Cervicalgia
Neck pain can come out of nowhere, gradually or rapidly, after any kind of trauma–like a car accident or snowboard fall.
No matter where it came from, once it’s there, it can ruin your life in a hurry. What was once enjoyable now becomes something you avoid because of the consequences that come with it…
If this sounds too familiar, let’s dig into cervicalgia.
What is cervicalgia? What are the causes of cervicalgia? What are the symptoms associated with cervicalgia? How is cervicalgia diagnosed? What are the treatment options for cervicalgia?
What is Cervicalgia aka Neck Pain?
Cervicalgia is a broad medical term that refers to pain or discomfort in the neck area. This condition is usually caused by musculoskeletal problems or abnormalities in the cervical spine (the portion of the spine that runs through the neck). It is a common condition and can range from mild to severe.
Symptoms of cervicalgia can include:
- Pain or stiffness in the neck
- Headaches
- Pain that radiates to the shoulders, arms, or hands
- Tingling or numbness in the arms or hands
- Difficulty turning the head or neck
- Muscle spasms in the neck
Cervicalgia can be caused by a variety of factors, including poor posture, injury, arthritis, and degenerative disc disease. Risk factors for neck pain include prior history of musculoskeletal pain, high quantitative jobs, low social support, job insecurity, low physical strength, and poor computer station design.
Cervicalgia is common and affects approximately two-thirds of the population at some point in their lives. It is the fourth major cause of disability.
Symptoms of This Condition
The cervical spine is complex and composed of 16 facet joints, 6 intervertebral discs, 14 nerve roots, and a network of ligaments and muscles. All or any of these can cause pain that could be under the broad umbrella of cervicalgia.
With that said, this is why there are so many symptoms associated with cervicalgia.
Pain
- Pain in the neck region
- Stiffness and spasm in neck muscle
- Radiating pain throughout the body and arms
- Numbness and tingling in the arms
- Neck soreness
- Difficulties in neck movement
- Neck pain that gets worse if you hold your head in one place
- Shoulder pain
- Thoracic pain
- Pain in the arm, forearm, or hand.
- Electrical shooting pain from the neck into fingers
- Numbness in the hand and fingers
- Weakness in the arm, hand, or fingers
Dizziness & More
- Nausea
- Headache
- Loss of bowel or bladder control
Common Causes of This Condition
There are many different causes of neck pain.
The most common cause of cervicalgia include:
Muscle Injury
Injury to the muscle is also known as strain and typically is the result of overactivity or trauma. It typically improves with conservative care.
One example of muscle injury is when a patient is in a minor car accident and experiences whiplash that strains the muscles and causes pain. The good news is that if only the muscles are injured, then it will likely resolve on its own. If the pain does not resolve, it could be coming from other damaged structures in the neck!
Facet Injury
A facet is a small joint on the backside of the spine that provides stability and limits rotation. It is susceptible to injury. Pain arising from the facet joint has been well studied. Each joint has a distinct referral pattern which is illustrated to the right.
For example injury to the C5/6 facet joint typically results in pain in the shoulder and wing blade area. Injury to the facet joint can cause cervicalgia.
Disc Injury
The disc is an important shock absorber sandwiched between the boney building blocks of the spine. Discs are also susceptible to injury. Common disc injuries include disc protrusion, disc bulges, and disc herniations–all of which can cause cervicalgia.
Understand more about disc and disc injuries in this page.
Spinal Nerve Injury/ Compression
At each level of the spine, a spinal nerve exits the spinal column through a boney doorway. The doorway is called the neural foramen. The existing nerve can be irritated or compressed by disc protrusions, facet overgrowth, thickened ligaments, and bone spurs.
Common symptoms include electrical radiating pain down one or both arms which can extend into the fingers. Numbness and tingling may occur. Spinal nerve irritation is a frequent cause of cervicalgia.
Ligament Injury
Ligaments are thick pieces of connective tissue that connect one bone to another. They provide important stability for the cervical spine. Damage or injury of the ligament can result in excessive movement of the structures in the spine.
This is a very overlooked cause of cervicalgia; many times co-existing with other issues. The best way to diagnose ligamentous injuries is with a digital motion x-ray!
A ligament injury is unstable and can cause additional wear and tear on the discs, facets, and nerves. Ligament injury can cause cervicalgia.
Poor Posture
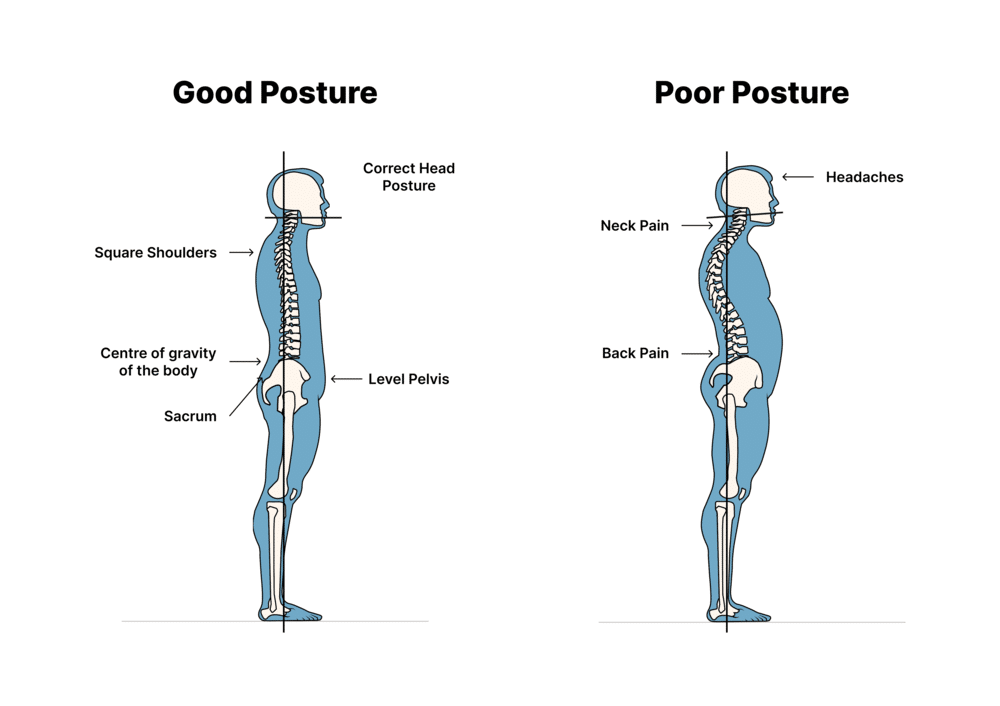
The neck is a series of boney building blocks that stack upon one another. Neutral spinal alignment is essential for the proper function of the muscles, joints, and discs.
Regrettably, computer screens, tablets, and cell phones have compromised this spinal alignment placing excessive demand on the supporting muscles, ligaments, and tendons.
Over time the facet joints and discs become irritated and injured. Neck pain soon develops. Poor posture is a significant cause of cervicalgia.
Stress and Psychological Issues
Stress and psychological issues cause muscle tension in the neck. If persistent, this can change the alignment of the spine resulting in pain and limitation.
Common Treatments for This Condition
Treating cervicalgia is very much dependent on the cause! As we have just highlighted, there are so many causes and multiple things that can be the root cause of your cervicalgia. The first and most important determination to make is to find out what is causing the cervicalgia. Once this has been determined, we can then determine the best treatment options.
This puts a huge emphasis on the initial examination and is why our physicians carve out between 40-60 minutes for our new patient evaluation to give time to find out the causes. Many times, there can be multiple causes but let’s discuss various treatment options:
Conservative
- Rest
- Heat or ice compresses
- Safe anti-inflammatory medications such as fish oil and turmeric
- Stretching
- Good posture with neutral spine alignment: Say goodbye to the rounded shoulders and collapsed chest.
- Chiropractic care
- Physical therapy
- Yoga
Steroids
When conservative therapy fails to provide relief, many patients are referred for steroid injections. Steroids are powerful anti-inflammatory agents that should be avoided as they are toxic to cartilage and other orthopedic tissue. They also have significant side effects including bone death and osteoporosis.(4)
Surgery
Surgery is oftentimes recommended for patients with disc and spinal nerve injuries who do not respond to conservative therapy. There are a number of different surgeries for these conditions.
A common surgical solution is cervical fusion. This is a major surgery where a disc is removed and replaced with bone or a spacer and the spinal bones are stabilized by screws and plates.
Fusion is no guarantee that the pain will improve. There are significant complications associated with fusion which include:
- Infection
- Failure: The bones do not fuse
- Nerve injury
Adjacent Segment Disease: This is a condition where there is additional pressure placed on the disc and facets above and below the level of the fusion. This added pressure leads to degeneration, pain, and oftentimes the need for additional surgery.
To learn more about adjacent segment disease please click on the video below.
Regenerative Options
At the Centeno-Schultz Clinic, we are experts in the diagnosis and treatment of neck pain. We have 15 years of experience treating disc, facet, ligament, spinal nerve, and ligament injuries. Treatment options include PRP and a patient’s own stem cells.
In 2005, we were the first clinic in the world to inject stem cells into the disc. PRP is rich in growth factors that can increase blood flow, decrease inflammation, and accelerate healing. Stem cells are powerhouses of regeneration and repair using different pathways throughout the body to promote healing.
To learn more about the destructive consequences of repeated steroid injections and how PRP can help save your spine from surgery.
Research has grown over the past 15 years, showing superiority of PRP as compared to more traditional non-surgical options (corticosteroids or radio frequency ablations).
Who Is At Risk of Getting This Condition?
There are several risk factors that can increase the likelihood of developing cervicalgia:
- Poor posture: Holding the neck in an awkward position for prolonged periods can strain the muscles and increase the risk of developing neck pain.
- Age: The risk of developing cervicalgia increases with age as the cervical spine undergoes degenerative changes.
- Gender: Women are more likely to develop cervicalgia than men.
- Occupation: Jobs that require prolonged sitting or standing, repetitive neck movements, or heavy lifting can increase the risk of developing neck pain.
- Stress: Emotional stress can cause tension in the neck muscles and contribute to the development of cervicalgia.
- Lack of physical activity: A sedentary lifestyle can weaken the neck muscles and increase the risk of developing neck pain.
- Smoking: Smoking can increase inflammation in the body and reduce blood flow to the cervical spine, which can contribute to the development of cervicalgia.
- Medical conditions: Certain medical conditions, such as fibromyalgia, spinal cord tumors, or infections, can increase the risk of developing cervicalgia.
It’s important to address these risk factors to reduce the risk of developing cervicalgia. Maintaining good posture, engaging in regular physical activity, managing stress, and avoiding smoking are some of the ways to reduce the risk of developing neck pain.
Reducing Risk & Prevention
There are several steps you can take to help prevent cervicalgia, or neck pain:
- Maintain good posture: Sit and stand with your shoulders back and your head level. Avoid hunching over a computer or phone for prolonged periods.
- Take breaks: If you spend long hours sitting or standing, take breaks to stretch and move around every 30-60 minutes.
- Use ergonomic equipment: Make sure your workstation is set up properly with a chair that supports your back and a computer screen at eye level.
- Exercise regularly: Engage in regular physical activity to keep your neck and back muscles strong and flexible. This can include stretching, yoga, or other low-impact exercises.
- Manage stress: Stress can cause tension in the neck muscles, so finding ways to manage stress, such as meditation or deep breathing exercises, can help prevent neck pain.
- Avoid repetitive motions: Repetitive motions, such as typing or using a mouse, can strain the neck muscles over time. Take frequent breaks or switch to different tasks to avoid overuse.
- Avoid carrying heavy loads: Carrying heavy bags or backpacks can strain the neck muscles. Use a backpack with wide straps or a rolling bag instead.
- Quit smoking: Smoking can reduce blood flow to the cervical spine, which can contribute to the development of neck pain.
By taking these steps to prevent cervicalgia, you can reduce your risk of developing neck pain and improve your overall neck health.
Diagnosing Cervicalgia
As seen above, cervicalgia is a generalized diagnosis with multiple causes or pain generators resulting in neck pain. During your evaluation with one of our experts, we will spend the better part of an hour getting to know you and your unique features of your cervicalgia.
Once a thorough history has been taken, then the examination and review of any imaging studies will help narrow down the exact causes. Here is a hint: there is likely more than one cause for your neck pain and this is why your treatment plan will likely include multiple tissue targets.
One example of these causes could be facets, ligaments, and epidural around the discs.They could even include the discs themselves. This approach is what makes us different from most traditional interventional pain doctors.We treat the entire Functional Spinal Unit (FSU).
Treating the functional spinal unit is important because it is the fundamental structural and functional unit of the spine. A functional spinal unit consists of two adjacent vertebrae, the intervertebral disc, and the associated ligaments and muscles.
Each functional spinal unit is responsible for transmitting forces and motion between the vertebrae. The FSU provides stability to the spine, and allows for proper range of motion.
When a functional spinal unit is compromised, it can lead to pain, inflammation, reduced mobility, and other symptoms. This can be caused by a variety of factors, such as injury, degenerative changes, or poor posture.
Treating the functional spinal unit involves addressing the underlying cause of the problem and restoring proper function. This may include physical therapy, chiropractic adjustments, exercises to improve strength and flexibility, medication to reduce inflammation and pain, or in some cases, surgery.
By treating the functional spinal unit, not only can the immediate symptoms be relieved, but the overall health and function of the spine can be improved. This can help prevent future problems and reduce the risk of developing chronic spinal conditions.
Don’t Take Neck Pain Lightly. Get Yourself Checked Now.
Neck pain is a progressive condition that can get worse over time if you don’t take action. Taking pills and hoping that it will go away is not effective. Dependence on medication also poses significant risks which include increasing your risk for heart attack, GI bleed, dependence, and addiction.
Schedule a Telemedicine consultation with a board-certified, fellowship-trained physician and learn about your regenerative treatment options. Act now while the issue is small and treatment is available. Get your life and level of activity back today!

Christopher J. Centeno, MD
Christopher J. Centeno, M.D. is an international expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate in orthopedics. He is board-certified in physical medicine and rehabilitation with a subspecialty of pain medicine through The American Board of Physical Medicine and Rehabilitation. Dr. Centeno is one of the few physicians in the world with extensive experience in the culture expansion of and clinical use of adult bone marrow concentrate to treat orthopedic injuries. His clinic incorporates a variety of revolutionary pain management techniques to bring its broad patient base relief and results. Dr. Centeno treats patients from all over the US who…
Read more
John Schultz, MD
John R. Schultz M.D. is a national expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate for orthopedic injuries. He is board certified in Anesthesiology and Pain Medicine and underwent fellowship training in both. Dr. Schultz has extensive experience with same day as well as culture expanded bone marrow concentrate and sees patients at the CSC Broomfield, Colorado Clinic, as well the Regenexx Clinic in Grand Cayman. Dr. Schultz emphasis is on the evaluation and treatment of thoracic and cervical disc, facet, nerve, and ligament injuries including the non-surgical treatment of Craniocervical instability (CCI). Dr. Schultz trained at George Washington School of…
Read more
John Pitts, M.D.
Dr. Pitts is originally from Chicago, IL but is a medical graduate of Vanderbilt School of Medicine in Nashville, TN. After Vanderbilt, he completed a residency in Physical Medicine and Rehabilitation (PM&R) at Emory University in Atlanta, GA. The focus of PM&R is the restoration of function and quality of life. In residency, he gained much experience in musculoskeletal medicine, rehabilitation, spine, and sports medicine along with some regenerative medicine. He also gained significant experience in fluoroscopically guided spinal procedures and peripheral injections. However, Dr. Pitts wanted to broaden his skills and treatment options beyond the current typical standards of care.
Read more
Jason Markle, D.O.
Post-residency, Dr. Markle was selected to the Interventional Orthopedic Fellowship program at the Centeno-Schultz Clinic. During his fellowship, he gained significant experience in the new field of Interventional Orthopedics and regenerative medicine, honing his skills in advanced injection techniques into the spine and joints treating patients with autologous, bone marrow concentrate and platelet solutions. Dr. Markle then accepted a full-time attending physician position at the Centeno-Schultz Clinic, where he both treats patients and trains Interventional Orthopedics fellows. Dr. Markle is an active member of the Interventional Orthopedic Foundation and serves as a course instructor, where he trains physicians from around the world.
Read more
Brandon T. Money, D.O., M.S.
Dr. Money is an Indiana native who now proudly calls Colorado home. He attended medical school at Kansas City University and then returned to Indiana to complete a Physical Medicine and Rehabilitation residency program at Indiana University, where he was trained on non-surgical methods to improve health and function as well as rehabilitative care following trauma, stroke, spinal cord injury, brain injury, etc. Dr. Money has been following the ideology behind Centeno-Schultz Clinic and Regenexx since he was in medical school, as he believed there had to be a better way to care for patients than the status quo. The human body has incredible healing capabilities…
Read moreAre you a Candidate?
References:
- Lee, J. W., Kim, S. H., Kim, M. Y., & Hwang, C. J. (2018). Intra-articular platelet-rich plasma injections for the treatment of chronic facet joint pain: a randomized, double-blind, controlled clinical trial. Spine, 43(3), 149-156.
- Kim, J. H., Lee, K. J., Kim, H. J., Kim, Y. J., & Cho, H. K. (2018). The efficacy of intra-articular platelet-rich plasma injections for the treatment of lumbar facet joint syndrome. Journal of Back and Musculoskeletal Rehabilitation, 31(3), 387-393.
- Patel, V. B., Thacker, J., Patel, M. B., & Rawal, J. S. (2019). Intra-articular platelet-rich plasma injection for chronic low back pain originating from the facet joints: a randomized, double-blinded, active-control trial. Asian Spine Journal, 13(4), 572-581.
- Murtagh, J. (2016). Managing mechanical back pain. Australian Prescriber, 39(5), 162-166. https://doi.org/10.18773/austprescr.2016.057
- Huang, Q., Cheng, L., Yang, T., & Li, H. (2019). A review on the anatomy and biomechanics of the functional spinal unit. Journal of Healthcare Engineering, 2019, 9732462. https://doi.org/10.1155/2019/9732462
- Panjabi, M. M. (2006). A hypothesis of chronic back pain: Ligament subfailure injuries lead to muscle control dysfunction. European Spine Journal, 15(5), 668-676. https://doi.org/10.1007/s00586-005-0925-3
- Lee, M., Lee, J., Lee, H., Lee, S., Lee, J., Lee, S., & Park, S. (2019). Changes in cervical sagittal alignment parameters and health-related quality of life scores following anterior cervical discectomy and fusion. Clinical Spine Surgery, 32(7), E334-E339. https://doi.org/10.1097/BSD.0000000000000748
- Wu J, Zhou J, Liu C, Zhang J, Xiong W, Lv Y, Liu R, Wang R, Du Z, Zhang G, Liu Q. A Prospective Study Comparing Platelet-Rich Plasma and Local Anesthetic (LA)/Corticosteroid in Intra-Articular Injection for the Treatment of Lumbar Facet Joint Syndrome. Pain Pract. 2017 Sep;17(7):914-924. doi: 10.1111/papr.12544. Epub 2017 Feb 22. PMID: 27989008.
- Kim et al. (2012) conducted a retrospective case series of 26 patients who received PRP injections for lumbar facet joint pain. The study found that the majority of patients reported significant improvement in pain and function scores, and that there were no major adverse events associated with the injections.
- Lee et al. (2018) conducted a randomized controlled trial to evaluate the effectiveness of intra-articular PRP injections in patients with chronic facet joint pain. The study found that the PRP group had significantly greater improvement in pain and function scores than the control group at 6 months after the injection.
- Patel et al. (2019) conducted a randomized, double-blind, placebo-controlled trial to evaluate the efficacy of PRP injections for the treatment of chronic low back pain originating from the facet joints. The study found that the PRP group had significantly greater improvement in pain and function scores than the control group at 12 weeks after the injection.