Cervical Spine Injections: Powerful Relief or Potential Risks?
Am I a Candidate?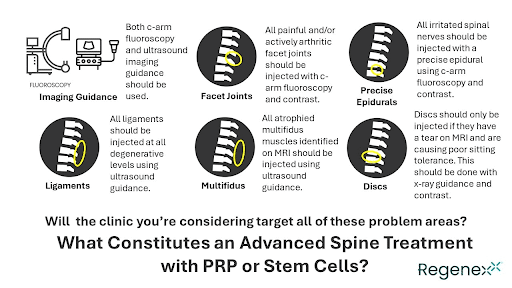
Cervical spine injections involve the administration of medications directly into the cervical (neck) region to alleviate pain and inflammation associated with various spinal conditions, such as herniated discs, spinal stenosis, or facet joint arthritis.
Accurate information about the procedure is crucial as it ensures precise targeting of affected areas, minimizing risks and optimizing therapeutic outcomes.
This intervention plays a pivotal role in the comprehensive management of cervical spine disorders, providing both diagnostic insight and therapeutic relief for patients experiencing neck and upper extremity pain.
What Is a Cervical Spine Epidural Injection?
A cervical spine epidural injection involves injecting steroids and a local anesthetic into the epidural space in the neck. This medical procedure aims to alleviate pain and reduce inflammation associated with various cervical spine conditions.
Unlike labor epidurals, which are performed in the lower back for childbirth, a cervical epidural is specifically targeted at neck-related pain conditions. The epidural space, a potential area between the dura and spinal ligaments, encompasses fat, veins, arteries, spinal nerve roots, and lymphatics, extending from the base of the skull to the tailbone.
Analogous to inflating a bicycle tire tube, the epidural space fills with medicine when a needle is accurately placed into it, providing therapeutic relief.
Are There Different Types of Cervical Epidural Injections?
There are two different types of cervical epidural injections: interlaminar vs transforaminal. The differences are based on their approach to the cervical spine.
Interlaminar Epidural Injections
An interlaminar epidural is performed on the backside of the spine. Patients are typically lying face down on a procedure table. The injection is best performed with X-ray guidance and contrast.
The lamina is a thin bone on the backside of the vertebrae. It provides important protection to the fragile spinal cord. An interlaminar epidural injection is the injection of medicine into the epidural space by directing a needle between the lamina of two adjacent vertebrae.
Transforaminal Epidural Injections
A transforaminal cervical epidural injection differs significantly from a traditional cervical epidural, as it targets the front portion of the neck. The procedure involves injecting medication into the epidural space and nerve by precisely placing a needle near the specific foramen through which the spinal nerve exits.
Each spinal level has right and left foramen, and for instance, at the C5/6 level, the injection targets the C6 nerve as it exits the foramen, traveling down the neck into the shoulder and upper arm to address pain and inflammation in that specific area.
How Do Cervical Epidural Injections Work?
Cervical epidural steroid injections are recommended when conservative care fails to alleviate symptoms associated with various conditions, such as cervical degenerative disc disease, disc herniation, radiculopathy causing arm pain, cervical headaches, mild cervical stenosis, and scoliosis leading to nerve root irritation.
These injections work by delivering steroids and local anesthetics directly into the epidural space, aiming to reduce inflammation and provide pain relief. While not a first-line treatment, they serve as targeted interventions to manage persistent symptoms that have not responded to initial conservative approaches.
What Is Injected during the Procedure?
During a cervical epidural steroid injection, local anesthetic and steroids are injected into the epidural space. Steroids, such as hydrocortisone, betamethasone, dexamethasone, and methylprednisolone, serve as potent anti-inflammatory agents to reduce pain and swelling.
It’s important to note that while steroids can be effective, they come with significant potential side effects, including cartilage damage, increased infection risk after certain surgeries, delayed healing, compromised glucose balance, and elevated risk of bone fractures.
Awareness of these side effects underscores the importance of careful consideration and informed decision-making when opting for such procedures.
Five Major Reasons for Increased Pain after the Procedure
After a cervical spine epidural injection, patients may experience increased pain due to various factors. Additionally, the dispersion of medication can lead to inflammation, causing transient discomfort. Below are five reasons for pain after the procedure.
1. Nerve Irritation
Improperly performed cervical epidural injections may lead to irritation or injury of spinal nerve roots within the epidural space, resulting in intensified pain. This can manifest as severe lancinating pain radiating down the arm.
2. Vascular Injection
Injection into veins or arteries within the epidural space, though unintended, can pose significant complications, including stroke and increased pain. Radicular artery injection is a documented complication of cervical epidural steroid injections.
3. Severe Underlying Condition
In cases of severe underlying conditions such as advanced cervical degenerative disc disease, extensive cervical disc herniation, or severe cervical stenosis, a single cervical epidural may prove insufficient for pain management.
Providers may recommend a second injection if initial relief is inadequate, acknowledging that not all cervical conditions can be effectively treated with this procedure.
4. Dural Puncture
Incorrectly performed epidurals may puncture the protective dura surrounding the spinal cord, leading to severe positional headaches known as dural leaks. A blood patch, involving another epidural containing blood, aims to patch the hole in the dura and alleviate symptoms.
5. Failed Injection
Some cervical epidural injections are not accurately placed into the epidural space, resulting in trauma to the skin and underlying tissues. This can lead to increased pain as the injected medications fail to reach their intended target. When steroids are mistakenly injected into neck muscles or ligaments, they can cause significant pain and swelling, and weaken ligament strength.
How to Avoid Increased Pain after the Procedure
Pain can be debilitating, keeping us sidelined from our passions. Nobody wants their pain to escalate. Four ways to avoid increased pain after a steroid injection include the following:
Choose Experienced and Board-Certified Physicians
Experience, education, and training are critical when seeking cervical epidural steroid injections. Opt for a board-certified physician specializing exclusively in pain management and advanced pain procedures, avoiding those with diverse practices.
Assess reviews and consult the Department of Regulatory Agencies (DORA) for additional insights into the physician’s credentials and competence.
Correct Diagnosis
Not all neck conditions can be successfully treated with a cervical epidural injection. Neck pain is not a diagnosis but rather a symptom. Ensure that you have the correct diagnosis. Know what is causing your ongoing neck symptoms and whether a cervical epidural steroid injection is appropriate. Ask which type of cervical epidural steroid is best for your condition.
- The importance of X-ray guided injections
The importance of X-ray guided injections, particularly with the use of contrast, cannot be overstated. At the Centeno-Schultz Clinic, where patients often seek second opinions, we have encountered disappointing outcomes from injections performed elsewhere without proper guidance or contrast.
Without contrast, confirming the accurate needle placement and assessing the dispersion of injected medicine becomes impossible. This lack of information hinders a correct diagnosis, leaving patients and their families in search of answers and viable treatment options. To ensure precision and transparency in your medical care, insist on X-ray guided injections with contrast.
Request and retain the images as part of your medical records for comprehensive evaluation and improved diagnostic accuracy.
Proper Guidance
Cervical epidural steroid injections must always be conducted under X-ray guidance to ensure precise needle placement. Accurate positioning is crucial to avoid potential complications such as nerve irritation, dural puncture, vascular injection, and damage to muscles and ligaments.
Blind injections, performed without X-ray guidance, fall below the standard of care and pose risks to patients. Never consent to a cervical epidural injection without the aid of X-ray guidance.
While ultrasound is a powerful tool for tendon, ligament, and peripheral joint injections, it is not suitable for cervical epidural steroids as it cannot confirm the precise needle placement into the epidural space. Insist on the highest standard of care – insist on X-ray guidance for cervical epidural steroid injections.
Use of Contrast
Contrast, a vital component used in X-ray guided injections, serves as a dye that plays a crucial role in enhancing the precision of the procedure. By injecting contrast, the targeted nerves and epidural space are clearly outlined, ensuring that the administered medicine reaches its intended destination.
The absence of contrast during an X-ray guided procedure leaves uncertainties about whether the targeted structures received the injection. In such cases, medication may inadvertently be delivered into the muscle, subcutaneous fat, or ligaments, offering no therapeutic benefits and potentially exacerbating pain after the cervical epidural steroid injection.
A recent study revealed that over 50% of cervical epidural injections performed without X-ray and contrast failed to reach the epidural space, underscoring the significance of contrast for accuracy in targeting and treatment effectiveness.(1)
Ensuring Accuracy for Effective Diagnosis and Treatment
Ensuring accuracy in cervical spine injections is vital for effective diagnosis and treatment.
Accurate needle placement within the epidural space is crucial to target specific pain sources and minimize risks. While these injections help patients avoid surgery, it’s essential to note potential drawbacks, as high-dose steroids in epidurals can cause severe side effects, potentially hindering the body’s natural healing processes.
Centeno-Schultz provides minimally invasive procedures for back and neck pain, utilizing image-guided spinal injections of platelet lysates or bone marrow concentrate, offering regenerative alternatives that prioritize healing over steroid-related concerns.
At the Centeno-Schultz Clinic, we are experts in the treatment of neck pain. If you or your family members suffer from ongoing neck and/or radiating arm pain, please consider an in-office or virtual evaluation. A board-certified, fellowship-trained physician will review your history and imaging and discuss non-surgical treatment options.
Not ready to undergo cervical spine injections to treat your condition? Consult with us to get a second opinion and get a safe and effective treatment option.

Christopher J. Centeno, MD
Christopher J. Centeno, M.D. is an international expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate in orthopedics. He is board-certified in physical medicine and rehabilitation with a subspecialty of pain medicine through The American Board of Physical Medicine and Rehabilitation. Dr. Centeno is one of the few physicians in the world with extensive experience in the culture expansion of and clinical use of adult bone marrow concentrate to treat orthopedic injuries. His clinic incorporates a variety of revolutionary pain management techniques to bring its broad patient base relief and results. Dr. Centeno treats patients from all over the US who…
Read more
John Schultz, MD
John R. Schultz M.D. is a national expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate for orthopedic injuries. He is board certified in Anesthesiology and Pain Medicine and underwent fellowship training in both. Dr. Schultz has extensive experience with same day as well as culture expanded bone marrow concentrate and sees patients at the CSC Broomfield, Colorado Clinic, as well the Regenexx Clinic in Grand Cayman. Dr. Schultz emphasis is on the evaluation and treatment of thoracic and cervical disc, facet, nerve, and ligament injuries including the non-surgical treatment of Craniocervical instability (CCI). Dr. Schultz trained at George Washington School of…
Read more
John Pitts, M.D.
Dr. Pitts is originally from Chicago, IL but is a medical graduate of Vanderbilt School of Medicine in Nashville, TN. After Vanderbilt, he completed a residency in Physical Medicine and Rehabilitation (PM&R) at Emory University in Atlanta, GA. The focus of PM&R is the restoration of function and quality of life. In residency, he gained much experience in musculoskeletal medicine, rehabilitation, spine, and sports medicine along with some regenerative medicine. He also gained significant experience in fluoroscopically guided spinal procedures and peripheral injections. However, Dr. Pitts wanted to broaden his skills and treatment options beyond the current typical standards of care.
Read more
Jason Markle, D.O.
Post-residency, Dr. Markle was selected to the Interventional Orthopedic Fellowship program at the Centeno-Schultz Clinic. During his fellowship, he gained significant experience in the new field of Interventional Orthopedics and regenerative medicine, honing his skills in advanced injection techniques into the spine and joints treating patients with autologous, bone marrow concentrate and platelet solutions. Dr. Markle then accepted a full-time attending physician position at the Centeno-Schultz Clinic, where he both treats patients and trains Interventional Orthopedics fellows. Dr. Markle is an active member of the Interventional Orthopedic Foundation and serves as a course instructor, where he trains physicians from around the world.
Read more
Brandon T. Money, D.O., M.S.
Dr. Money is an Indiana native who now proudly calls Colorado home. He attended medical school at Kansas City University and then returned to Indiana to complete a Physical Medicine and Rehabilitation residency program at Indiana University, where he was trained on non-surgical methods to improve health and function as well as rehabilitative care following trauma, stroke, spinal cord injury, brain injury, etc. Dr. Money has been following the ideology behind Centeno-Schultz Clinic and Regenexx since he was in medical school, as he believed there had to be a better way to care for patients than the status quo. The human body has incredible healing capabilities…
Read moreAm I a Candidate?
To answer this question, fill out the candidate form below to request a new patient evaluation, and a patient advocate will reach out to you to determine your next steps. Your one-hour, in-office or telemedicine evaluation will be with one of the world’s experts in the field of Interventional Orthopedics.