Cervical Radiculopathy
Cervical radiculopathy, often called “pinched nerve,” is a medical condition that occurs when a nerve in the neck is compressed or irritated at the point where it branches away from the spinal cord. This condition often leads to pain, numbness, or weakness in various parts of the arms or shoulders. Understanding the causes, symptoms, and treatment options for cervical radiculopathy is essential for individuals experiencing these discomforts. This blog aims to provide a comprehensive overview of this condition, offering insights into effective management and prevention strategies.
What Is Cervical Radiculopathy?
Radiculopathy is derived from the Latin roots of radix, meaning root, as in the nerve root, and patheia, meaning suffering. Cervical radiculopathy is a common musculoskeletal problem. This refers to a condition of the nerves in the neck becoming irritated, causing a variety of symptoms.
In the neck, there are seven bones. The nerves come out of spaces between the bones, called foramen, where a nerve can be pinched. The most common area in the neck for a pinched nerve is the C5-6 space followed by the C6-7 space after that.
There are several main causes of pinched nerves:
- Nerves can get pinched in the neck as a result of injured discs, such as disc bulges, protrusion, herniation, or disc annular tears.
- They can also get pinched from bone spurs or enlarged arthritic facet joints.
- Nerves can get pinched when there is less space due to a condition known as spondylolisthesis where there is a misalignment of the vertebral bodies.
- Other things that are rare such as infection, tumor, hematoma, or spinal fracture can cause pinched nerves as well.
- A pinched nerve can result from having previous surgery on the neck.
Cervical Radiculopathy Symptoms
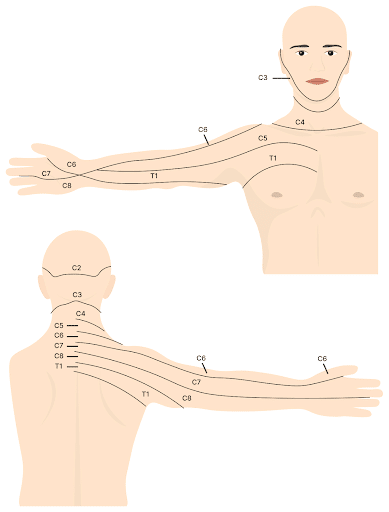
Since cervical radiculopathy affects the nerves, patients can feel symptoms anywhere along the course of the nerve from the neck into the shoulder, arm, elbow, forearm, wrist, hand, or fingers. The figure above shows how these regions correspond to the pathway of each nerve root that exits the cervical spine to the arm.
Numbness
Numbness refers to reduced sensation in the area of the body supplied by a specific nerve. For the neck nerves, this would be the area of the shoulder, arm, elbow, forearm, wrist, hand, and/or fingers.
Numbness can give your arm a sensation that it is “falling asleep.” Sometimes this can happen at night and wake you from your sleep. With numbness, there is a risk of injuring the extremity further, such as cutting or burning yourself more easily since the sensation is reduced. It can also cause you to drop items if the hand is numb and you don’t feel what you are holding.
Different nerve roots that are injured can cause numbness in different areas. Here are some examples of what is meant by numbness, corresponding to which nerve is being pinched:
- Numbness in the collarbone area can be coming from the C4 nerve.
- The C5 nerve commonly causes numbness around the outside of the arm and elbow.
- Irritation to the C6 nerve can cause numbness in the forearm and into the thumb and first digit.
- Irritation to the C7 nerve can cause numbness in the back of the arm, or towards the middle finger.
- Irritation for the C8 nerve can cause numbness in the last 2 fingers.
Pain
Cervical radiculopathy, unfortunately, can be the cause of pain that can show itself in various types of ways. Here are some things to know about pain and this condition:
- Pain can be sharp, stabbing abrupt, or jolting.
- Pain can be a burning sensation that may come and go or linger on.
- Pain can be aching deep pain that can be constant or intermittent.
- Pain can also be radiating from the neck to any part of the arm, shoulder, elbow, forearm, wrist, hand, or fingers. It may not radiate and you only feel pain in one or two of these areas.
- Pain can be made worse by certain positions, postures, movements, exercises, and/or activities.
Tingling
Tingling (or paresthesia) can cause the sensation of pins and needles that may be weird and/or uncomfortable.
Muscle Weakness
Muscle weakness can occur in any part of the upper extremity. It may be related to particular activities such as lifting the arm or shoulder, gripping things, working out, exercising, etc.
For instance, muscle weakness corresponding to C5 nerve root irritation can manifest as shoulder weakness. For the C6 nerves, it can manifest as shoulder and forearm weakness. For the C7 nerve, it can be triceps weakness, and for the C8 nerve, it can be a weakness in the hand or with grip strength.
Diving Deeper into Other Common Symptoms
In addition to numbness, pain, tingling, and muscle weakness, there are a variety of other symptoms that can be associated with cervical radiculopathy. These symptoms are often reflective of the nerve root that is affected and can impact an individual’s daily activities and overall quality of life.
Here are some of the other common symptoms that people may experience with cervical radiculopathy:
Abnormal Reflexes
Deep tendon reflexes (DTRs) are involuntary responses of muscles to a sudden stretch, typically elicited by a sharp tap from a reflex hammer on a tendon. They work through a simple neural circuit known as the monosynaptic reflex arc. When a tendon is tapped, the muscle attached to it is quickly stretched, stimulating specialized sensory receptors called muscle spindle fibers. These receptors then send an impulse via afferent (sensory) neurons to the spinal cord, where they directly synapse with efferent (motor) neurons.
Read More About Abnormal ReflexesArm Pain at Night
Arm pain at night can be miserable. The pain can interrupt your sleep and erode your quality of life. Irritability becomes increasingly more common. What are the causes? When should I worry about it? What are the treatment options for arm pain at night? The neck is composed of 7 boney building blocks numbered 1- 7. Sandwiched between the bones is a disc that functions as an important shock absorber. The cervical discs are susceptible to injury due to trauma, degeneration, repetitive motion, and surgery. Common disc injuries include disc bulges, and herniations. The injured disc can compress or irritate one or more nerves resulting in arm pain at night. It can…
Read More About Arm Pain at NightArm Throbbing
In many patients, irritated neck nerves don’t present as a symptom in the neck. In fact, sometimes the only symptoms of irritated nerves in the neck occur in the arm muscles, as either tightness, throbbing, or both. While the arm throbbing might be frustrating as it’s happening, you might not think a whole lot about it, especially if it only happens on occasion. However, ignoring it is not a good idea since it is often a warning signal of a bigger problem in the neck. These body connections occur all the way back to when we were a fetus, like the neck, shoulder, and arm.
Read More About Arm ThrobbingCervicalgia / Neck Pain
Cervicalgia is also known as neck pain, which is an all-too-common, unpleasant pain. Read here to learn the symptoms, diagnosis, and treatment options. We will discuss other causes for cervicalgia. What symptoms are associated with cervicalgia? How is cervicalgia diagnosed? What are the treatment options for cervicalgia? Cervicalgia is a medical term used to describe neck pain. It is very common and affects approximately 2/3 of the population at some point in their life. Cervicalgia is the 4th major cause of disability. Risk factors include injury, prior history of neck and musculoskeletal pain, jobs that require a lot of desk work, low social support, job insecurity, physical weakness, and poor computer station setup.
Read More About Cervicalgia / Neck PainFeeling Of Pins And Needles In Fingers
Are you experiencing the sensation of pins and needles in your fingertips? This is a common symptom of cervical radiculopathy. Although many conditions can cause pins and needles, if it is accompanied by neck pain, then cervical radiculopathy would be at the top of the diagnostic list. Cervical radiculopathy also referred to as a “pinched nerve.” is a medical syndrome that occurs when a nerve root in the neck ( cervical spine) becomes compressed or irritated leading to symptoms that include pain, numbness, tingling, and potentially weakness. It occurs in about 85 people per 100,000 (1). Read this post to find out more about cervical radiculopathy and how it can cause pins and needles in your fingertips.
Read More About Feeling Of Pins And Needles In FingersHand Numbness and Tingling
A 2023 study estimates that pain complaints account for 50-80% of emergency department visits – and up to 50% of those cases relate to what’s known as neuropathic pain, or nerve pain. This refers to paresthesia (or “pins and needles”), burning sensations, and numbness, symptoms that often indicate damage or disease of a somatosensory nerve. However, these symptoms are often non-specific: they don’t usually point to a specific disease and can indicate many different conditions of the peripheral nervous system, from neuropathy to cervical radiculopathy.
Read More About Hand Numbness and TinglingHands Stiff in the Morning
Hand stiffness can make simple tasks overwhelming. Why are my hands stiff in the morning? What are the treatment options for hand stiff in the morning? Are there new, natural treatment options to treat hands that are stiff in the morning? Our hands are central to virtually everything we do. Stiffness can compromise function and cause pain. What are the causes of hand stiffness in the morning? There are many which include: excessive daily wear and tear, medications that can cause hand swelling and stiffness. Common examples include hormones, calcium channel blockers for high blood pressure, steroids, anti-depressants, and NSAIDs, Diets high in salt, alcohol, and trauma.
Read More About Hands Stiff in the MorningLeft Arm Numbness
Treatment depends upon the underlying cause of the arm numbness. Left-arm numbness is a warning sign that requires attention. As noted above unexplained numbness requires immediate attention. At the Centeno-Schultz Clinic, we are experts in the treatment of left-arm numbness due to cervical nerve irritation, cervical stenosis, thoracic outlet syndrome, and peripheral nerve injuries. When appropriate first-line treatment should involve conservative care including physical therapy and stretching. Steroid injections should be avoided as they are toxic to orthopedic tissue and can accelerate damage. Surgery for Cervical Stenosis and Thoracic…
Read More About Left Arm NumbnessMotor Issues
Cervical radiculopathy is a condition caused by compression of a cervical nerve root, which can result in pain and sensorimotor deficits. Nerve roots are mixed nerves which are responsible for sensory and motor function. There are eight cervical nerve roots that branch off from the spinal cord, labeled from C1-C8. Each cervical nerve root supplies a particular region of skin, called a dermatome,and innervates certain groups of muscles, called a myotome. When the cervical nerve root is compressed, the sensory supply to the dermatome in the upper limb can be altered. This can lead to pain, decreased sensation, the feeling of pins and needles, and even numbness. This can also coincide with muscle weakness, and a decreased reflex response.
Read More About Motor IssuesMuscle Pain After Cervical Fusion Surgery
Cervical Fusion is a major surgery that involves joining one or more of the spinal bones together using screws, bolts, and plates (1). The hardware may be placed in the front (anterior) or the back( posterior) of the cervical spine. The disc between the spinal bones is often times removed and replaced with a bone graft or a spacer. The neck of composed of 7 boney building blocks that are numbered from 1-7. The letter C is associated with the numbers to designate the cervical spine. Hence the bones in the neck are C1 through C7. Sandwiched between neck bones are important shock absorbers called discs. A cervical fusion surgery removes…
Read More About Muscle Pain After Cervical Fusion SurgeryNeck Pain And Dizziness
Our body’s balancing system is compromised of three separate systems that work closely together to keep the body in balance: the eyes, inner ear, and upper cervical spine. The upper cervical spine contains and processes information about your position in space and communicates this information to your eyes and inner ears via nerves. There is a constant highway of electrical signals between the cervical spine, inner ear, and eyes that keep us upright, make us aware of our position and enable us to walk, move and run. This balancing system requires the inner ear, eyes and cervical spine to be operational…
Read More About Neck Pain And DizzinessNeck Spasms
Typically they involve the entire neck but may be more intense on one side leading to an involuntary rotation of the neck. Neck spasm and neck pain are common as 2/3rd of all people will experience it at some time. It occurs most often during middle age with women being affected more than men. muscle tightness. The neck muscles may feel hard or knotted to the touch. When severe it may be difficult to bend or rotate the neck due to pain and muscle tightness. The pain may extend down into the shoulders or up into the base of the skull with the onset of a headache.
Read More About Neck SpasmsPain In Left Side Of Neck
Almost everyone has experienced a sore or stiff Neck at some point. The overall prevalence of Neck pain ranges from 04. to 86.8% of the general population (1). Read more to learn the signs, symptoms, causes of treatment options for pain in the left side of Neck. Neck pain can arise from a number of different conditions. Common causes of minor, intermittent Neck pain include fatigue, improper sleeping position, stress and overactivity. If neck pain persists it is a warning sign that you may have a problem that warrants investigation. Think of it as the red engine light on your car. It is warning that if left unchecked can progress to serious and expensive consequences.
Read More About Pain In Left Side Of NeckShoulder Pain Radiating Down Arm to Fingers
Common Cervical Radiculopathy symptoms include neck pain, arm pain, shoulder pain radiating down arm to fingers, numbness, tingling, and weakness. Cervical Radiculopathy is a clinical condition in which a nerve or nerves in your neck become irritated or compressed. It is also known as ” a pinched nerve,” The causes are discussed below. It can affect individuals of any age with peak prominence between ages 40-50 years of age. Cervical Radiculopathy is due to spinal nerve inflammation, irritation, or compression. The most common causes of Cervical Radiculopathy are: Disc Injury – The disc is an important shock absorber. Unfortunately, it is susceptible to injury.
Read More About Shoulder Pain Radiating Down Arm to FingersStiff Neck
A painful stiff neck affects one in three people every year, and is most prevalent in the 35-49-year age group. It causes significant disability for all those affected, but is more commonly seen in women. A stiff neck can be a symptom of vascular disease, inflammatory disorders, infection, and malignancy. Therefore, it needs to be evaluated properly before any treatment begins. In this article, we’ll discuss what causes a painful stiff neck, how to diagnose it, and some common treatments.
Read More About Stiff NeckTingling Sensation in the Hands
Have you ever felt the sensation of a thousand tiny pins and needles pricking your hands or the subtle, electric tingling that runs down your fingers like a gentle current? Tingling sensations in the hands are more common than you might think and can be triggered by a multitude of factors, from temporary nerve compression to chronic medical conditions. While often dismissed as a momentary inconvenience, this seemingly innocuous tingling can sometimes be a signal from your body, a signpost pointing to underlying health concerns. In this article, we delve into the intriguing world of tingling sensations in the hands, unraveling the causes, potential implications, and, most importantly, what you can do to address them.
Read More About Tingling Sensation in the HandsCommon Causes and Risk Factors of Cervical Radiculopathy
Now that we have a visual understanding of the cervical dermatomes (the areas of skin supplied by particular spinal nerves) and their roles in the upper extremity, let’s delve into the common causes of cervical radiculopathy. This condition can arise from various factors that impact the nerves in the cervical spine. Understanding these causes is crucial for both prevention and effective treatment strategies. Let’s explore some of the most frequent contributors to the development of cervical radiculopathy.
Age
One can be at greater risk of cervical radiculopathy with age. The most common onset happens in the 40s and 50s. As we get older, there are more opportunities to have these injuries from repetitive use stress, and our natural ability to heal lessens.
Obesity
Obesity can be a significant risk factor for cervical radiculopathy due to the extra strain it places on the spine. Excessive body weight increases the mechanical stress on the spinal column, particularly in the cervical (neck) region. This additional pressure can accelerate the degenerative processes of the spine, such as the wearing down of intervertebral discs and the formation of bone spurs, both of which can lead to nerve compression.
Furthermore, obesity can contribute to a general inflammatory state in the body. Chronic inflammation can exacerbate degenerative changes in the spine and potentially lead to swelling around the cervical nerves, increasing the likelihood of nerve irritation or compression.
Another aspect to consider is that obesity often limits physical activity, leading to muscle weakness and decreased flexibility. This can result in poorer support and stabilization of the cervical spine, making it more susceptible to injuries that can cause radiculopathy.
Overall, the combination of increased mechanical stress, heightened inflammation, and reduced muscular support in individuals with obesity creates a conducive environment for the development of cervical radiculopathy. Managing weight through a healthy diet and regular exercise is not only beneficial for overall health but also crucial in reducing the risk of spinal disorders, including cervical radiculopathy.
Diabetes
Diabetes, a chronic condition characterized by high blood sugar levels, can have numerous effects on the body, including an increased risk of developing cervical radiculopathy.
High glucose levels in the bloodstream can lead to nerve damage, known as diabetic neuropathy, which may exacerbate the vulnerability of the cervical nerves. Additionally, diabetes can contribute to degenerative changes in the spine, such as disc herniation or bone spurs, which can compress the cervical nerves.
This compression can manifest as cervical radiculopathy, resulting in pain, weakness, or numbness in the neck and arms. Individuals with diabetes need to manage their condition effectively and be aware of these potential complications. Regular check-ups and proactive healthcare can help in identifying and addressing such issues early, thereby reducing the risk of cervical radiculopathy.
Rheumatoid Arthritis (RA)
Rheumatoid arthritis (RA) is a chronic inflammatory disorder that can significantly contribute to the development of cervical radiculopathy. RA primarily affects joints, causing pain and swelling, but it can also impact the cervical spine. In the neck, RA can lead to inflammation and erosion of the joints and ligaments, destabilizing the vertebral column. This instability can result in subluxation (partial dislocation) of the vertebrae, which, in turn, can compress the nerves exiting the spinal cord.
Such compression can manifest as cervical radiculopathy, characterized by pain, numbness, or weakness in the neck, shoulders, arms, and hands. Individuals with RA must monitor their neck health and seek medical attention if they experience symptoms consistent with cervical radiculopathy. Early intervention and effective management of RA can help mitigate these risks and maintain spinal health.
Smoking
Smoking can be a major risk factor for cervical radiculopathy as it impairs blood flow and nutrient delivery to the spinal tissues, exacerbating degenerative changes in the cervical spine. Additionally, smoking contributes to inflammation and reduced oxygenation in tissues, increasing the vulnerability of cervical nerves to compression and damage.
Traumatic Injuries
Traumatic injuries such as motor vehicle accidents, falls, whiplash, etc. can cause injury to the cervical bones, discs, and joints that can lead to pinching of the nerve or cervical radiculopathy.
Also, minor injuries that build up over time due to exercise, activities, and minor falls can be related as well. Nerve stretch injuries such as rapid neck or shoulder movements or trauma, like from a football stinger, can also be a cause of cervical radiculopathy.
Common Treatment Options for Cervical Radiculopathy
Cervical radiculopathy can be treated with conservative and invasive measures as well as surgery as a last resort.
Home Therapies
- Initial home therapies might just be relative rest, stretching, massage, heat, ice, and taking anti-inflammatory supplements like turmeric, fish oil, etc.
- Other conservative measures would be seeing a licensed professional such as a physical therapist. A good physical therapist will evaluate you, work on your posture, alignment, and any muscle asymmetries, and work on relaxing tight muscles and strengthening weak muscles.
- Other similar modalities might be Egoscue therapy, muscle activation technique or MAT, myofascial release, Rolfing, chiropractic care including gentle manipulation, cervical traction, or cervical decompression.
- Sometimes a cervical collar can be used. Collars can be soft or hard, for more restriction of the range of motion. Typically, you do not want to wear a collar for too long as this can weaken the muscles that support the neck. Still, sometimes collars might be highly indicated if there is a more severe injury with instability.
Supplements
Supplements such as turmeric, fish oil, glucosamine chondroitin, and tart cherry juice can help reduce inflammation and help with the pain.
Pain Medications
Pain medications for radiculopathy serve two primary purposes: firstly, they provide relief from the discomfort and pain associated with nerve compression, improving the patient’s quality of life. Secondly, by reducing pain and inflammation, these medications can enhance the patient’s ability to participate in other therapeutic activities, such as physical therapy, which are essential for long-term management and recovery from radiculopathy.
Over-the-Counter Medications
Over-the-counter medications such as Acetaminophen or Tylenol can help with pain. Tylenol is mostly safe unless taken in doses of more than 1000mg at a time, and it is recommended not to exceed 3000mg in a day. This can increase the risk of liver failure and death.
NSAIDs
Over-the-counter oral nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen, Aleve, etc, or prescription NSAIDs like Celebrex or meloxicam etc can be tried. They help with pain and inflammation and can be taken for a few days or a week.
However, they should not be taken often or for too long as they have many risks. These include stomach upset, GI bleeds, kidney or liver problems, reducing the body’s ability to heal, and increasing the risk of high blood pressure, heart attack, or stroke.
Steroids and Narcotic Pain Medication
A course of oral steroids can be used to reduce inflammation. However, these are very powerful and dangerous drugs that come with a host of side effects, and the longer one uses them the higher the risk of severe side effects such as bone death (osteonecrosis), hormonal problems, weight gain, increase in blood sugars, bone loss, and inhibiting healing mechanisms. These are not recommended for these reasons.
Sometimes narcotic pain medications can be used, but in high doses, these have significant risks of addiction and death and really should only be used for temporary severe acute pain or pain post-surgery or following a procedure. Please check with Dr Markle – should this be ‘known as’ rather than ’caused by’?
Surgery
Surgery should be a last resort treatment option only, with the exception being a condition known as cervical myelopathy, which is a condition where the spinal cord is getting a direct injury causing weakness in the leg or arm. This is more of a surgical emergency and needs immediate surgical care.
The next reason for surgery would be a direct mechanical injury to the nerve where there is a large disc herniation or bone spur that is directly pressing on the nerve, causing radiculopathy.
This means that the patient has a nerve injury causing severe pain and weakness that is not improving, or is worsening over a short period. This would be a high surgical candidate as well.
In most cases, however, the nerves are getting chemical irritation from less space around them from disc bulge and protrusion, herniation, bone spurs, joint swelling, or instability, in which case conservative care or injection therapy would be the best first-line therapies to try.
However, far too often patients are being offered surgery as the first line of therapy without mechanical symptoms, without trying physical therapy or with trying physical therapy but not injection-based therapies, or not trying platelet-rich plasma (PRP) or bone marrow concentrate with stem cells first.
Performing surgery before exhausting all other safer methods means increased use of unnecessary, expensive interventions and invasive surgeries that have many potential risks and down-the-road complications.
Artificial Disc Replacements (ADR)
Artificial disc replacement or ADR is a surgery where a disc is removed and replaced with an artificial disc. The potential advantage of these is to maintain some of the mobility versus fusion.
However, studies still show the same risk of adjacent segment disease as described above (2) and the potential for the artificial disc to wear out over 10-20 years, requiring revision surgery in the future. Also, they can cause an increase in metal ions in the blood (3).
Posterior Cervical Laminectomy
Posterior cervical laminectomy or foraminotomy with or without fusion is a surgery in which the doctor goes in from the back and removes some of the bone that is behind the nerves to open up space. This may be done with or without fusion from the back of the neck as well.
Without a fusion, this can lead to some further neck instability and muscle weakness. Still, with fusion, you get more of the risk of adjacent segment disease, higher complications, and more risk in general (4). There may be little additional benefit to fusion.
Deep Dive Into All Treatment Options
ACDF Surgery
ACDF stands for “anterior cervical discectomy and fusion.” It is a surgical procedure performed on the neck to relieve pressure on the spinal cord or nerve roots caused by a damaged or degenerated disc. During the procedure, the surgeon removes the damaged disc and replaces it with a bone graft or synthetic implant. Metal plates and screws may be used to hold the vertebrae together during the fusion process. ACDF surgery can help relieve symptoms such as neck pain, numbness, tingling, and weakness in the arms or hands caused by nerve compression in the neck. It is a commonly performed procedure…
Read More About ACDF SurgeryAnterior Cervical Discectomy And Fusion (ACDF) For Neck Pain
Anterior cervical discectomy and fusion (ACDF) surgery is a surgical procedure used to treat cervical radiculopathy in the neck region. It is also an effective treatment for those with severe neck pain due to spondylosis, tumors, fractures, and herniated discs. There are two stages of the ACDF surgery: discectomy and spinal fusion. In an anterior cervical discectomy and fusion surgery, the diseased disc is first removed and a bone graft is inserted in its place. The graft is then held in place by a plate and fused with the cervical vertebra above and below.
Read More About Anterior Cervical Discectomy And Fusion (ACDF) For Neck PainCervical Epidural Steroid Injection
The neck pain started out as a dull ache but steadily progressed. It becomes constant and oftentimes keeps you up at night. Turning your head can send an electrical current down your arm. Rest, medications and physical therapy failed to provide much relief. Your doctor referred you to a pain clinic for a Cervical Epidural steroid injection. The injection was performed at an ambulatory surgical center. Unfortunately, the pain is now worse. What is a Cervical Epidural injection? Are there different types of Cervical Epidural injections? What are…
Read More About Cervical Epidural Steroid InjectionCervical Fusion
Cervical Fusion is often recommended when chronic neck pain problems worsen over time. What exactly is it? Cervical Fusion is a major surgery that involves joining one or more of the spinal bones together using screws, bolts, and plates (1). The hardware may be placed in the front (anterior) or the back( posterior) of the Cervical spine. The disc between the spinal bones is often times removed and replaced with a bone graft or a spacer. The neck of composed of 7 boney building blocks that are numbered from 1-7. The letter C is associated with the numbers to designate the Cervical Spine.
Read More About Cervical FusionCervical Radiofrequency Ablation
Cervical radiofrequency ablation is used to treat cervical facet mediated pain. Cervical facet pain can come in many types of pain from muscle spasms, neck pain, shoulder pain, sharp, stabbing, throbbing, deep ache, upper back pain, mid back pain, headaches, and much more. Pain is generated by several small nerves that innervate the facet joint (medial branch nerves). Radiofrequency ablation is a technique used by traditional interventional pain management physicians. Cervical Radiofrequency ablation burns the nerves (medial branches) that innervates the facet joints to cut off the pain signal.
Read More About Cervical Radiofrequency AblationFacet Joint Injections
A facet joint injection is a common medical procedure utilized in the diagnosis and treatment of facet joint injuries. It can be performed in the cervical, thoracic, and lumbar spine and may involve one or more facet joints. A facet injection involves the placement of a needle under an x-ray or ultrasound directly into the targeted facet joint and the administration of medication. The injected medicine goes directly into the joint and for this reason, some may refer to a facet injection as an intra-articular facet injection. Intra-articular refers to within the joint. The procedure can be diagnostic or therapeutic.
Read More About Facet Joint InjectionsProlotherapy Injections
It has been successful in the treatment of many disorders including neck, shoulder, knee, and ankle pain. Dr. Centeno recently published an article in The Journal of Prolotherapy in which he discusses the use of x-ray guidance with prolotherapy. This ensures that the injection is in the correct place to maximize clinical results. Dr. Centeno discusses the use of prolotherapy for the treatment of neck, knee, sacroiliac joint, ankle, ischial tuberosity, and shoulder pain. At the Centeno-Schultz Clinic x-ray guided prolotherapy is just one of the therapies utilized in the successful treatment of pain. Regenerative injection therapy (RIT) or prolotherapy…
Read More About Prolotherapy InjectionsPRP Injections
PRP is short for platelet-rich plasma, and it is autologous blood with concentrations of platelets above baseline values. The potential benefit of platelet-rich plasma has received considerable interest due to the appeal of a simple, safe, and minimally invasive method of applying growth factors. PRP treatments are a form of regenerative medicine that utilizes the blood healing factors to help the body repair itself by means of injecting PRP into the damaged tissue. In regenerative orthopedics, it is typically used for the treatment of muscle strains, tears, ligament and tendon tears, minor arthritis, and joint instability. There have been more than 30 randomized controlled trials of PRP…
Read More About PRP InjectionsHow Do Doctors Diagnose Cervical Radiculopathy?
- The first step in a doctor’s diagnosis will be taking a detailed history, asking you about the onset, duration, history, characterization, and quality of your symptoms, and taking an overall medical history and family history.
- A detailed physical examination will be a key component of the diagnosis.
- The doctor may look for decreased sensation in the neck and upper extremities.
- They will check reflexes to see if there are any asymmetries in reflexes.
- They will check strength to see if there is a weakness that you may or may not perceive.
- They can do a specialized test such as a Spurling’s maneuver, where you extend your head and rotate with compression to see if it reproduces your symptoms.
- They will palpate tender areas around the neck and nerves in the shoulders to see if they are painful.
After a thorough examination, several additional imaging modalities can help clarify the exact cause and extent of your radiculopathy:
X-Ray
X-rays can show bony pathology such as fractures and can give clues to disc space, bone spurs, and joint arthritis.
A specialized X-ray called a digital motion X-ray can find the same clues in addition to taking pictures with the patient moving their head. This is a much better test to look for dynamic instability in the neck that can contribute to the pinching of the nerves and damage to other structures.
MRI
An MRI can be used as the best test to visualize the soft tissues such as the discs, nerves, joint cartilage, and muscles. Our physicians will review the imaging themselves, rather than relying on a radiologist’s reports! This will help delineate who is and who isn’t a candidate for orthobiologics.
CT Scan
A CT scan may be used if you cannot get an MRI or if the doctor highly considers surgery and wants detailed pictures of the bony anatomy.
NCS/EMG
Other tests that can be used are nerve conduction studies and electromyography or NCS/EMG. This test can be helpful when there is severe irritation or nerve damage and is pretty specific.
However, this test can be painful and is not very sensitive, meaning only more severe nerve injuries are typically picked up with an EMG. It also can help decipher cervical radiculopathy from nerve injuries elsewhere like in the carpal tunnel, ulnar nerve, or other peripheral nerves.
When Should You See Your Doctor?
If any of the following six scenarios pertain to you, you should see a doctor:
- You should see your doctor if you are having pain, numbness, tingling, or weakness that is persistent and lasting longer than a few days up to a few weeks despite conservative measures.
- Certainly, if you have weakness, especially with rapid onset or worsening, you should go see your doctor immediately.
- If you are getting associated symptoms such as difficulty with urination or bowel movements, bowel and bladder accidents, leg pain or weakness, or severe arm weakness, you should see your doctor right away.
- If you have tried six weeks or so of conservative therapy and things are not improving, you should see a doctor.
- You should also see a doctor if anything is rapidly getting worse.
A lot of patients will resolve their symptoms with conservative measures after several weeks but it can take up to four to six months as well. For problems that are not helped with conservative measures, injection-based therapies will likely be needed to help resolve the issue.
Steroid-type injections will need to be repeated more frequently, whereas PRP and bone marrow concentrate procedures with stem cells typically provide longer-lasting results and need to be repeated less frequently.
If there is a condition where surgery is absolutely needed, the earlier the surgical intervention, the better. However, in most cases, surgery is not absolutely needed.
Regenerative Medicine for Cervical Radiculopathy
Anyone considering getting an orthobiologic (PRP or bone marrow concentrate) here is a quick guide to make sure you will get the most out of your treatment.
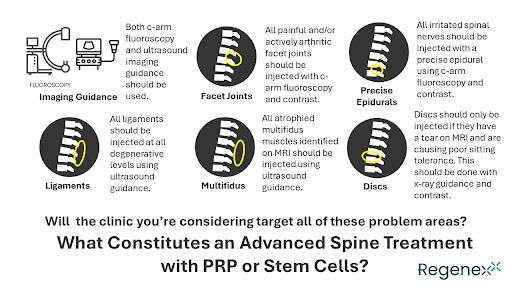
Here at the Centeno-Schultz Clinic, we are board-certified musculoskeletal specialists, fellowship-trained in regenerative medicine and orthobiologic treatments.
This means that we are trained to diagnose and treat all musculoskeletal problems non-surgically with various methods, including precise injections of substances like PRP or bone marrow concentrate that allow your body to heal itself.
We were the first clinic in the world to start doing these types of injections for orthopedic uses, so we have the professional experience to treat chronic pain. We take a holistic approach to care and take additional time to spend with patients on history, exams, and reviewed imaging to make sure we have accurate diagnoses.
We do not only talk about injection-based therapy, we also talk about diet, supplements, and adjunctive therapy modalities.
With our therapies, these are all personalized to the specific person.
Unlike the traditional pain model which focuses on just one area to treat at a time that is typically something that is causing pain, we focus on the functional spinal unit or FSU (5), which treats multiple areas that are contributing to the underlying cause, thus providing better and longer lasting results based on our research.
We also track all of our patients in the registry to collect outcome data to discuss chances of success and improve therapies as we learn more.
Get World-Class Treatment for Your Cervical Radiculopathy
If you or anyone you know has been dealing with signs and symptoms of a pinched nerve or cervical radiculopathy, contact the Centeno-Schultz Clinic for an evaluation right away.
Are you a Candidate?

Christopher J. Centeno, MD
Christopher J. Centeno, M.D. is an international expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate in orthopedics.
Dr. Centeno is one of the few physicians in the world with extensive experience in the culture expansion of and clinical use of adult bone marrow concentrate to treat orthopedic injuries. His clinic incorporates a variety of revolutionary pain management techniques to bring its broad patient base relief and results. Dr. Centeno treats patients from all over the US who travel to Colorado to undergo innovative, non-surgical treatments. Dr. Centeno has chaired multiple international research-based conferences. He also maintains an active research-based practice, with multiple publications listed in the US National Library of Medicine. Dr. Centeno has also served as editor-in-chief of a medical research journal dedicated to traumatic injury.
Dr. Centeno trained at the Baylor College of Medicine, Texas Medical Center, and the Institute for Rehabilitation Research. He hails from both Florida and New York and currently resides in Boulder, Colorado with his wife and three children.

John Schultz, MD
John R. Schultz M.D. is a national expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate for orthopedic injuries. He is board certified in Anesthesiology and Pain Medicine and underwent fellowship training in both. Dr. Schultz has extensive experience with same day as well as culture expanded bone marrow concentrate and sees patients at the CSC Broomfield, Colorado Clinic, as well the Regenexx Clinic in Grand Cayman. Dr. Schultz emphasis is on the evaluation and treatment of thoracic and cervical disc, facet, nerve, and ligament injuries including the non-surgical treatment of Craniocervical instability (CCI). Dr. Schultz trained at George Washington School of…
Read more
John Pitts, M.D.
Dr. Pitts is originally from Chicago, IL but is a medical graduate of Vanderbilt School of Medicine in Nashville, TN. After Vanderbilt, he completed a residency in Physical Medicine and Rehabilitation (PM&R) at Emory University in Atlanta, GA. The focus of PM&R is the restoration of function and quality of life. In residency, he gained much experience in musculoskeletal medicine, rehabilitation, spine, and sports medicine along with some regenerative medicine. He also gained significant experience in fluoroscopically guided spinal procedures and peripheral injections. However, Dr. Pitts wanted to broaden his skills and treatment options beyond the current typical standards of care.
Read more
Jason Markle, D.O.
Post-residency, Dr. Markle was selected to the Interventional Orthopedic Fellowship program at the Centeno-Schultz Clinic. During his fellowship, he gained significant experience in the new field of Interventional Orthopedics and regenerative medicine, honing his skills in advanced injection techniques into the spine and joints treating patients with autologous, bone marrow concentrate and platelet solutions. Dr. Markle then accepted a full-time attending physician position at the Centeno-Schultz Clinic, where he both treats patients and trains Interventional Orthopedics fellows. Dr. Markle is an active member of the Interventional Orthopedic Foundation and serves as a course instructor, where he trains physicians from around the world.
Read more
Brandon T. Money, D.O., M.S.
Dr. Money is an Indiana native who now proudly calls Colorado home. He attended medical school at Kansas City University and then returned to Indiana to complete a Physical Medicine and Rehabilitation residency program at Indiana University, where he was trained on non-surgical methods to improve health and function as well as rehabilitative care following trauma, stroke, spinal cord injury, brain injury, etc. Dr. Money has been following the ideology behind Centeno-Schultz Clinic and Regenexx since he was in medical school, as he believed there had to be a better way to care for patients than the status quo. The human body has incredible healing capabilities…
Read moreMore Resources for Cervical Radiculopathy
-
Learn Why Your Neck Hurts
Globally, neck pain is estimated to affect 203 million people, making it one of the most common musculoskeletal pains worldwide. It often stems from a combination of factors, such as muscle strain, poor posture, and degenerative disc conditions. This pain can limit movement, disrupt daily life, and, in severe cases, impact overall health. While some…
-
The L5 Vertebra: Everything You Need to Know
The spine, consisting of 33 individual bones called vertebrae, is divided into five major regions: cervical (neck), thoracic (upper back), lumbar (lower back), sacral (pelvic region), and coccygeal (tailbone). These vertebrae are separated by intervertebral discs, which act as cushions and allow for flexibility in movement. The lumbar spine, also known as the lower back,…
-
Why Does My Neck Hurt?
Neck pain can result from various factors, including poor posture, muscle strain, injury, or underlying medical conditions. It can be treated effectively when diagnosed properly. Treatment options may include physical therapy, pain management, exercise, and lifestyle changes to address the root causes of the pain and significantly improve your comfort and quality of life. If…
-
Muscles Of The Neck
The muscles of the neck are a complex network of tissues that play a crucial role in supporting the head and facilitating a wide range of movements essential for everyday activities. This intricate system of muscles is responsible for a variety of functions, making them indispensable for maintaining both stability and mobility in the neck…
-
Neck Pain Causes
Neck pain is a common musculoskeletal complaint. Over twenty-five million Americans are absent from work for eleven days on average due to neck pain (1). Neck pain has many causes and is often considered multifactorial. As a result, it is especially important to diagnose the cause of the neck pain so that it can be…
-
Exploring the Lumbosacral Joint: What Should You Be Wary Of?
The L5 S1 joint, or the lumbosacral joint, is a critical joint. It lies between the lumbar segment of the spine and the auricular processes of the sacrum. The L5-S1 joint plays a vital role in transmitting the weight of the body via the sacrum and ilium downwards. The weight is distributed to the femur…
-
Where Is The Thoracic Spine?
The thoracic spine is a region of the spine that is located in the middle back. It is located below the cervical spine and above the lumbar spine. It is composed of 12 vertebrae that are numbered T1-12. The T denotes the thoracic spine. It has many important functions which are discussed below. Location Of The…
-
Anterior Cervical Discectomy and Fusion Complications
ACDF stands for Anterior Cervical Discectomy and Fusion. It is a surgical procedure to treat cervical spine (neck) problems such as herniated disc, degenerative disc disease, or spinal stenosis. In this article, we will review what this surgery is and discuss anterior cervical discectomy and fusion complications. A brief overview of what the surgery entails:…
-
What is a Cervical Disc?
There are 23 discs in the spine: 6 in the cervical region (neck), 12 in the thoracic region (middle back), and 5 in the lumbar region (lower back). The disc’s function is to provide flexibility and stability to the spine. The disc absorbs approximately 70% of the forces placed on the spine in multiple movements…