Shoulder Arthritis
Causes, Symptoms, & Treatment Options for Shoulder Osteoarthritis
Shoulder arthritis is a common musculoskeletal condition. It affects about 32% of the US population above 60 (1). Shoulder arthritis causes progressive and irreversible destruction of the glenohumeral (shoulder) joint.
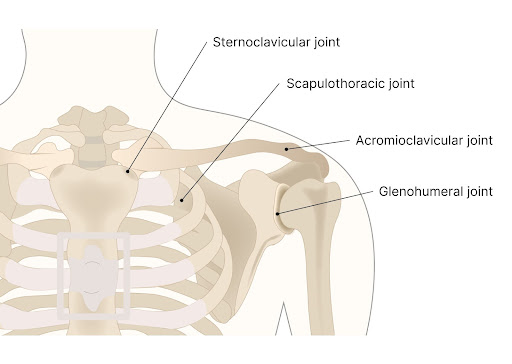
Basic Anatomy of the Shoulder
The shoulder joint is composed of the following parts:
- Bones
There are three major bones in the shoulder. The upper arm bone (humerus), the scapula (shoulder blade), and the clavicle (collarbone). - Joints
There are three joints in the shoulder.
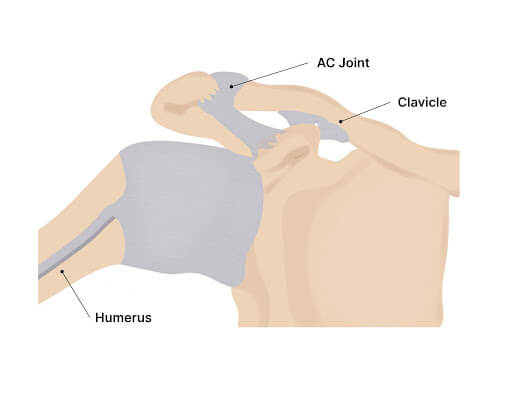
The large ball socket joint (glenohumeral joint) where the rounded portion of the humerus (arm bone) connects with the shoulder socket (glenoid). The sternoclavicular (SC) is where the clavicle connects with the sternum medially. The acromioclavicular (AC) joint is where the clavicle connects with the acromion laterally.
- Muscles
Muscles provide strength, support, and stability for the shoulder joint. The rotator cuff is composed of 4 major muscles: supraspinatus, infraspinatus, teres minor, and subscapularis. - Tendons
Tendons are thick pieces of connective tissue that connect muscle to bone. The rotator cuff tendons are the most important tendons in the shoulder as they provide stability, support, and movement for the shoulder. - Ligaments
Ligaments are thick pieces of connective tissue that connect bone to bone. The superior, middle, and inferior glenohumeral ligaments provide stability for the shoulder. - Cartilage
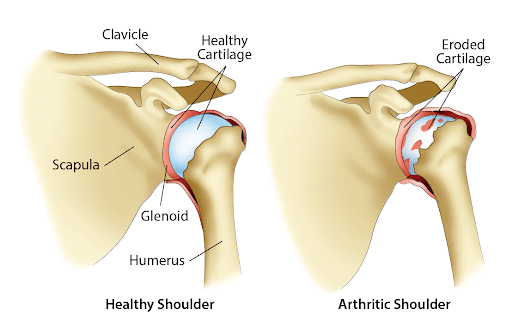
Cartilage is the smooth tissue that covers the ends of the bones. It allows the bones to move smoothly against each other.
Keep reading to learn more about shoulder arthritis and how it is diagnosed and treated.
All three joints in the shoulder, the glenohumeral, sternoclavicular (SC), and acromioclavicular joints can be affected by arthritis. Arthritis can erode or break down the cartilage in the shoulder joints leading to inflammation and stiffness.
What Is Arthritis In The Shoulder?
The shoulder joint is a ball and socket with a wide range of motion. The cartilage in the shoulder can be eroded from wear and tear, aging, inflammation, or antibodies produced in certain autoimmune conditions.
The Types Of Arthritis In The Shoulder
Many types of arthritis affect the shoulder. We discuss them briefly below.
- Rheumatoid Arthritis (RA): Rheumatoid arthritis (RA) is an autoimmune condition characterized by inflammation of the joints. In RA, the immune system mistakenly attacks one’s joints leading to inflammation, swelling, pain, and restriction in range of motion.
It initially affects the smaller joints in the body, but gradually over time, it can start to affect larger joints like the shoulders. Inflammatory cells invade the synovial membrane and cause thickening, leading to joint pain and stiffness. - Osteoarthritis: Osteoarthritis (OA) can affect many joints, including the shoulder joint. Primary OA is the most common type of OA, which occurs in the absence of a predisposing trauma or disease.
Secondary OA occurs with a preexisting joint condition, such as trauma or injury, congenital joint disorders, inflammatory arthritis, avascular necrosis, infectious arthritis, Paget’s disease, osteoporosis, osteochondritis dissecans, metabolic disorders like hemochromatosis, and hemoglobinopathy. - Post-Traumatic Arthritis: Post-traumatic arthritis (PTA) can develop after acute direct trauma to the joints. It is a chronic inflammatory arthritis where inflammation occurs in response to acute trauma.
PTA can persist and damage the rest of the joint, leading to osteoarthritis (2). Post-traumatic arthritis (PTA) accounts for approximately 8-20 % of all osteoarthritis cases (3). - Arthritis Secondary To Avascular Necrosis: Necrosis means cell and tissue death. Avascular necrosis is bone death that occurs when there is a limited blood supply to the head of the humerus.
This can be due to trauma or disease. Without an adequate blood supply, the bone will gradually die, which can lead to arthritis. As the AVN progresses, the joint changes shape from a ball socket joint to a square peg in a round hole.
- Rotator Cuff Tear Arthropathy: Rotator cuff tear arthropathy is a type of arthritis that occurs due to a prolonged tear of the rotator cuff. The tendons of the rotator cuff cover the head of the humerus. If the muscles are torn, the head gets exposed and rubs or grinds against the scapula, which can lead to arthritis.
Symptoms Of Arthritis In The Shoulder
Arthritis in the shoulder can present with different symptoms based on the underlying cause of the arthritis. Here’s a list of symptoms associated with shoulder arthritis:
Pain In The Shoulder Joint
Pain can occur in different shoulder locations, which can indicate which part is affected:
- When the acromioclavicular (AC) joint is affected, the pain is usually experienced at the top of the shoulder.
- Pain surrounding the shoulder can indicate an involvement of the rotator cuff.
- The pain can disrupt joint shoulder movement and affect sleep when the person sleeps on the side of the affected shoulder joint.
More Symptoms You May Experience from Shoulder OA
Left Shoulder Blade Pain
Learn to know the symptoms and causes of shoulder blade pain as well as the diagnostic tests to run for it and its treatment options. Shoulder blade pain can be a common, annoying, hard to diagnose problem. There are many different causes of shoulder blade pain and the exact cause of the shoulder blade pain will determine what type of treatments would be recommended.
Read More About Left Shoulder Blade PainMuscle Spasm In Shoulder
A muscle spasm, also known as a muscle cramp, is a sudden and involuntary contraction or tightening of a muscle or group of muscles. This can occur in any part of the body but is most commonly experienced in the legs, arms, and back. These spasms can last for a few seconds up to many minutes. Occasional muscle spasms may not be something to worry about, but chronic muscle spasms can be a serious issue. In the shoulder, there are many muscles that can go into spasm. These spasms or cramps can cause pain, stiffness, and limited mobility.
Read More About Muscle Spasm In ShoulderPain in Front of Shoulder Joint
Front shoulder pain is a disabling complaint commonly seen in the doctor’s office with a lifetime prevalence of 70%. It is a treatable condition within the shoulder joint. If left untreated, the recovery can be awfully slow with high recurrence rates. There are many causes of pain in front of the shoulder joint. The key is to identify what causes front shoulder pain and diagnose it promptly. The shoulder joint is a ball and socket joint. The rotator cuff muscles stabilize the joint by attaching it to the capsule of the joint. Tendons of other muscles also provide the joint with added stability…
Read More About Pain in Front of Shoulder JointShoulder And Neck Pain On Right Side
Shoulder and neck pain on the right side can indicate conditions involving the organs in the right side of your chest and abdomen. If you have right-sided neck and shoulder pain, it must be investigated. This post delves into the possible symptoms, causes, and treatments for this condition.
Read More About Shoulder And Neck Pain On Right SideShoulder Blade Pain
The upper back or shoulder blade area can be a challenging area to identify what is causing the pain. This area is an overlapping region with multiple possible causes of pain. All of these are on the differential when it comes to pain in the upper back or shoulder blade pain: Thoracic Radiculitis (T1 – T6 nerve roots: 10 different nerves),Thoracic discogenic pain (T1-T6: 5 different discs) Thoracic facet joint syndrome (rib connection to the spine 1-5: 10 different joints), Scapulothoracic bursitis, Cervical radiculitis (C4-T1 nerve roots: 8 different nerves), Cervical facet joint syndrome (C3-T1 facets: 10 different joints), Cervical disc…
Read More About Shoulder Blade PainShoulder Cracking
The Scapula is your shoulder blade. It is a large triangular bone that compromises part of the shoulder joint. The Scapula is positioned over the back chest wall and ribs where it moves in different directions with shoulder movements (1). The Scapula meets with the arm bone (humerus) to form the shoulder joint. It also meets with the clavicle to form the AC joint. Multiple structures attach onto the Scapula which provides important support and movement for the scapulae and shoulder joint (2). These include:- Muscles/Tendons: Multiple muscles attach to the Scapula which include the deltoid, supraspinatus, infraspinatus, triceps, and teres minor.
Read More About Shoulder CrackingShoulder Pain When Reaching Across Body
Shoulder pain can make simple chores almost impossible. Have you ever reached for an object high on a shelf only to have pain that takes your breath away? What causes shoulder pain when reaching across the body? What is shoulder impingement? What does shoulder impingement feel like? Can a shoulder X-ray show shoulder impingement? What are the treatment options for shoulder pain when reaching across the body? ulder impingement and rotator cuff injuries are among the most common causes of shoulder pain (1). Both can cause shoulder pain when reaching across the body. Shoulder impingement is a painful condition in which the bursa and muscles of the shoulder are pinched or compressed.
Read More About Shoulder Pain When Reaching Across BodyShoulder Pain When Sleeping
There are several reasons why shoulder pain at night occurs or is aggravated; The common explanations include: Sleep typically involves a static position lasting hours at a time with little or no movement. Sleeping on your side places additional pressure on the tendons and bursa of the shoulder. Sleep can cause muscles and tendons to settle in a slightly different position resulting in additional pressure and reduced blood flow. Identifying the underlying problem is important! This allows therapy to focus exclusively on the exact problem or problems. When appropriate conservative care is always the first line of treatment. Focus is typically on strengthening and improving range of motion.
Read More About Shoulder Pain When SleepingWhy Does My Shoulder Hurt When I Lift My Arm?
Shoulder pain can be very non-specific, meaning that multiple structures and issues can cause identical pain in the shoulder. Most shoulder examination maneuvers are very limited in their ability to assess exactly what the problem is. With pain when lifting your shoulder, it is critical to take a detailed history, good examination, coupled with imaging to fully understand what is causing the shoulder pain. Many conditions can present with these symptoms
Read More About Why Does My Shoulder Hurt When I Lift My Arm?Risk Factors for Developing Shoulder Arthritis
There are many causes of arthritis in the shoulder joint. They are listed below:
- Excessive Body Weight
Excess body weight can affect the joints in many ways. The weight itself limits the movement of the joints and makes them stiff. Stiff joints may prevent the joint fluid from lubricating the joints. In a typical joint, movement helps lubricate the joint capsule and synovium.
Without this normal movement, the joints have no lubrication and gradually break down due to grinding over dry surfaces.
Higher body weight also means increased amounts of stored fat. Stored fat contributes to an overactive immune system with larger quantities of inflammatory cells and chemicals, such as cytokines and proteins, which can attack the cartilage and the joint. Increased BMI is a risk factor for the development of shoulder arthritis(5). - History Of Trauma Or Shoulder Injuries
A history of previous fractures, dislocations, and trauma can also increase the risk of arthritis. Fibrous tissue may replace the connective tissue when the joint does not heal properly after an injury. As a result, there is a higher chance of developing arthritis.
Trauma and injuries, such as cuts or wounds, can cause bacteria, viruses, or fungi to enter the bloodstream and infect the shoulder joint. These organisms can invade the joint and cause an infection. T blood supply, these microorganisms can invade the joint and cause an infection. This can lead to conditions like arthritis or joint sepsis. - Autoimmune Disorders
Large proximal joints like the shoulder are susceptible to attack by antibodies in autoimmune conditions. These autoimmune disorders, such as rheumatoid arthritis and psoriasis, are conditions where the body produces inflammatory substances that gradually destroy the bone.
There is often a familial or genetic predisposition to these conditions. - Age
The risk of developing shoulder arthritis increases with age (8). - Tobacco Use
Smoking is a risk factor for the development of shoulder arthritis. - History of Ligament Laxity or Dislocations
Ligaments provide important stability for the shoulder. Injury to the ligaments can lead to shoulder instability which in turn can erode the joint cartilage leading to shoulder arthritis (7). - Genetics
Unfortunately, some of us carry that old family gene that predisposes us to degenerative conditions such as shoulder arthritis. - Excessive Mechanical Loading
Powerlifting, training with heavy weights, and repetitive shoulder motions required by some professions can lead to shoulder arthritis. - Shoulder Instability
Stability of the shoulder joint is imperative for optimal joint health and function. Shoulder instability due to ligament laxity or rotator cuff injuries can lead to shoulder instability. In such cases, there is excessive motion of the arm bone (humerus) in relation to the socket leading to damage to the cartilage. - Inflammatory Arthritis
Inflammatory arthritis is a group of diseases caused by an overactive immune system. This is also called an autoimmune disorder in which the body attacks it own healthy cells. Examples include rheumatoid arthritis (RA), psoriatic arthritis, juvenile idiopathic and ankylosing spondylitis (AS), and gout.
Common Treatments For Arthritis In The Shoulder
There are different treatment options for arthritis in the shoulder. The treatment depends on what is causing arthritis and the severity of the condition. The following are some common treatments that can help improve the symptoms of shoulder arthritis:
Natural Treatments
These are those that don’t require equipment or medications. Some natural treatments for shoulder arthritis are listed below:
- Activity Modification
Certain activities may aggravate arthritic symptoms, such as exercise or repetitive shoulder movements. Avoiding painful movements and choosing joint-friendly activities can help reduce inflammation and symptoms like pain and stiffness.
For example, walking or cycling are alternative forms of exercise to other activities like tennis. - Range Of Motion Exercises
Range of motion exercises can improve the flexibility of the shoulder joint. These exercises promote gentle movement in the joint within a comfortable range.
After some time, as the pain decreases, exercises can also strengthen the joint. Muscle strength is an important component to shoulder stability. These exercises may include shoulder, pectoral, and biceps stretches and scapular range of motion exercises. - Heat Therapy
Studies have shown that applying heat and moisture during stretching exercises can improve the extensibility of the muscles in the shoulder (3).
This is because it increases blood supply to the muscles and relaxes them. This can include hot water bottles, steam towels, moist heating packs, or even a hot shower. - Ice Therapy
Cold therapies are recommended for arthritis. For pain relief, icing your shoulder for 10-minute intervals can help alleviate the pain as the cold constricts the blood vessels.
A combination of ice and heat therapy may be beneficial for shoulder arthritis. Each person must find what works for them regarding arthritis and shoulder pain. - Physical Therapy
Physical therapy can improve range of motion, muscle strengthening, and improved posture and body mechanics. - Chiropractic Care
Chiropractic care can provide spinal adjustments, mobilization of the joint and restoration of soft tissue injuries that are compromising shoulder joint health and function.
Non-Surgical Options
Non-surgical treatment options for shoulder arthritis include medical solutions that require a doctor or therapist. They are listed below:
- Dietary Supplements
Studies have shown that seven dietary supplements can help reduce pain from arthritis, namely collagen hydrolysate, passion fruit peel extract, Curcuma longa extract, Boswellia serrata extract, curcumin, pycnogenol, and L-carnitine (4).
Studies have shown that these supplements have a significant clinical effect on arthritic pain in the short term. However, no supplements have been shown to reduce pain in the long term. - NSAID
NSAIDs are powerful anti-inflammatory agents. Common examples include ibuprofen, naproxen, Voltaren, and Celebrex. They are available in both tablets and topical creams. They have significant side effects which have been previously discussed and should be avoided. - Oral Narcotics
Narcotics are powerful medications to reduce pain and increase function. They have significant side effects which include dependence and therefore should be avoided. Furthermore, they do NOT address the underlying arthritis. Rather, they simply mask the pain. - Corticosteroids
Corticosteroids are a type of medication that reduces inflammation and immune responses. They do so by inhibiting transcription factors that control the synthesis of pro-inflammatory mediators such as macrophages, eosinophils, lymphocytes, mast cells, and dendritic cells.
They also inhibit phospholipase A2, which produces numerous inflammatory mediators. They are prescribed for arthritis to reduce local inflammation and prevent further bone destruction. Corticosteroids can be taken orally or injected directly into the joint.
However, as corticosteroids reduce the density of the bone when taken for extended periods, they are not a permanent treatment option.
Surgical Procedures
Many doctors recommend surgery for shoulder arthritis, especially if conservative options have not been effective.
- Arthroscopic Surgery: Arthroscopic surgery is a type of surgery where a small camera is introduced through the skin to visualize the structures inside the shoulder joint. For shoulder arthritis caused by tendonitis or tears, the repair can be done arthroscopically.
For shoulder nerve compression, loose bodies are present in the joint, or for a torn labrum, arthroscopic procedures may also be recommended over open surgery.
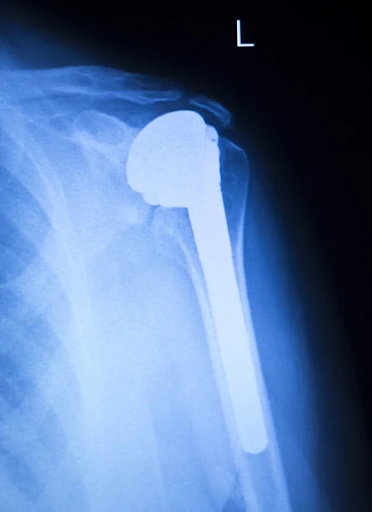
Additionally, in older patients who have shoulder arthritis due to rotator cuff damage, arthroscopic rotator cuff debridement or removal of the synovium is preferred. - Hemiarthroplasty: A hemiarthroplasty is a partial replacement of the shoulder joint. The damaged humeral head is replaced with a prosthetic humeral head. It is usually done in people with osteoarthritis, avascular necrosis, or multiple fractures, particularly when the proximal humerus is involved.
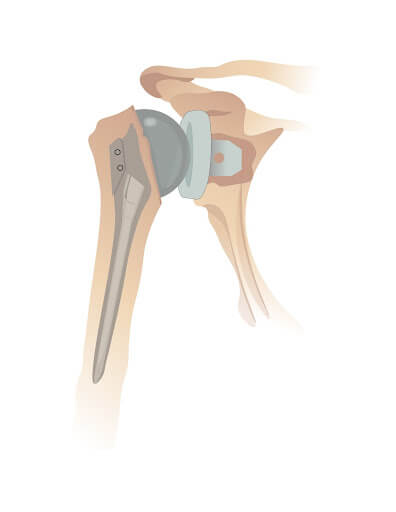
- Shoulder Joint Replacement (Arthroplasty): This is a total shoulder joint replacement. It is the preferred surgery for rheumatoid and other types of inflammatory arthritis. In this procedure, the arthritic ball and socket shoulder joint are replaced with a metal prosthetic joint.
This metallic ball is fixed to the humerus by a stem that fits inside the humerus. This stem anchors the joint and helps articulate the new metallic ball and socket joint. This success of the procedure depends on the integrity of the rotator cuff tendons. If the patient has poor tendon health, they may not be suitable for this procedure.
- Reverse Total Shoulder Arthroplasty: Reverse shoulder arthroplasty is another type of shoulder arthroplasty. The surgeon reconstructs the shoulder joint by reversing the ball and socket mechanism in this procedure.
They use a convex glenoid hemispheric ball to replace the socket part of the shoulder joint and a concave humerus articulating cup to return the ball part of the joint. The procedure can help alleviate pain and improve movement in the joint. - Resection Arthroplasty: This procedure reverses previous reconstructive procedures. In this surgery, the old prosthetic or implant is removed. This is usually done if there is an infection or the shoulder arthroplasty fails.
When Should You Consult Your Doctor?
While arthritis is a condition that is manageable with conservative care, some symptoms should prompt you to seek medical attention.
- A red or inflamed shoulder joint
- The shoulder joint is hot or tender to touch
- Severe pain on joint movement
- Presence of fever
- Inability to elevate the arm
- Severe restriction of motion
- Pain and stiffness
- Crepitus in the shoulder joint
- An injury preceding the shoulder joint pain
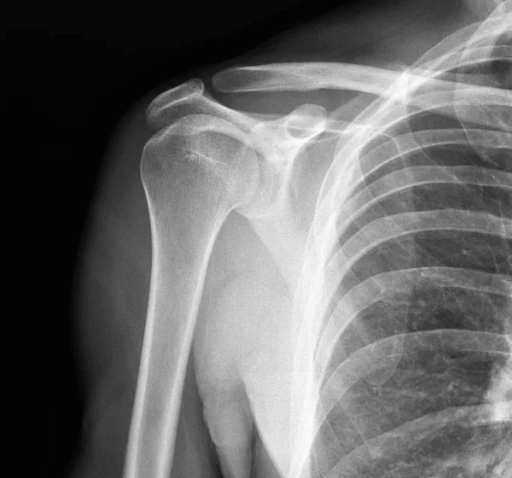
Diagnosis Of Arthritis In The Shoulder
Arthritis in the shoulder is diagnosed with the following methods:
- Medical History: A medical history is significant to identify if you have arthritis and what kind of arthritis it is. The doctor will ask you about the joint, any history of trauma, your occupation, the presence of pain, any associated symptoms, and the relieving and exacerbating factors.
They will also want to know if there is a family history of arthritis, as certain types of inflammatory arthritis tend to have a genetic predisposition. - Physical Examination: The physical exam involves checking all the joints and the range of motion. Since arthritis can affect multiple joints, it is common for various large joints to be involved. In some types of autoimmune arthritis, the diagnosis is based on how many joints are involved.
- Pain Evaluation: The doctor will also test the muscles to determine which movements elicit pain and evaluate the strength of the muscles. Weak muscles may indicate irritation or compression of one or more nerves in the neck.
- Lab Tests: Blood tests are done to rule out an infection, such as a complete blood count. Other blood tests like RA (rheumatoid arthritis) factors, a metabolic panel, and an Antinuclear Antibody Test (ANA) are ordered to diagnose autoimmune arthritis.
- X-Rays: X-rays are the initial imaging modality used to rule out fractures or dislocations. X-rays can identify soft tissue inflammation and joint surface changes but cannot identify any tears in the cartilage or muscles around the joint.
- Ultrasound: The use of ultrasound to diagnose arthritis is steadily increasing. Ultrasound is available as an in-office procedure and can be an efficient and cost-effective alternative to MRIs.
At the Centeno-Schultz Clinic, an ultrasound evaluation is part of every new patient evaluation. Ultrasound can detect subclinical and early inflammation, joint swelling, irritation of bursa, rotator cuff tendinosis, rotator cuff tears, and joint instability.
It is also cheaper than other modalities, so it can be used to monitor remission following physical therapy or surgery. - CT Scan: CT scans are used to detect arthritic changes, especially to identify bony deformities, subchondral cysts, or loss of cartilage. They can also accurately predict prosthetic sizes for shoulder replacement surgery if needed.
- MRI Scan: An MRI can detect certain features of arthritis within the synovium, subchondral bone marrow, and articular fat. These cannot be visualized with other imaging modalities, such as CT or X-ray.
When Shoulder Replacement Surgery Becomes A Good Option
When is shoulder replacement surgery a good option? Shoulder replacement surgery may be considered in the following situations:
- When the shoulder arthritis causes chronic pain
- When there is a loss of function in the joint
- When conservative and medical treatments have failed
- When the pain disrupts sleep at night
- When the pain affects daily activities
Recovery And Rehabilitation After Shoulder Surgery
The recovery time after shoulder surgery depends on the type of surgery performed and the extent of arthritis. The shoulder joint can take six months to two years to become fully functional.
However, it is important to remember recovery always includes pain management, a rehabilitation program, and physical therapy. In general, recovery depends on two main factors:
- Pain Management: Pain after shoulder surgery can be almost as severe as arthritis. Doctors can use a combination of painkillers, including acetaminophen, NSAIDs, tramadol, and gabapentinoids, to help ease the pain.
- Physical Therapy: The type of surgery used can dictate rehab protocol for the shoulder. In general, rehabilitation starts with an eight-week program, with a sling to be used in the first week.
Cryotherapy (cold therapy) can be used to control pain and edema. Range-of-motion exercises usually begin by week three, with a progressive increase in strength training as the weeks go by.
Endurance and strength training usually begin by week eight. The rest of the recovery period depends on the patient’s general health and age.
Can Shoulder Arthritis Heal Without Surgery?
Arthritis can be treated without surgery, especially if the joint damage is not severe. Alternative treatment options include PRP and stem cell injections.
At our Centeno-Schultz Center, shoulder pain caused by shoulder arthritis is treated with precise image-guided stem cell injections. The stem cells are derived from the patient’s body, so the body responds well, reducing the risk of a reaction or rejection.
Regenerative Treatment Options for Shoulder Arthritis
The physicians at the Centeno-Schultz Clinic are experts in the evaluation and treatment of shoulder injuries and arthritis. We offer a comprehensive approach that is referred to as the SANS approach.
It stands for Stability, Articulation, Neurologic, and Symmetry.
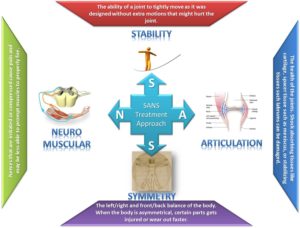
Stability is a very important, often overlooked issue that when compromised can lead to popping and cracking of the shoulder in addition to injury to the rotator cuff tendons and cartilage.
The shoulder is a shallow ball socket joint. It is held in position by the supporting ligaments and muscles. In some cases through trauma or loose ligaments, the ball portion of the shoulder can be dislocated or pulled out of the socket. Why is this important? Once dislocated, the shoulder capsule can become stretched out or loose predisposing the shoulder to chronic instability. This is illustrated below.
Normal shoulder movement is illustrated on the left. Shoulder instability is illustrated on the right. Note there is an excessive movement within the shallow shoulder socket that allows the ball portion of the joint to strike and injure the little gray triangle which is the labrum. Shoulder instability can lead to labrum injury and shoulder osteoarthritis.
Neurologic issues are also important but often overlooked. At the Centeno-Schultz Clinic, we always evaluate the patient as a whole as opposed to focusing only on the shoulder. The cervical spine is included in the examination as many cases of “shoulder pain” are actually pain being referred from an irritated or injured cervical facet or disc.
Treatment options vary depending on the specific injury, its severity, and presenting symptoms. Treatment options include PRP and bone marrow concentrate which is rich in stem cells. Both are powerhouses of healing.
The injections are demanding and require a thorough understanding of the shoulder anatomy. All injections are performed under ultrasound or x-ray guidance, or both. These injections can not be performed by your PCP or orthopedic surgeon. To watch one of my ultrasound-guided shoulder injections please click on the video below.
Relieve Shoulder Pain With The Right Treatment Option
Arthritis is a chronic condition that can be managed well with the right treatment. If you have shoulder arthritis, there are non-surgical and surgical treatment options.
At CSC, we have a holistic approach to treating shoulder arthritis and avoiding unnecessary surgery. If you have shoulder arthritis, talk to one of our board-certified, fellowship-trained doctors today.
Are you a Candidate?

Christopher J. Centeno, MD
Christopher J. Centeno, M.D. is an international expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate in orthopedics. He is board-certified in physical medicine and rehabilitation with a subspecialty of pain medicine through The American Board of Physical Medicine and Rehabilitation. Dr. Centeno is one of the few physicians in the world with extensive experience in the culture expansion of and clinical use of adult bone marrow concentrate to treat orthopedic injuries. His clinic incorporates a variety of revolutionary pain management techniques to bring its broad patient base relief and results. Dr. Centeno treats patients from all over the US who…
Read more
John Schultz, MD
John R. Schultz M.D. is a national expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate for orthopedic injuries. He is board certified in Anesthesiology and Pain Medicine and underwent fellowship training in both. Dr. Schultz has extensive experience with same day as well as culture expanded bone marrow concentrate and sees patients at the CSC Broomfield, Colorado Clinic, as well the Regenexx Clinic in Grand Cayman. Dr. Schultz emphasis is on the evaluation and treatment of thoracic and cervical disc, facet, nerve, and ligament injuries including the non-surgical treatment of Craniocervical instability (CCI). Dr. Schultz trained at George Washington School of…
Read more
John Pitts, M.D.
Dr. Pitts is originally from Chicago, IL but is a medical graduate of Vanderbilt School of Medicine in Nashville, TN. After Vanderbilt, he completed a residency in Physical Medicine and Rehabilitation (PM&R) at Emory University in Atlanta, GA. The focus of PM&R is the restoration of function and quality of life. In residency, he gained much experience in musculoskeletal medicine, rehabilitation, spine, and sports medicine along with some regenerative medicine. He also gained significant experience in fluoroscopically guided spinal procedures and peripheral injections. However, Dr. Pitts wanted to broaden his skills and treatment options beyond the current typical standards of care.
Read more
Jason Markle, D.O.
Post-residency, Dr. Markle was selected to the Interventional Orthopedic Fellowship program at the Centeno-Schultz Clinic. During his fellowship, he gained significant experience in the new field of Interventional Orthopedics and regenerative medicine, honing his skills in advanced injection techniques into the spine and joints treating patients with autologous, bone marrow concentrate and platelet solutions. Dr. Markle then accepted a full-time attending physician position at the Centeno-Schultz Clinic, where he both treats patients and trains Interventional Orthopedics fellows. Dr. Markle is an active member of the Interventional Orthopedic Foundation and serves as a course instructor, where he trains physicians from around the world.
Read more
Brandon T. Money, D.O., M.S.
Dr. Money is an Indiana native who now proudly calls Colorado home. He attended medical school at Kansas City University and then returned to Indiana to complete a Physical Medicine and Rehabilitation residency program at Indiana University, where he was trained on non-surgical methods to improve health and function as well as rehabilitative care following trauma, stroke, spinal cord injury, brain injury, etc. Dr. Money has been following the ideology behind Centeno-Schultz Clinic and Regenexx since he was in medical school, as he believed there had to be a better way to care for patients than the status quo. The human body has incredible healing capabilities…
Read moreOther Resources for Shoulder Arthritis
-
Craniocervical Instability and Vagus Nerve Compression
Craniocervical instability (CCI) occurs when the supportive muscles and ligaments in the upper cervical spine become ‘loose’ or ‘lax’. The importance and complexity of the vagus nerve is highlighted in its name. Vagus is the Latin word for ‘wandering’ and, as the name suggests, the vagus nerve travels widely throughout the body, resembling the root…
-
Why Does My Neck Hurt?
Neck pain can result from various factors, including poor posture, muscle strain, injury, or underlying medical conditions. It can be treated effectively when diagnosed properly. Treatment options may include physical therapy, pain management, exercise, and lifestyle changes to address the root causes of the pain and significantly improve your comfort and quality of life. If…
-
Can Neck Pain Cause Dizziness?
Neck pain and dizziness can be caused by various underlying factors, and their combination may indicate different medical conditions. Here’s a brief overview of the potential causes of neck pain and dizziness. Accompanying Symptoms Experiencing neck pain and dizziness, especially when they occur together, can be quite distressing and impact various aspects of a person’s…
-
Neck Pain Causes
Neck pain is a common musculoskeletal complaint. Over twenty-five million Americans are absent from work for eleven days on average due to neck pain (1). Neck pain has many causes and is often considered multifactorial. As a result, it is especially important to diagnose the cause of the neck pain so that it can be…
-
KT Tape For Hamstring Tendonitis
Hamstring tendinosis is a condition that causes pain and inflammation in the hamstring tendons. The hamstring tendons are the tough bands of tissue that attach the hamstring muscles to the bones in the back of the thigh. Hamstring tendinosis is a degenerative condition, meaning that it is a condition that causes the tissue to break…
-
Cervical Anterior Longitudinal Ligament (ALL) Injuries – What to Know
Is chronic neck pain keeping you from enjoying daily life and activities? Neck feeling stiff, and hurting with computer work turning in the car, playing with your children? Have you been told your neck imaging is fine, you just have a whiplash injury and should be fine, but you know you are not? Sick of…
References:
- Chillemi C, Franceschini V. Shoulder osteoarthritis. Arthritis. 2013;2013:370231. doi:10.1155/2013/370231
- Punzi L, Galozzi P, Luisetto R, et al. Post-traumatic arthritis: overview on pathogenic mechanisms and role of inflammation. RMD Open. 2016;2(2):e000279. Published 2016 Sep 6. doi:10.1136/rmdopen-2016-000279.
- Thomas AC, Hubbard-Turner T, Wikstrom EA, Palmieri-Smith RM. Epidemiology of Posttraumatic Osteoarthritis. J Athl Train. 2017 Jun 2;52(6):491-496. doi: 10.4085/1062-6050-51.5.08. Epub 2016 May 4. PMID: 27145096; PMCID: PMC5488839.
- Liu X, Machado GC, Eyles JP, Ravi V, Hunter DJ. Dietary supplements for treating osteoarthritis: a systematic review and meta-analysis. Br J Sports Med. 2018;52(3):167-175. doi:10.1136/bjsports-2016-097333.
- Rechardt M, Shiri R, Karppinen J, Jula A, Heliövaara M, Viikari-Juntura E. Lifestyle and metabolic factors in relation to shoulder pain and rotator cuff tendinitis: a population-based study. BMC Musculoskelet Disord. 2010 Jul 20;11:165. doi: 10.1186/1471-2474-11-165. PMID: 20646281; PMCID: PMC3161397.
- Kruckeberg BM, Leland DP, Bernard CD, Krych AJ, Dahm DL, Sanchez-Sotelo J, Camp CL. Incidence of and Risk Factors for Glenohumeral Osteoarthritis After Anterior Shoulder Instability: A US Population-Based Study With Average 15-Year Follow-up. Orthop J Sports Med. 2020 Nov 11;8(11):2325967120962515. doi: 10.1177/2325967120962515. PMID: 33241059; PMCID: PMC7675883.
- Cameron ML, Kocher MS, Briggs KK, Horan MP, Hawkins RJ. The prevalence of glenohumeral osteoarthrosis in unstable shoulders. Am J Sports Med. 2003 Jan-Feb;31(1):53-5. doi: 10.1177/03635465030310012001. PMID: 12531757.
- Chan HBY, Pua PY, How CH. Physical therapy in the management of frozen shoulder. Singapore Med J. 2017 Dec;58(12):685-689. doi: 10.11622/smedj.2017107. PMID: 29242941; PMCID: PMC5917053.