Spontaneous Osteonecrosis Of The Knee (SONK)
Spontaneous osteonecrosis of the knee, aka SONK, is a condition that causes acute unilateral knee pain. It was first described in 1968 in individuals in their sixth decade of life. SONK develops insidiously, which makes the diagnosis process quite challenging.
However, SONK is a progressive disease and can gradually lead to deterioration of the structures in the knee if left untreated. Keep reading to find out more about SONK, and the possible causes, symptoms, diagnosis, and treatments.
What Is SONK?
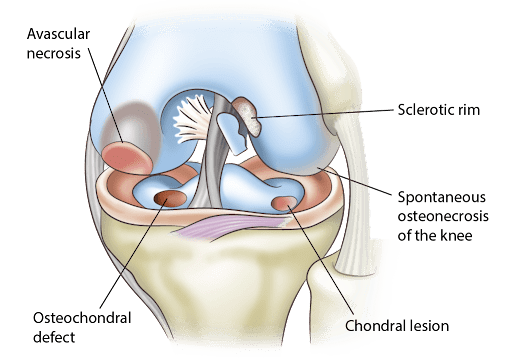
Spontaneous osteonecrosis of the knee is the most common form of primary osteonecrosis in the knee. Osteonecrosis is a condition where blood supply to part of the bone is disrupted, depriving the bone of oxygen and nutrients, ultimately leading to the breakdown of the bone.
The cause of SONK is unknown. The condition usually affects people older than 50. It is ore prevalent in women and those with a history of high exercise levels and osteopenia or osteoporosis (weakened bone).
In contrast, secondary osteonecrosis is destruction of the bone due to a lack of blood supply following arthroscopy of the knee or trauma.
Although the cause of SONK isn’t clear, several theories on how it develops have been suggested. The main theory is that subchondral fractures of the femoral head lead to fluid accumulation of fluid that interrupts the blood supply to the bone, leading to destruction of the bone.
Other theories suggest that there is a vascular injury cause to SONK.
A study in 2019 suggested a strong connection between meniscal tears and spontaneous osteonecrosis of the knee (1). Meniscal tears were found to be present in as many as 50 to 100% of patients with SONK.
According to this systematic review, the extent of medial meniscus extrusion was directly connected to the extent of the SONK lesion as well. Extrusion means the meniscus is unstable and has migrated out of the normal space between the tibia and femur resulting in more stress on the cartilage and bone.
The investigators in the study suggested that disruption of the posterior medial meniscus root causes the meniscus extrusion leading to theincrease tibiofemoral contact pressure.
The augmented pressure can change the biomechanics in the knee. As a result, the femur may sustain subchondral insufficiency fractures, leading to SONK.However, it’s important to remember that there is no consensus about what causes SONK. SONK usually develops gradually over time and, in many cases, occurs spontaneously without a cause – hence the name, spontaneous osteonecrosis of the knee.
Symptoms Of Spontaneous Osteonecrosis Of The Knee
The clinical symptoms of SONK include sudden onset knee pain with joint effusion and tenderness. Usually only one knee joint is involved. Here are some common symptoms of spontaneous osteonecrosis of the knee:
Sudden Onset Of Pain
People with SONK usually have no history of trauma. However, they can often pinpoint when the pain began. Sudden onset of pain most commonly over the area of the medial condyle of the femur is a key symptom of SONK. The pain often limits mobility and may be accompanied by mild swelling. The pain can be with weight bearing and with rest or at night.
Tenderness Around the Knee
Localized tenderness on palpation around the affected knee is a symptom of SONK. This is especially common over the medial area of the knee where osteonecrosis often develops.
Knee Stiffness
Knee stiffness is also a common symptom of SONK. If there is a mild effusion or swelling, then moving the knee can become difficult or painful, affecting the range of motion.
Knee Pain
Knee pain can be caused by many factors. Overuse injuries, direct trauma to the knee and arthritis are the most common causes of knee pain. Damage to the knee structures may cause swelling, scar tissue formation (fibrosis), and loss of function of the joint. Pain is often accompanied by difficulty walking, weakness, and instability. When the knee is overused, the thigh and shin bones (femur and tibia), cartilage, or tendons may experience stress. This leads to pain and discomfort as well as stiffness in the knee. Overuse injuries are common among athletes who participate in sports that involve running, jumping…
Read More About Knee PainReduced Range of Motion in Knees
A knee can feel stiff if there is some swelling in or around the joint or muscle tightness can caused restricted motion This can occur from a problem in the knee joint, such as inflammation, arthritis, or infection, or an injury. The distance and direction that a joint may move are referred to as its range of motion. Various joints in the human body have specific normal ranges set by doctors and therpists. One study, for example, found that a normal knee should be able to bend to between 133 and 153 degrees. A typical knee should also be able to extend fully straight. Limitation of motion occurs when a person range of motion in any limb is reduced below the normal range….
Read More About Reduced Range of Motion in KneesCommon Causes Of Spontaneous Osteonecrosis Of The Knee
The primary causes of spontaneous osteonecrosis of the knee are subchondral fractures of the head of the femur and medial meniscus root tears. They are explained in detail below:
Subchondral Insufficiency Fractures
Subchondral insufficiency fractures are stress fractures that occur below the cartilage. They are commonly seen on the weight bearing surface of the bone. These stress fractures can compromise the blood supply to parts of the bone, which later leads to necrosis of the bone and the potential onset of SONK.
Medial Meniscal Root Tears
Medial meniscal root tears can occur due to specific repetitive movements, such as deep squatting or high intensity sports. The tear leads to the extrusion of the medial meniscus, and this changes how the load is transmitted throughout the knee.Meniscal root tears are so common that they are seen in about 10% of patients who undergo arthroscopy for other reasons. The tears indirectly affect the medial epicondyle of the femur due to the altered biomechanics, which can lead to SONK.
Diagnosing SONK In Patients
Medical professionals use a variety of imaging tests to diagnose SONK. Some of them are listed below:
- Radiography: X-rays can be used to diagnose SONK. Anteroposterior (AP), oblique, and lateral plain X-rays of the knee are first obtained, which can visualize the flattening of the involved condyles. However, X-rays are only useful for the later stages of SONK as they cannot accurately detect early changes in the bone.
- MRI: Magnetic resonance imaging (MRI) is extremely useful for diagnosing SONK in the early stages of the disease. MRIs have an extremely high sensitivity to bone edema, meaning they can visualize bone marrow edema that is localized to the medial femoral condyle. MRIs can also detect if the bone marrow edema extends into the intercondylar notch.
Additionally, an MRI can also identify concurrent meniscal tears that present along with the SONK lesions.
- Bone scintigraphy: Bone scintigraphy is a type of nuclear medicine procedure where small amounts of radioactive material (similar to the contrast commonly used in CTs and MRIs) are injected into the veins. The lesions take up the contrast dye and light up, highlighting the exact area of any SONK lesions and how deep or big they are.
This can also visualize even smaller lesions that may not appear on an MRI. Bone scintigraphy can therefore help with the diagnosis of SONK. However, bone scintigraphy is not as sensitive as MRI, so MRI continues to be the best imaging method to diagnose SONK.
Classification of Spontaneous Osteonecrosis Of The Knee
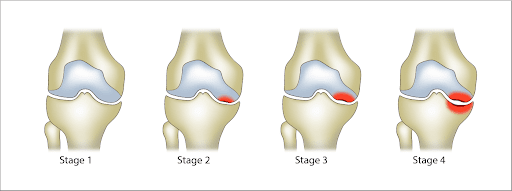
The Koshino staging system was created to categorize the different stages of SONK. There are four distinct stages of SONK, which are based on clinical and radiological findings. They are listed below:
Stage 1: Symptomatic knee with normal findings on X-ray
Stage 2: Presence of condyle flattening and subchondral inflammatory bone lesions without collapse
Stage 3: Extension of inflammatory bone lesions with subchondral collapse
Stage 4: Degenerative changes with formation of osteophytes and osteosclerosisThe best treatment for SONK depends on the stage of the condition. The first two stages can be treated with conservative therapy while the last two stages need surgical measures.
Common Treatments For Spontaneous Osteonecrosis Of The Knee
NSAIDs
The other day I was evaluating a patient and reviewing the treatment options for their spine condition. After discussing prior treatments, we got to the topic of medications taken for pain relief. She explained that she mainly utilized anti-inflammatory (NSAID) medications and then she told me to hold much she takes and has been for many years…..she takes close to 2 grams (2000 milligrams) on a daily basis which equated to about 9-10 capsules of medication per day. I was shocked, considering she was pre-diabetic and with high blood pressure plus the kicker of it is that her PCP (primary care physician) is ok with this…
Read More About NSAIDsConservative Therapy
Non-surgical, conservative therapy for SONK includes home remedies that do not require a prescription. Conservative therapies are helpful for those in the initial stages of SONK and can be a great alternative to surgery. Some of the common conservative options for SONK are listed below:
- Protected weight bearing: Protected weight bearing is an instruction given to patients with SONK. Protected weight bearing means bearing weight with the help of a gait aid. This can include using a cane, crutches, or a walker, which can help prevent exacerbating the SONK lesions.
- Wearing lateral wedge insoles: Lateral wedge insoles are shoe inserts that can reduce knee pain from SONK. Insoles help by reducing the load on the medial knee. There are various insole designs with different degrees, namely higher than 0°, lower than 5°, higher than 5°, equal to or lower than 9°, and higher than 9°.
You can ask your doctor which one is best for you. By reducing the load on the knee using an insole, you can prevent the osteonecrosis from worsening and allow the lesions to heal.
- Strengthening exercises: Physical therapy can help build the femoral muscles using passive and active exercises. Depending on the severity and cause of the SONK, these exercises may include straight leg raises, knee bends, hamstring stretches, and other exercises that can help build the muscles that support the knee.
- Extracorporeal shockwave therapy (ESWT): ESWT is a type of therapy where an electromagnetic source generates a shockwave. This occurs by passing an electric current through a coil which produces a magnetic field. Waves are created from this, which can be directed to a specific diseased area using a lens.
ESWT modifies the changes in cartilage and subchondral bone that occur due to osteoarthritis and other inflammatory conditions in the knee joint. This therapy can be used to treat the lesions in the early stages of osteonecrosis.
- Pulsed electromagnetic field (PEMF) therapy: PEMF therapy uses magnetic energy to send electromagnetic waves in pulses across the knee. These waves can reduce the size of any necrotic lesions and also reduce the area where the lesions have affected the bone marrow of the femur.
- Hyperbaric oxygen: Hyperbaric oxygen therapy involves exposing a tissue to a high concentration of oxygen. For SONK, this therapy can be a good alternative to surgery as it improves the oxygen and reperfuses the necrosed area. This helps to increase perfusion to the lesions and promotes faster healing.
- Bisphosphonates: Bisphosphonates are a class of drugs that slow down bone loss. They work by binding to bone that is reabsorbed by osteoclasts (cells that break down bone). Once inside the osteoclast cell, bisphosphonates trigger the self-programmed death of the osteoclast, thereby preventing the reabsorption of bone.
This is very helpful for SONK as it can prevent subchondral collapse. By preventing the resorption of the necrotic area in the condyles, it can prevent further osteonecrosis.
- Knee Braces And Supports: Knee braces and supports are a conservative treatment option for SONK. Knee braces and knee supports (e.g., knee sleeves) are designed to protect the knee by reducing unwanted flexion, abduction, and adduction of the knee (2).
Studies have shown that knee braces can help reduce excessive knee movement and protect the knee from further injury (3). In one study, the knee brace reduced knee adduction and pain in participants, and also improved function of the knee joint when the brace was used for a long period of time.
Knee braces and supports are usually made of non-latex neoprene material and are designed to be easily pulled on or secured with Velcro straps. Some knee braces have metal hinges built into them to stabilize the knee, helping to prevent the SONK lesions from progressing and allowing time for the knee to heal.
Regenerative treatments:
If common conservative treatments are not helping then there are still some non surgical regenerative injections that can help.
At the Centeno Schultz Clinic we are the world experts in using regenerative injection therapies to treat orthopedic injuries. These treatments can help the body heal from injury without the associated risks of medication and invasive surgeries.
- PRP (platelet rich plasma)
PRP is made from taking a person’s whole blood and processing it to separate the different layers. The layers with platelets can be isolated and concentrated. The platelets have many growth factors (cytokines, proteins, exosomes, etc) that can help with tissue healing.
Most PRP procedures performed currently are autologous, meaning that that come from and go back into the same patient being treated. These injections are safe and used for a variety of orthopedic problems. Precise injections of PRP into the bone can aid in healing.
There is published research that shows PRP can help knee bones heal (5) and osteonecrosis (6). PRP can also be used to help the associated knee meniscus tears, mild to moderate arthritis and knee ligament injuries. There are many randomized controlled trials that support the use of PRP for knee problems (A Research Update on PRP to Treat Knee Arthritis – Regenexx).
- Bone marrow concentrate (BMAC) containing stem cells.
SImilarly to PRP, bone marrow can be collected from a patient, its cellular component isolated and concentrated, then injected to treat musculoskeletal problems. Bone marrow is most commonly obtained from the posterior iliac crest (back of the large hip bone). This is a safe and more comfortable procedure than it sounds like.
The BMAC contains stem cells which are believed to be the most important cells involved with healing. There are many published studies showing injections of BMAC into the knee bone for necrosis and bone injuries due to arthritis can be helpful (7-10).
Surgery
There are several surgical options for the management of SONK. Surgery is usually only considered for cases of extensive SONK, or when conservative treatment has failed. Surgical options for SONK include:
- Arthroplasty
Unicompartmental knee arthroplasty (UKA) or total knee arthroplasty (TKA) are both good options for treating SONK. In these surgeries, the knee joint is replaced with a prosthesis. This helps as the affected bone is replaced by a prosthesis which aids in the movement of the joint and reduces pain.
- Core decompression
In this surgery, the surgeon drills the area of osteonecrosis which decreases pressure on the bone surface and allows new channels for blood vessels to nourish the the bone to heal.
- High Tibial Osteotomy
This is a surgical procedure where the surgeon realigns the joint. This is done by wedging open the upper portion of the tibia which reconfigures the knee joint and changes the biomechanics of the knee.
As a result, the surgery helps shift load away from the damaged tissue. This is not a permanent fix as it will only last about ten years. However, it helps to buy time to decide on other treatment options, such as a total knee replacement procedure.
- Osteochondral transplantation
Osteochondral transplantation is a two-stage procedure where chondrocytes or cartilage cells are implanted, followed by bone grafting. This type of surgery can help repair hyaline cartilage and subchondral bone. It is usually only used for large SONK lesions.
Autologous chondrocyte implantation and mesenchymal stem cells are used together for large cartilage defects.
Recovering From SONK
Recovery from SONK depends on the stage of the condition and the treatments used. Here are some key points about how long it will take to recover.
- Conservative therapy can take about 6-12 weeks before the osteonecrosis begins to heal.
- Conversely, 30 sessions of hyperbaric oxygen are needed for complete resolution of the SONK lesions, while electromagnetic radiation can take about 6 months to work.
- Surgery for SONK can take about 3-6 months, which is then usually followed by a period of physical therapy.
The Prognosis Of SONK
The prognosis of SONK depends entirely on the size of the lesion. The larger the lesion, the higher the risk of osteoarthritis. If about 40% of the joint surface is affected, there is a likelihood of developing osteoarthritis in 15 years (4).
The good thing is, if this is diagnosed early, it can be treated successfully using non-operative measures. However, if symptoms are left undiagnosed, SONK can progress to end-stage osteoarthritis.
When the traditional measures of rest, physical therapy, medications and supplements fail, then PRP and bone marrow concentrate can be a great alternative to surgery to help the kneeheal, reducing pain, keeping the natural anatomy, and reducing the risk for future surgeries. Have you been diagnosed with SONK or are you experiencing unilateral knee pain that hasn’t been diagnosed yet? Schedule an appointment with one of our board-certified doctors today and find out what to do next. We are world experts at helping the body heal itself through regenerative measures for orthopedic problems.

Christopher J. Centeno, MD
Christopher J. Centeno, M.D. is an international expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate in orthopedics.
Dr. Centeno is one of the few physicians in the world with extensive experience in the culture expansion of and clinical use of adult bone marrow concentrate to treat orthopedic injuries. His clinic incorporates a variety of revolutionary pain management techniques to bring its broad patient base relief and results. Dr. Centeno treats patients from all over the US who travel to Colorado to undergo innovative, non-surgical treatments. Dr. Centeno has chaired multiple international research-based conferences. He also maintains an active research-based practice, with multiple publications listed in the US National Library of Medicine. Dr. Centeno has also served as editor-in-chief of a medical research journal dedicated to traumatic injury.
Dr. Centeno trained at the Baylor College of Medicine, Texas Medical Center, and the Institute for Rehabilitation Research. He hails from both Florida and New York and currently resides in Boulder, Colorado with his wife and three children.

John Schultz, MD
John R. Schultz M.D. is a national expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate for orthopedic injuries. He is board certified in Anesthesiology and Pain Medicine and underwent fellowship training in both. Dr. Schultz has extensive experience with same day as well as culture expanded bone marrow concentrate and sees patients at the CSC Broomfield, Colorado Clinic, as well the Regenexx Clinic in Grand Cayman. Dr. Schultz emphasis is on the evaluation and treatment of thoracic and cervical disc, facet, nerve, and ligament injuries including the non-surgical treatment of Craniocervical instability (CCI). Dr. Schultz trained at George Washington School of…
Read more
John Pitts, M.D.
Dr. Pitts is originally from Chicago, IL but is a medical graduate of Vanderbilt School of Medicine in Nashville, TN. After Vanderbilt, he completed a residency in Physical Medicine and Rehabilitation (PM&R) at Emory University in Atlanta, GA. The focus of PM&R is the restoration of function and quality of life. In residency, he gained much experience in musculoskeletal medicine, rehabilitation, spine, and sports medicine along with some regenerative medicine. He also gained significant experience in fluoroscopically guided spinal procedures and peripheral injections. However, Dr. Pitts wanted to broaden his skills and treatment options beyond the current typical standards of care.
Read more
Jason Markle, D.O.
Post-residency, Dr. Markle was selected to the Interventional Orthopedic Fellowship program at the Centeno-Schultz Clinic. During his fellowship, he gained significant experience in the new field of Interventional Orthopedics and regenerative medicine, honing his skills in advanced injection techniques into the spine and joints treating patients with autologous, bone marrow concentrate and platelet solutions. Dr. Markle then accepted a full-time attending physician position at the Centeno-Schultz Clinic, where he both treats patients and trains Interventional Orthopedics fellows. Dr. Markle is an active member of the Interventional Orthopedic Foundation and serves as a course instructor, where he trains physicians from around the world.
Read more
Brandon T. Money, D.O., M.S.
Dr. Money is an Indiana native who now proudly calls Colorado home. He attended medical school at Kansas City University and then returned to Indiana to complete a Physical Medicine and Rehabilitation residency program at Indiana University, where he was trained on non-surgical methods to improve health and function as well as rehabilitative care following trauma, stroke, spinal cord injury, brain injury, etc. Dr. Money has been following the ideology behind Centeno-Schultz Clinic and Regenexx since he was in medical school, as he believed there had to be a better way to care for patients than the status quo. The human body has incredible healing capabilities…
Read moreReferences
- Hussain ZB, Chahla J, Mandelbaum BR, Gomoll AH, LaPrade RF. The Role of Meniscal Tears in Spontaneous Osteonecrosis of the Knee: A Systematic Review of Suspected Etiology and a Call to Revisit Nomenclature. Am J Sports Med. 2019;47(2):501-507. doi:10.1177/0363546517743734
- Moon J, Kim H, Lee J, Panday SB. Effect of wearing a knee brace or sleeve on the knee joint and anterior cruciate ligament force during drop jumps: A clinical intervention study. Knee. 2018;25(6):1009-1015. doi:10.1016/j.knee.2018.07.017
- Baghaei Roodsari R, Esteki A, Aminian G, et al. The effect of orthotic devices on knee adduction moment, pain and function in medial compartment knee osteoarthritis: a literature review. Disabil Rehabil Assist Technol. 2017;12(5):441-449. doi:10.3109/17483107.2016.1151952
- Juréus J, Lindstrand A, Geijer M, Robertsson O, Tägil M. The natural course of spontaneous osteonecrosis of the knee (SPONK): a 1- to 27-year follow-up of forty patients. Acta Orthop. 2013 Aug;84(4):410-4.
- Sánchez M, Delgado D, Pompei O, et al. Treating Severe Knee Osteoarthritis with Combination of Intra-Osseous and Intra-Articular Infiltrations of Platelet-Rich Plasma: An Observational Study. Cartilage. 2019;10(2):245‐253. doi:10.1177/1947603518756462
- Guadilla J, Fiz N, Andia I, Sánchez M. Arthroscopic management and platelet-rich plasma therapy for avascular necrosis of the hip. Knee Surg Sports Traumatol Arthrosc. 2012 Feb;20(2):393-8. doi: 10.1007/s00167-011-1587-9. Epub 2011 Jun 22. PMID: 21695463.
- Hernigou, P., Auregan, J. C., Dubory, A., Flouzat-Lachaniette, C. H., Chevallier, N., & Rouard, H. (2018). Subchondral stem cell therapy versus contralateral total knee arthroplasty for osteoarthritis following secondary osteonecrosis of the knee. International Orthopaedics. doi:10.1007/s00264-018-3916-9
- Hernigou, P., Auregan, J. C., Dubory, A., Flouzat-Lachaniette, C. H., Chevallier, N., & Rouard, H. (2018). Subchondral stem cell therapy versus contralateral total knee arthroplasty for osteoarthritis following secondary osteonecrosis of the knee. International Orthopaedics. doi:10.1007/s00264-018-3916-9
- Kasik CS, Martinkovich S, Mosier B, Akhavan S. Short-Term Outcomes for the Biologic Treatment of Bone Marrow Edema of the Knee Using Bone Marrow Aspirate Concentrate and Injectable Demineralized Bone Matrix. Arthrosc Sports Med Rehabil. 2019;1(1):e7-e14. Published 2019 Aug 26. doi:10.1016/j.asmr.2019.07.001
- Rackwitz L, Eden L, Reppenhagen S, Reichert JC, Jakob F, Walles H, Pullig O, Tuan RS, Rudert M, Nöth U. Stem cell- and growth factor-based regenerative therapies for avascular necrosis of the femoral head. Stem Cell Res Ther. 2012 Feb 22;3(1):7. doi: 10.1186/scrt98. PMID: 22356811; PMCID: PMC3340551.