMID: 15564918.
- Kos N, Gradisnik L, Velnar T. A Brief Review of the Degenerative Intervertebral Disc Disease. Med Arch. 2019 Dec;73(6):421-424. doi: 10.5455/medarh.2019.73.421-424. PMID: 32082013; PMCID: PMC7007629.
- Urban JP, Smith S, Fairbank JC. Nutrition of the intervertebral disc. Spine (Phila Pa 1976). 2004 Dec 1;29(23):2700-9. doi: 10.1097/01.brs.0000146499.97948.52. PMID: 15564919.
- Kim YJ, Bridwell KH, Lenke LG, Rhim S, Cheh G. Sagittal thoracic decompensation following long adult lumbar spinal instrumentation and fusion to L5 or S1: causes, prevalence, and risk factor analysis. Spine (Phila Pa 1976). 2006 Sep 15;31(20):2359-66. doi: 10.1097/01.brs.0000238969.59928.73. PMID: 16985465.
- Sambrook PN, MacGregor AJ, Spector TD. Genetic influences on cervical and lumbar disc degeneration: a magnetic resonance imaging study in twins. Arthritis Rheum. 1999 Feb;42(2):366-72. doi: 10.1002/1529-0131(199902)42:2<366::AID-ANR20>3.0.CO;2-6. PMID: 10025932.