Osteoarthritis (OA)

Osteoarthritis (OA) is a progressive joint disorder characterized by the breakdown of cartilage, the cushioning between the joints’ components. Typically, it affects joints like hips, hands, knees, and the spine, and, if left unaddressed, can lead to pain, stiffness, and reduced mobility.
Although osteoarthritis can emerge at any age, it is more prevalent in older adults. Today, this condition affects nearly 600 million people worldwide, making it one of the leading causes of disability.
What Is Osteoarthritis?
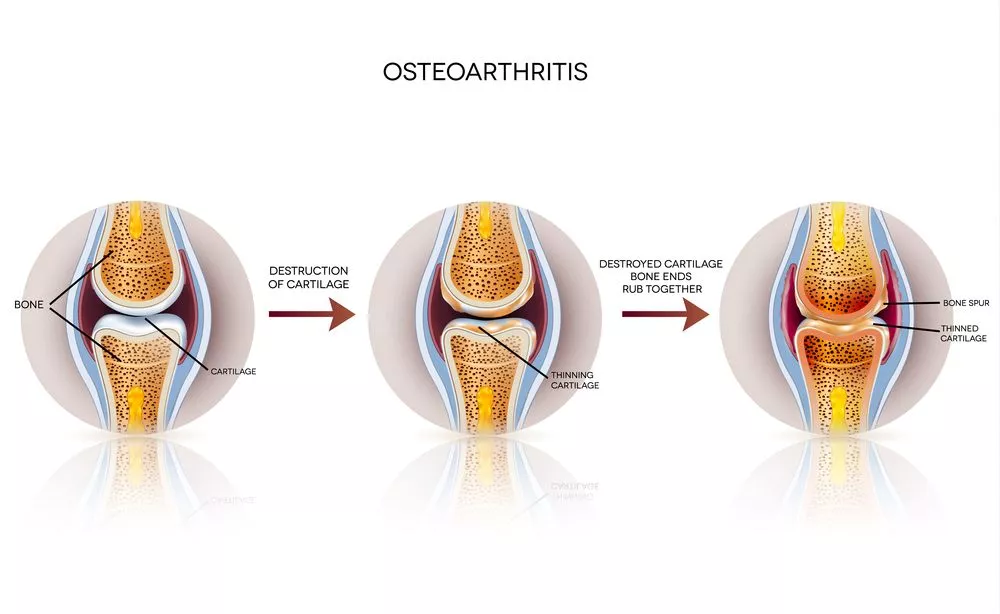
In people with OA, low-grade chronic inflammation causes the progressive breakdown of the cartilaginous components of joints like the hands, knees, and spine. As the cartilage breaks down, the joints remain unprotected and exposed to friction and shock during movement.
Over time, this causes the ends of the bones to deteriorate and rub against one another, causing pain, swelling, and reduced range of motion.
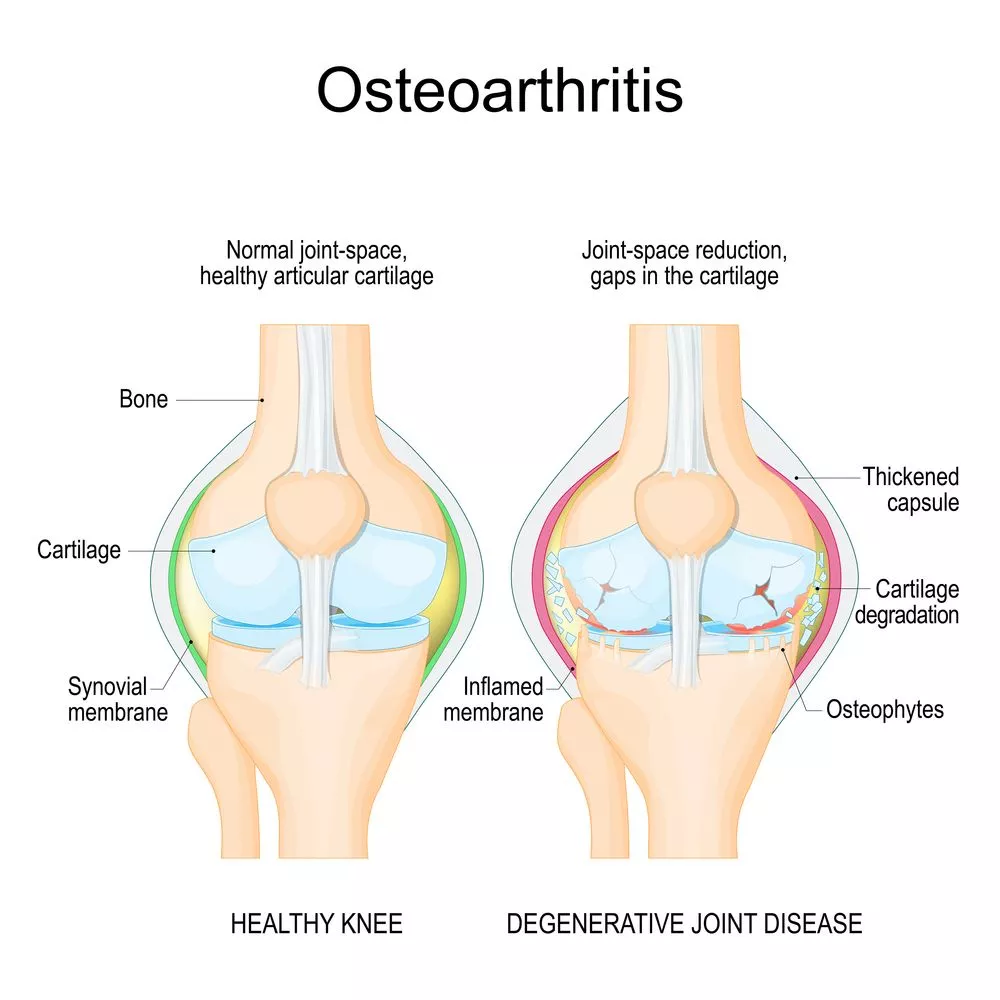
As the damage, inflammation, and irritation begin to affect nearby structures and tissues (e.g.: ligaments and tendons), OA can cause abnormal changes in the bone, severe mobility issues, and even disability.
Although OA is typically associated with aging, it can affect anyone, due to risk factors such as obesity, diabetes, repetitive stress on the joints (due to work or sports activities), previous injury, or defects, such as having a thinner cartilage.
- Which Body Parts Does Osteoarthritis Affect?
The low-grade inflammation that characterizes OA disrupts the normal rate at which cartilage is regenerated by the body, leading to an excessive loss of soft tissues. As the cartilage deteriorates, the bones can rub against each other, causing damage and inflammation to the bone and synovium, which lines the joint and produces lubricating fluid.
OA can affect any joint, but it typically affects the following ones:
- Hands: OA in the hands can lead to stiffness, swelling, and pain in the fingers and base of the thumb. This can affect fine motor skills, making tasks such as buttoning a shirt challenging. It’s estimated that about half of all women and one-quarter of all men will suffer from hand OA at one point in their lives.
- Knees: The knees are commonly impacted by OA, leading to pain, swelling, and stiffness, which can impair walking, climbing stairs, and other daily activities. Knee OA often causes a grinding sensation and can lead to decreased range of motion. Around 14 million people are estimated to have symptomatic knee OA in the US alone.
- Back: OA in the spine, particularly in the lower back, can cause pain and stiffness. This may result in reduced flexibility and mobility, impacting daily functions like bending or lifting.
- Neck: In the neck, OA leads to pain and stiffness, often resulting in a reduced range of motion and bone spurs. This can make it difficult to rotate the head fully, impacting activities that involve looking over the shoulder or maintaining certain postures.
Recognizing the Signs and Symptoms
Osteoarthritis manifests itself with a range of symptoms, which can vary in intensity and nature. One study has found that between 4% and 43% of those showing MRI signs of OA are asymptomatic.
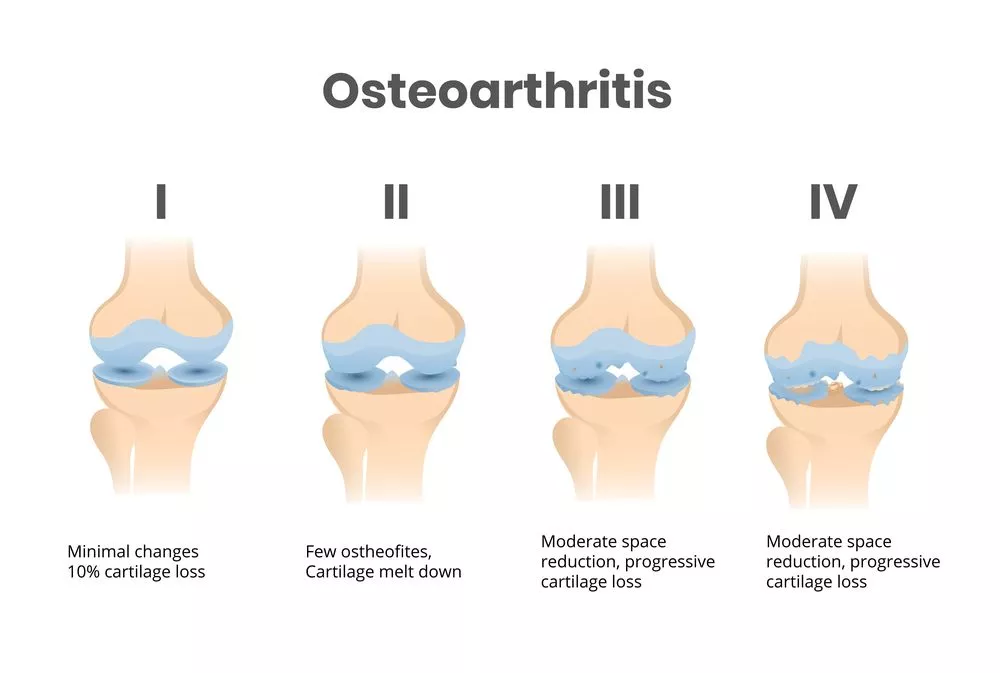
Additionally, given that symptoms tend to develop over time and progress alongside joint degeneration, you are likely to only experience mild discomfort at first. However, leaving the early symptoms of OA unaddressed can lead to irreparable joint damage and, in time, disability. Below are some of the telltale signs to be mindful of.
Joint Weakness
Joint weakness in OA often results from repetitive stress and damage to joint structures such as cartilage and ligaments. Over time, this leads to the weakening of muscles, tendons, and ligaments around the affected joint, making it difficult to support the overall structure, lift weight, or maintain grip strength.
Joint Pain
Pain is a hallmark symptom of OA, resulting from the breakdown of cartilage, which leads to bones rubbing against each other. This friction further exacerbates inflammation, which can cause intense discomfort and pain in and around the joint. The discomfort typically worsens with activity or after prolonged periods of inactivity (e.g.: in the morning after waking up) and improves with rest, settling in as a deep, aching sensation that can be localized.
Joint Swelling and Stiffness
Swelling and stiffness are hallmarks of active inflammation, even if it is low-grade. They occur in response to joint damage: when the cartilage is torn or broken down, the synovium, or joint lining, produces extra fluid to cushion the joint, resulting in swelling.
Stiffness, which is a consequence of bone damage and swelling, is often more noticeable in the morning or after periods of inactivity, during which the joint fluids settle and thicken.
Limited Motion
As OA progresses, joints can become less flexible due to the damage to cartilage and bones and the formation of bone spurs. This limits the range of motion, making it harder to perform everyday activities like bending, reaching, or walking.
Estimates show that around 80% of those with OA have some degree of movement limitation, and a quarter of patients can’t perform major activities of daily living.
Why Do Joints Wear Down Over Time?
Osteoarthritis typically develops as a result of various causes and risk factors that affect joint health over time. These include:
- Aging: As you age, the wear and tear on cartilage accumulate, reducing its ability to cushion joints. Additionally, the body’s capacity for repairing cartilage and maintaining joint health decreases with age.
- Joint injury: Previous joint injuries can accelerate the wear and tear process in joints. When a joint is injured, the cartilage can be damaged, and if it doesn’t heal properly, this can lead to OA later. For instance, a torn meniscus or ligament damage in the knee can disrupt normal joint mechanics, speeding up cartilage wear.
- Heredity: Genetics plays a significant role in the development of OA. Specific genetic traits can make cartilage more susceptible to breaking down. For example, inherited abnormalities in the shape of the bones around a joint or being born with thinner cartilage can lead to an increased risk of OA.
- Obesity: Extra body weight puts weight-bearing joints, like hips and knees, under undue stress, which can speed up the wear and tear of cartilage. Additionally, fat tissue produces proteins that can cause harmful inflammation in and around your joints, contributing to joint damage. Studies show that those with a BMI greater than 30 kg/m2 are 6.8 times more likely to develop knee OA than those in a normal weight range.
- Abnormal structure: Structural abnormalities, such as leg length discrepancies among the joint components, improper joint alignment, or congenital conditions, can lead to uneven stress distribution on cartilage. Over time, this abnormal loading can cause cartilage to wear down faster, especially in certain areas of the joint, and cause OA.
Other confirmed risk factors for OA include hormonal imbalances (e.g.: post-menopausal changes), diabetes, smoking, metabolic disorders, and joint overuse.
How Is the Joint Condition Diagnosed?
Because there is no definitive test to diagnose OA and symptoms develop slowly over time, patients can experience a delay of around seven years before receiving an accurate diagnosis.
However, as healthcare technology improves, tests can now help you and your physician determine whether you are experiencing the early symptoms of OA. Because of this, undergoing regular screening tests is of paramount importance.
Some of the diagnostic tools used include:
- Physical examination: Your physician will start your examination with an assessment of your affected joint, checking for tenderness, swelling, redness, instability, weakness, and range of motion.
- X-rays: X-rays are commonly used to create images of the inner aspect of affected joints. They can reveal the narrowing of the joint space, the presence of bone spurs (osteophytes), and changes in the shape of the bone, which can indicate OA.
- CT scan: A CT scan provides detailed cross-sectional images of the joint and surrounding tissues. This can help in detecting joint damage not visible on an X-ray, such as small bone fractures, and can better assess the extent of cartilage loss.
- MRI: Magnetic resonance imaging (MRI) offers high-resolution images of both hard and soft tissues. It’s especially useful for visualizing cartilage, menisci, ligaments, and other joint structures. An MRI can detect early signs of OA, such as cartilage degeneration and changes in the bone, before they become apparent on an X-ray.
Common Treatments
Commonly, OA is managed conservatively through medications, lifestyle modifications, and alternative therapies. Surgery, while it should only be considered as the last resort, may sometimes be recommended when joint damage is extensive, irreversible, and causing disability.
Lifestyle Modifications
Lifestyle and activity modification can improve joint function, slow down the progression of OA, and ultimately reduce the need for medications or surgical interventions. These include:
- Weight management. As seen above, obese and overweight patients have a much higher risk of developing OA, especially in weight-bearing joints like the knee. One study shows that even a 5.1 kg reduction in body weight over 10 years can reduce the risk of OA by 50%.
Adopting a healthy diet and exercising regularly can also ease the load on joints, improve mobility, boost cardiovascular health, and reduce proinflammatory agents like cytokines in the body, ultimately contributing to easier OA management and better overall health.
- Assistive devices. Assistive devices, such as canes, walkers, and orthotic supports, can help distribute weight away from the affected joints, reducing pain and strain and preventing further injury.
- Joint protection techniques. Strategies to minimize stress on the joints during daily activities include using ergonomically designed tools, practicing good posture, and avoiding activities that involve repetitive joint motions. These techniques aim to improve movement patterns to distribute load evenly across the joints and reduce loads on the affected components.
Alternative Therapies
Alternative therapies offer varying results, but they can help you better manage the symptoms of OA, reduce the frequency of pain flare-ups, and decrease the need for medications. These include:
- Acupuncture. Acupuncture involves inserting thin needles into specific points on the body to stimulate nerve endings, release the body’s natural painkillers (endorphins), stimulate blood flow, and in turn, activate healing. A study conducted on 18,000 people shows that patients find acupuncture helpful in managing their symptoms and relieving pain.
- Physical therapy (PT). PT aims to strengthen the muscles around the affected joint, improve flexibility, and reduce pain. PT programs for osteoarthritis often include exercises guided by a specialist to enhance joint stability and range of motion. Other tools your therapist may use include ultrasound, electrical stimulation, and massages.
Medications
Medications are typically recommended for osteoarthritis when non-pharmacological interventions have failed to manage symptoms. They are used to provide temporary pain relief and attempt to slow down the progression of the disease but seldom tackle the root cause of OA. The most commonly recommended medications for OA management include:
NSAIDs
The other day I was evaluating a patient and reviewing the treatment options for their spine condition. After discussing prior treatments, we got to the topic of medications taken for pain relief. She explained that she mainly utilized anti-inflammatory (NSAID) medications and then she told me to hold much she takes and has been for many years…..she takes close to 2 grams (2000 milligrams) on a daily basis which equated to about 9-10 capsules of medication per day. I was shocked, considering she was pre-diabetic and with high blood pressure plus the kicker of it is that her PCP (primary care physician) is ok with this…
Read More About NSAIDsHyaluronic Acid Injection Treatment
Hyaluronic acid injections have several uses, including for the treatment of osteoarthritis, particularly in the context of knee pain. Osteoarthritis is a degenerative joint disease characterized by the breakdown of cartilage in the joints, leading to pain, swelling, and reduced mobility. In this medical application, hyaluronic acid serves as a viscosupplement, aiming to alleviate symptoms and improve joint function.
Read More About Hyaluronic Acid Injection Treatment- Corticosteroids. Corticosteroid injections are often administered directly into the joint to reduce inflammation rapidly. They work by suppressing inflammatory pathways and modulating the body’s immune response, leading to decreased swelling and pain. When used chronically, they can accelerate the degeneration of cartilage and cause severe conditions like adrenal insufficiency.
Surgery
The two main surgical approaches to OA are arthroscopic surgery and joint replacement surgery:
- Arthroscopic surgery: Arthroscopic surgery involves inserting a small camera and surgical instruments into the joint through small incisions. The instruments are used to examine the joint space and then repair issues such as meniscal tears, ligament damage, or cartilage debris.
While less invasive than traditional joint replacement surgery, arthroscopic surgery still carries risks of infection, blood clots, and damage to nearby components of the joint. Additionally, this surgery may not be effective in treating extensive joint damage, requiring patients to undergo revision surgeries.
- Joint replacement surgery. Joint replacement surgery, or arthroplasty, involves removing the damaged components of the joint (like bones, cartilage, and ligaments) to replace them with synthetic elements known as prosthetics. For patients with severe osteoarthritis, this can significantly reduce pain and improve function.
However, this surgery is highly invasive and carries a significant risk of joint damage. Additionally, undergoing surgery does not mean you’ll be able to live pain-free: up to 37% of people undergoing this surgery will continue to experience chronic pain for two years or longer after the operation.
NSAIDs
The other day I was evaluating a patient and reviewing the treatment options for their spine condition. After discussing prior treatments, we got to the topic of medications taken for pain relief. She explained that she mainly utilized anti-inflammatory (NSAID) medications and then she told me to hold much she takes and has been for many years…..she takes close to 2 grams (2000 milligrams) on a daily basis which equated to about 9-10 capsules of medication per day. I was shocked, considering she was pre-diabetic and with high blood pressure plus the kicker of it is that her PCP (primary care physician) is ok with this…
Read More About NSAIDsHyaluronic Acid Injection Treatment
Hyaluronic acid injections have several uses, including for the treatment of osteoarthritis, particularly in the context of knee pain. Osteoarthritis is a degenerative joint disease characterized by the breakdown of cartilage in the joints, leading to pain, swelling, and reduced mobility. In this medical application, hyaluronic acid serves as a viscosupplement, aiming to alleviate symptoms and improve joint function.
Read More About Hyaluronic Acid Injection TreatmentKnee Arthroscopy Surgery
Knee arthroscopy surgery is a very common procedure performed by orthopedic surgeons in an attempt to treat knee pain. Knee arthroscopic surgery is typically performed in an outpatient surgical facility where a small camera is inserted into the knee joint, which allows the surgeon an inside view of one’s knee to operate. It is used both to diagnose and treat a wide variety of knee problems. Utilizing arthroscopic surgery the surgeon can trim any damaged ligaments which are called knee ligament surgery. Alternatively, if ‘damaged’ meniscus is detected, it also is trimmed and or removed, which is called meniscus knee surgery.
Read More About Knee Arthroscopy SurgeryPossible Complications When Left Untreated
If left unaddressed, OA tends to progress over time, which can cause symptoms to become progressively more severe and debilitating. Below are some of the complications of untreated OA.
Chronic Disability
OA is ranked as one of the most disabling conditions, and it’s associated with the most limitations in daily activities like walking and climbing stairs compared to other degenerative conditions. If left untreated, it can lead to:
- Loss of joint function. As OA advances, the degradation of cartilage and the growth of bone spurs lead to a significant reduction in joint function, preventing you from moving your fingers, decreasing dexterity, and making activities like walking or climbing stairs difficult. In 2019, OA accounted for nearly 19 million years lived with disability worldwide.
- Increased pain and stiffness. Pain and stiffness are hallmark symptoms of OA, and worsen alongside the degree of cartilage degeneration. Over time, morning stiffness lasting more than 30 minutes becomes common, and pain may become persistent, even at rest.
Structural Damage
As bones begin to rub against one another, structural damage to the joints and deformities can become severe, preventing mobility and leading to persistent pain.
- Bone damage. Untreated OA leads to substantial structural changes within the joint’s bones. Subchondral bone, the layer just beneath the cartilage, becomes thicker and harder (sclerotic). This results in microfractures and bone cysts, and, as the cartilage breaks down, more direct bone-on-bone contact and subsequent damage may occur.
- Joint deformity. Severe OA can result in visible joint deformities such as bone spurs. Also known as osteophytes, bone spurs can form around the joint margins as the body attempts to repair its structural damage. This can lead to angular deformities, such as varus (bow-leg) or valgus (knock-knee) deformities in the knees, and bony growth around the fingers’ joints, making mobility even more restricted.
The Centeno-Schultz Clinic’s Expertise in Osteoarthritis Treatment
Managing OA often involves patients relying on chronic medication use or living in fear of requiring surgery one day. Both of these aspects can have profound implications, affecting both a patient’s quality of life and mental and physical health.
That’s where the Centeno-Schultz Clinic approach becomes a viable alternative. The clinic stands at the forefront of osteoarthritis treatment through its pioneering approach in regenerative orthopedics, which addresses OA without surgery or drugs.
PRP Injections
Platelet-rich plasma (PRP) therapy is a pillar of osteoarthritis treatment at the Centeno-Schultz Clinic. PRP utilizes a concentrated dose of a patient’s own platelets suspended in plasma to stimulate repair and healing.
These platelets are rich in growth factors that enhance tissue repair and regeneration and when injected into the affected joint, they can promote the body’s ability to heal naturally. PRP injections have been shown to help in treating osteoarthritis in the knee, hands, and hips, offering a promising alternative for those suffering from chronic pain and limited mobility due to osteoarthritis.
Many physicians and other healthcare providers are quick to point out the lack of high-quality research backing these treatments. However, many of these doctors have not looked into the volume of high-quality literature.
We now have close to 150 high-quality, level-1 human research showing PRP superiority in almost every orthopedic condition, such as osteoarthritis, tendon tears, ligament tears, and nerve compressions.
Below are the studies in knee OA alone, with two solo red ones and the rest blue ones, indicating that the study shows the superiority of PRP as it was compared against other standard-of-care treatments like physical therapy, exercise, steroid injections, and surgery.

If you’d like to read them, here is a link to the infographic.
Bone Marrow Concentrate
Bone marrow concentrate (BMC) therapy is another advanced treatment available at CSC. This involves harvesting the patient’s own bone marrow, which contains stem cells, and re-injecting a highly concentrated solution into the affected joint.
BMC utilizes the body’s natural healing mechanisms to support the repair and regeneration of damaged tissues without the severe side effects often associated with traditional therapies.
BMC also has extensive literature supporting its use for knee OA! And continues to grow every year! Read this article to learn more.
Protect Your Joints For A Mobilized Future
With so many people suffering the complications of OA, having to endure the pain, stiffness, and immobility that come with osteoarthritis may seem like the only scenario for many. Fortunately, chronic medication use and surgeries are no longer the only options to manage OA effectively.
The Centeno-Schultz Clinic’s approach, based on regenerative orthopedics, can help you support long-term knee health without invasive procedures or drugs.
Get Your Osteoarthritis Checked by a Professional

Christopher J. Centeno, MD
Christopher J. Centeno, M.D. is an international expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate in orthopedics.
Dr. Centeno is one of the few physicians in the world with extensive experience in the culture expansion of and clinical use of adult bone marrow concentrate to treat orthopedic injuries. His clinic incorporates a variety of revolutionary pain management techniques to bring its broad patient base relief and results. Dr. Centeno treats patients from all over the US who travel to Colorado to undergo innovative, non-surgical treatments. Dr. Centeno has chaired multiple international research-based conferences. He also maintains an active research-based practice, with multiple publications listed in the US National Library of Medicine. Dr. Centeno has also served as editor-in-chief of a medical research journal dedicated to traumatic injury.
Dr. Centeno trained at the Baylor College of Medicine, Texas Medical Center, and the Institute for Rehabilitation Research. He hails from both Florida and New York and currently resides in Boulder, Colorado with his wife and three children.

John Schultz, MD
John R. Schultz M.D. is a national expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate for orthopedic injuries. He is board certified in Anesthesiology and Pain Medicine and underwent fellowship training in both. Dr. Schultz has extensive experience with same day as well as culture expanded bone marrow concentrate and sees patients at the CSC Broomfield, Colorado Clinic, as well the Regenexx Clinic in Grand Cayman. Dr. Schultz emphasis is on the evaluation and treatment of thoracic and cervical disc, facet, nerve, and ligament injuries including the non-surgical treatment of Craniocervical instability (CCI). Dr. Schultz trained at George Washington School of…
Read more
John Pitts, M.D.
Dr. Pitts is originally from Chicago, IL but is a medical graduate of Vanderbilt School of Medicine in Nashville, TN. After Vanderbilt, he completed a residency in Physical Medicine and Rehabilitation (PM&R) at Emory University in Atlanta, GA. The focus of PM&R is the restoration of function and quality of life. In residency, he gained much experience in musculoskeletal medicine, rehabilitation, spine, and sports medicine along with some regenerative medicine. He also gained significant experience in fluoroscopically guided spinal procedures and peripheral injections. However, Dr. Pitts wanted to broaden his skills and treatment options beyond the current typical standards of care.
Read more
Jason Markle, D.O.
Post-residency, Dr. Markle was selected to the Interventional Orthopedic Fellowship program at the Centeno-Schultz Clinic. During his fellowship, he gained significant experience in the new field of Interventional Orthopedics and regenerative medicine, honing his skills in advanced injection techniques into the spine and joints treating patients with autologous, bone marrow concentrate and platelet solutions. Dr. Markle then accepted a full-time attending physician position at the Centeno-Schultz Clinic, where he both treats patients and trains Interventional Orthopedics fellows. Dr. Markle is an active member of the Interventional Orthopedic Foundation and serves as a course instructor, where he trains physicians from around the world.
Read more
Brandon T. Money, D.O., M.S.
Dr. Money is an Indiana native who now proudly calls Colorado home. He attended medical school at Kansas City University and then returned to Indiana to complete a Physical Medicine and Rehabilitation residency program at Indiana University, where he was trained on non-surgical methods to improve health and function as well as rehabilitative care following trauma, stroke, spinal cord injury, brain injury, etc. Dr. Money has been following the ideology behind Centeno-Schultz Clinic and Regenexx since he was in medical school, as he believed there had to be a better way to care for patients than the status quo. The human body has incredible healing capabilities…
Read moreOther Resources for Osteoarthritis
-
Learn Why Your Neck Hurts
Globally, neck pain is estimated to affect 203 million people, making it one of the most common musculoskeletal pains worldwide. It often stems from a combination of factors, such as muscle strain, poor posture, and degenerative disc conditions. This pain can limit movement, disrupt daily life, and, in severe cases, impact overall health. While some…
-
Partial ACL Tear
A partial ACL (anterior cruciate ligament) tear occurs when the ligament in the knee is partially damaged, often leading to instability, pain, and limited range of motion. This injury typically results from sudden stops, pivots, or direct impacts, commonly seen in athletes. Early diagnosis and appropriate management are crucial to preventing further damage and ensuring…
-
The C1 And C2 Vertebrae – What To Know
The C1 and C2 vertebrae, also known as the atlas and axis, are the uppermost bones in the spinal column. They play a crucial role in supporting the skull and enabling head movements. Damage or injury to these vertebrae often leads to pain, limitations to daily activities, and reduced quality of life. Many patients, without…
-
Degenerating Meniscus
Degenerating meniscus is a common issue, particularly in aging populations, that can lead to significant knee pain and impaired mobility. This condition often arises from wear and tear over time, resulting in the breakdown of the meniscal cartilage, which is crucial in cushioning and stabilizing the knee joint. Early detection and appropriate management are key…
-
All You Need to Know about the L4 Vertebra
The L4 vertebra is one of the five vertebrae in the lower back, located just above the sacrum. It plays a crucial role in supporting the upper body’s weight and enabling movement. Injury or degenerative changes that affect the L4 vertebra can lead to chronic pain and mobility issues. Many patients often rely on medications…
-
Back Cracking: The Truth of What’s Actually Happening in Your Body
Back cracking is a phenomenon that many people experience, often eliciting both curiosity and concern. Whether it’s the satisfying pop from a morning stretch or the deliberate twist during a yoga session, the sound and sensation of cracking your back can be oddly gratifying. But what exactly is happening inside your body when you hear…
-
What Is Golfer’s Knee, And What Can I Do About It?
The nature of golf is such that both the backswing and downswing affect the knee. The entire swing takes a little over one second. However, it can exert a force of 4 times the body weight on the front knee and 3 times the weight on the back knee (1). This makes knee injuries just as…
-
10 Best Shoulder Physical Therapy Exercises to Ease the Pain
Physical therapists often recommend specific exercises to alleviate shoulder pain, recognizing their effectiveness in both treating and preventing shoulder issues. These exercises, designed to enhance strength, flexibility, and mobility, can be a key component of a pain management strategy. Moreover, the ability to perform these exercises at home makes them a convenient option for patients…
-
Understanding the Thoracic and Lumbar Spines
The thoracic spine and lumbar spine make up a vital nexus of stability and mobility in the human body. In this exploration, we delve into the biomechanics and complexities that define these regions, unraveling their significance in posture, movement, and overall well-being. Understanding the thoracic and lumbar spine not only illustrates the mechanics of our…
Want to learn more about your condition? Talk to us, and we’ll help you get to your healthy lifestyle.