Guyon’s Canal
Growing up in South Florida, I never knew what it was like to have different seasons – we basically had hot, hotter, and blistering hot! But now, being in Colorado for many years, I understand the transitions from winter to spring. It means that it’s time to put away my snowboard, dust off the golf clubs, and grease up the mountain bike!
For many of our patients who have a passion for cycling, it also means that the Triple Bypass is right around the corner and it’s time to bump up the training! I had never known about this race until I moved to Colorado. For those who don’t know it, The Triple Bypass is an epic 100+ mile race through the heart of the Colorado Rockies from EVERGREEN TO VAIL, COLORADO!
Today, we are going to discuss a syndrome with which many long-distance cyclists are diagnosed, as well as its preventative measures and treatment options. The condition is Guyon’s Canal Syndrome, also known as Cyclist Palsy.
What Is Guyon’s Canal Syndrome?
Guyon canal syndrome is a condition caused by the compression of the ulnar nerve as it passes through the Guyon canal, a narrow passageway located on the palm side of the wrist.
This syndrome is commonly seen in people who perform repetitive tasks with their hands or use tools that vibrate, such as jackhammers or drills. Other causes of Guyon canal syndrome may include trauma or injury to the wrist, arthritis, or tumors. Treatment for Guyon canal syndrome may include immobilization of the wrist, anti-inflammatory medications, physical therapy, or– in severe cases– surgery.
If left untreated, Guyon canal syndrome can lead to permanent nerve damage, muscle weakness, and loss of function in the affected hand and wrist.
Symptoms of Guyon’s Canal Syndrome
The most common symptoms are:
- Numbness or tingling in the ring and little fingers, which may be intermittent or constant.
- Weakness in the hand and wrist, which may make it difficult to grip objects or perform fine motor tasks.
- Pain in the wrist and hand, which may be sharp or dull and may worsen with certain activities.
- Loss of coordination and dexterity in the hand and fingers, which may make it difficult to perform tasks such as writing or typing.
- Swelling and tenderness in the wrist, which may be accompanied by a tingling or burning sensation.
- Muscle wasting in the hand and wrist, which may occur in advanced cases of Guyon canal syndrome.
Common Causes Of Guyon’s Canal
With any nerve issues – the key to treating successfully is to identify where along the course of the nerve the compression or injury is! Guyon’s Canal Syndrome can have symptoms of progressive impairment of the ulnar nerve functioning, secondary to chronic, mechanical compression of the nerve within the canal of Guyon.
Depending on the location of the lesion within Guyon’s canal, the symptoms may appear in different forms. Often, it can be misdiagnosed as “Cubital Tunnel Syndrome”, which is compression of the ulnar nerve at the elbow which can also give many of the same symptoms!
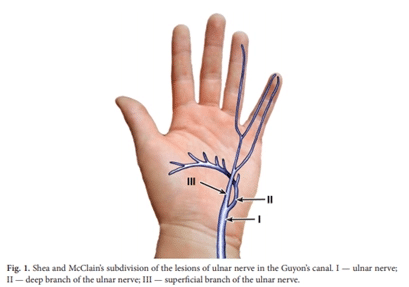
They are similar to the symptoms of the groove for the ulnar nerve, except for the sensory innervation of the dorsum of the hand. This feature is associated with the origin of ramus dorsalis manus, about 5–8 cm proximal from Guyon’s canal. Traditionally the lesions seen in the syndrome of Guyon’s canal are divided following the subdivision proposed by Shea and McClain (Fig. 1).
Chronic Or Repetitive Motion / Trauma
Repetitive hand and wrist movements: Performing repetitive motions with the hand and wrist, such as typing, using power tools, or playing a musical instrument, can increase the risk of developing Guyon canal syndrome.
Handlebar Palsy/Cyclist Palsy, vibration — hypothenar hammer syndrome — industrial workers, sportsmen: handball, basketball, tennis, squash, golf, martial arts, break-dancers.
Hand or wrist trauma: Injuries to the hand or wrist, such as fractures, dislocations, or sprains, can damage the ulnar nerve and increase the risk of developing Guyon canal syndrome.
Diseases Of Neighboring Vessels
Aneurysmatic dilatation of the ulnar artery, arterio-venous malformations, hemangiomas, thrombosis of the ulnar artery, giant cell arteritis.
Metabolic Diseases
People with diabetes may be more susceptible to nerve damage, including damage to the ulnar nerve, which can increase the risk of developing Guyon canal syndrome.
Obesity can increase pressure on the wrist and hand, which can compress the ulnar nerve and increase the risk of developing Guyon canal syndrome.
Other metabolic diseases include rheumatoid polyarthritis, amyloidosis, sarcoidosis, and sclerodermia.
Anatomical Variations
Anatomical abnormalities: Some people may be born with anatomical abnormalities that can put pressure on the ulnar nerve, increasing the risk of developing Guyon canal syndrome. Additional carpal muscles or bones, the presence of piso-hamate arch, fibrosis, a protruding or bifid hook of hamate bone.
Degenerative Diseases In The Wrist
Arthritis can cause inflammation and swelling in the wrist and hand, which can compress the ulnar nerve and increase the risk of developing Guyon canal syndrome. Arthritis creates bone spur/arthritis compressing nerve in Guyon’s canal.
Idiopathic Causatives
Some cases, we just don’t know why. No event / trauma / metabolic condition or repetitive use injuries to point to. This is known as “idiopathic” which is fancy doctor talk for: we just don’t know why.
Tumors
Rarely, tumors in the wrist or hand can put pressure on the ulnar nerve and increase the risk of developing Guyon canal syndrome. Other tumors, like ganglion, lipoma, lipo-fibroma, giant cell tumor, schwannoma, neuroma, osteoid osteoma [7–12] can also cause Guyon’s Canal Syndrome.
Who Is At Risk For Getting Guyon Canal?
Road Bike versus Mountain Biker……Sprint Race versus Endurance Racer….. who is more likely to get Cyclist Palsy?
A prospective study by Patterson et al in 2003, investigated the incidence of ulnar neuropathy in cyclists. The authors investigated 25 cyclists (ages 20–60 years old) randomly chosen for the study, who underwent a 600km bicycle tour over the course of four days.
Using a questionnaire and physical examination, ulnar and median nerve function were assessed on day 0 (the day before the ride began) and then re-evaluated on day 4 (within hours of completion of the ride).
70% of the participants experienced some form of neurological symptoms by the end of the ride! Motor weakness was experienced by 36%. Sensory loss was apparent in 10%. 25% experienced both motor and sensory deficit.
No difference between experienced riders compared to inexperienced riders regarding symptoms. Mountain bikers (9 out of 25) had more sensory loss when compared to individuals who were using road bikes (16 out of 25).
Preventative Measures Against Cyclist Palsy
Prevention of ulnar neuropathy and treatment of early symptoms include:
- Proper bike fitting
- Avoidance of excessive or prolonged weight-bearing through the hands
- Use of padded gloves
- Switching hand positions often on longer rides

Diagnosing Cyclist Palsy
In the clinic, the advancement of technology now allows us to diagnose compressive neuropathies with 98% accuracy based on a detailed physician examination and diagnostic ultrasound imaging.
Several studies have demonstrated that utilizing diagnostic ultrasound to visualize the nerve combined with dynamic test and examination was sensitive >98%.
The ultrasound features of peripheral nerve defects that were the most important are:
- Diameter or cross-sectional area of the nerve at the site of the visualized pathology
- Nerve echostructure, hyperemia
- Presence of instability in a dynamic US examination
- Pain reaction to nerve compression with the transducer
Common Treatments For Guyon’s Canal Syndrome
The treatment of Guyon canal syndrome depends on the severity of the condition and may include one or a combination of the following options:
Conservative Care
Rest and immobilization: Resting the affected hand and wrist and avoiding activities that aggravate symptoms can help reduce pressure on the ulnar nerve. Immobilizing the wrist with a splint or brace can also help alleviate symptoms.
Anti-inflammatory medications: Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, may be recommended to reduce inflammation and relieve pain.
Lifestyle modifications: Making lifestyle modifications, such as avoiding repetitive activities, maintaining good posture, and using ergonomic tools, can help prevent the development or recurrence of Guyon canal syndrome.
Steroid Injections
Corticosteroid injections: Corticosteroid injections into the wrist can help reduce inflammation and alleviate symptoms. BUT these injections come with higher than acceptable risks – corticosteroids can be toxic for nerves and soft tissue, causing further injuries. To learn more about these risks, visit this page: What If The Cortisone Shot Doesn’t Work?
Guyon’s Canal Release
In severe cases of Guyon canal syndrome, surgery may be necessary to relieve pressure on the ulnar nerve. The type of surgery will depend on the location and severity of the nerve compression.
Physical Therapy
Physical therapy can help improve hand and wrist strength and flexibility and may also include exercises to reduce pressure on the ulnar nerve. Utilizing techniques such as “neural flossing” to allow for mobilization of the nerve across the compressive region.
Massage Therapy
Similar to PT options, massage therapy can help mobilize the nerve and calm down nerve irritation.
Utilization Of Brace Or Splints
Immobilization can assist in resting the nerve and taking the repetitive nerve compression.
Nerve Hydrodissection
Nerve Hydrodissection is a medical procedure that aims to free up scar tissue or adhesions on a given peripheral nerve. The procedure utilizes ultrasound guidance to visualize both the needle and the targeted nerve. Medication is then injected through the needle to free up the scar tissue. Nerve Hydrodissection is a minimally invasive treatment option for many peripheral nerves that are compressed or entrapped by scar tissue.Pain is an uncomfortable and at times painful sensation. It varies significantly from patient to patient. There are many different types of pain which include inflammatory, nociceptive, and neuropathic. Neuropathic pain is pain that arises from nerve compression or injury.
Read More About Nerve HydrodissectionNeuro-Prolotherapy (Neural-Prolo)
Neural-Prolo, is also known as Neurofascial Prolotherapy (NPT). Born from traditional prolo-therapy, Neural-Prolo is described as: Subcutaneous peri-neural injection of 5% dextrose. It was created by a New Zealand physician, Dr. John Lyftogt while he was treating a series of Achilles tendon injuries. Similar to how traditional prolotherapy helps strengthen loose ligaments and damaged tendons, Dr. Lyftogt discovered that a low concentration of dextrose (5%) in the subcutaneous tissue can help in resolving chronic nerve inflammation and restoring the normal physiology of the nerve cell. Neuritis is also thought to be a contributing factor to chronic pain syndromes and why sometimes the pain continues…
Read More About Neuro-Prolotherapy (Neural-Prolo)Prolotherapy Injections
It has been successful in the treatment of many disorders including neck, shoulder, knee, and ankle pain. Dr. Centeno recently published an article in The Journal of Prolotherapy in which he discusses the use of x-ray guidance with prolotherapy. This ensures that the injection is in the correct place to maximize clinical results. Dr. Centeno discusses the use of prolotherapy for the treatment of neck, knee, sacroiliac joint, ankle, ischial tuberosity, and shoulder pain. At the Centeno-Schultz Clinic x-ray guided prolotherapy is just one of the therapies utilized in the successful treatment of pain. Regenerative injection therapy (RIT) or prolotherapy…
Read More About Prolotherapy InjectionsPRP for Nerve Damage
Peripheral nerves are comprised of various combinations of motor, sensory, and autonomic neurons. Nerve injuries are a common condition with a broad range of symptoms depending on the severity of nerve damage which presents various challenges to patients, ranging from mild discomfort to life-long impairment. PRP for nerve damage has been shown to be effective. Let’s dig in. Nerve injuries can be classified based on the severity of damage and which structures in the nerve have been damaged. The most severe case is the complete transection of the nerve, called neurotmesis. The most common is neuropraxia from acute or chronic compression of the nerve.
Read More About PRP for Nerve DamagePRP Injections
PRP is short for platelet-rich plasma, and it is autologous blood with concentrations of platelets above baseline values. The potential benefit of platelet-rich plasma has received considerable interest due to the appeal of a simple, safe, and minimally invasive method of applying growth factors. PRP treatments are a form of regenerative medicine that utilizes the blood healing factors to help the body repair itself by means of injecting PRP into the damaged tissue. In regenerative orthopedics, it is typically used for the treatment of muscle strains, tears, ligament and tendon tears, minor arthritis, and joint instability. There have been more than 30 randomized controlled trials of PRP…
Read More About PRP InjectionsHow Centeno-Schultz Approaches Guyon’s Canal Syndrome
Using platelet products to help nerve recovery is not a new concept! We have been treating nerve injuries from sciatica to carpal tunnel syndrome for years! Utilizing ultrasound guidance for nerve hydro-dissection with platelet lysate.
To understand more about HD of peripheral nerve entrapment syndromes watch here:
This page also has been excellent research showing success rates that are far beyond steroid injections! You can also download this resource.

Christopher J. Centeno, MD
Christopher J. Centeno, M.D. is an international expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate in orthopedics.
Dr. Centeno is one of the few physicians in the world with extensive experience in the culture expansion of and clinical use of adult bone marrow concentrate to treat orthopedic injuries. His clinic incorporates a variety of revolutionary pain management techniques to bring its broad patient base relief and results. Dr. Centeno treats patients from all over the US who travel to Colorado to undergo innovative, non-surgical treatments. Dr. Centeno has chaired multiple international research-based conferences. He also maintains an active research-based practice, with multiple publications listed in the US National Library of Medicine. Dr. Centeno has also served as editor-in-chief of a medical research journal dedicated to traumatic injury.
Dr. Centeno trained at the Baylor College of Medicine, Texas Medical Center, and the Institute for Rehabilitation Research. He hails from both Florida and New York and currently resides in Boulder, Colorado with his wife and three children.

John Schultz, MD
John R. Schultz M.D. is a national expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate for orthopedic injuries. He is board certified in Anesthesiology and Pain Medicine and underwent fellowship training in both. Dr. Schultz has extensive experience with same day as well as culture expanded bone marrow concentrate and sees patients at the CSC Broomfield, Colorado Clinic, as well the Regenexx Clinic in Grand Cayman. Dr. Schultz emphasis is on the evaluation and treatment of thoracic and cervical disc, facet, nerve, and ligament injuries including the non-surgical treatment of Craniocervical instability (CCI). Dr. Schultz trained at George Washington School of…
Read more
John Pitts, M.D.
Dr. Pitts is originally from Chicago, IL but is a medical graduate of Vanderbilt School of Medicine in Nashville, TN. After Vanderbilt, he completed a residency in Physical Medicine and Rehabilitation (PM&R) at Emory University in Atlanta, GA. The focus of PM&R is the restoration of function and quality of life. In residency, he gained much experience in musculoskeletal medicine, rehabilitation, spine, and sports medicine along with some regenerative medicine. He also gained significant experience in fluoroscopically guided spinal procedures and peripheral injections. However, Dr. Pitts wanted to broaden his skills and treatment options beyond the current typical standards of care.
Read more
Jason Markle, D.O.
Post-residency, Dr. Markle was selected to the Interventional Orthopedic Fellowship program at the Centeno-Schultz Clinic. During his fellowship, he gained significant experience in the new field of Interventional Orthopedics and regenerative medicine, honing his skills in advanced injection techniques into the spine and joints treating patients with autologous, bone marrow concentrate and platelet solutions. Dr. Markle then accepted a full-time attending physician position at the Centeno-Schultz Clinic, where he both treats patients and trains Interventional Orthopedics fellows. Dr. Markle is an active member of the Interventional Orthopedic Foundation and serves as a course instructor, where he trains physicians from around the world.
Read more
Brandon T. Money, D.O., M.S.
Dr. Money is an Indiana native who now proudly calls Colorado home. He attended medical school at Kansas City University and then returned to Indiana to complete a Physical Medicine and Rehabilitation residency program at Indiana University, where he was trained on non-surgical methods to improve health and function as well as rehabilitative care following trauma, stroke, spinal cord injury, brain injury, etc. Dr. Money has been following the ideology behind Centeno-Schultz Clinic and Regenexx since he was in medical school, as he believed there had to be a better way to care for patients than the status quo. The human body has incredible healing capabilities…
Read moreTreat Your Condition Safely And Effectively
Regardless of how you developed Guyon’s Canal Syndrome, we have been utilizing advanced regenerative treatment options for close to 2 decades…if you have been dealing with this and want to avoid surgery, give us a call for a consultation with one of our experts and we can discuss if you are a candidate for treatment!
Are you a candidate?