Spondylolisthesis
Causes, Symptoms, Treatment, & Other Resources
How bad is spondylolisthesis surgery recovery? Let’s review what spondylolisthesis is, and what can be done.
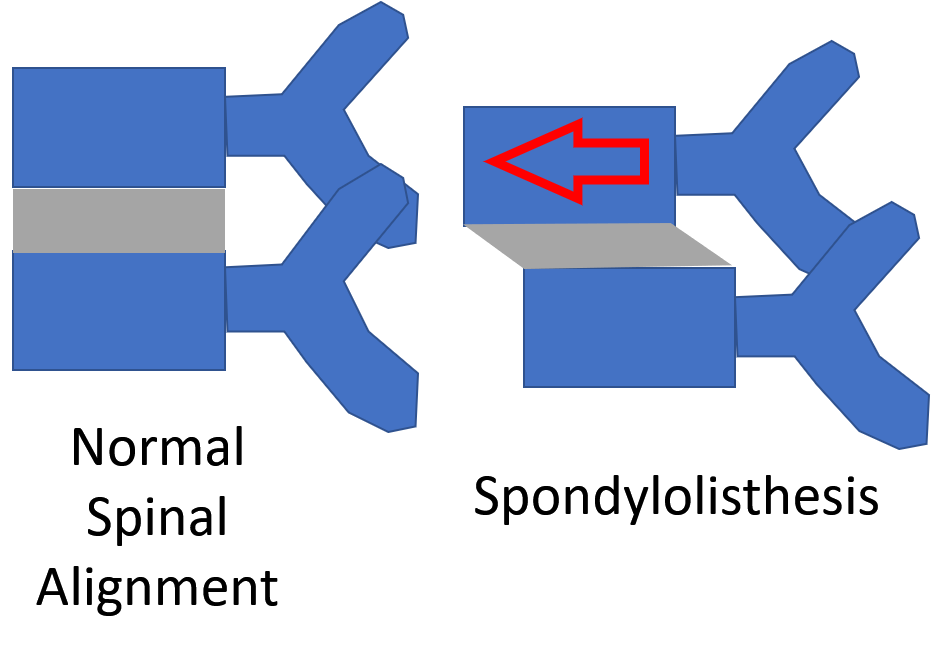
What Is Spondylolisthesis?
Spondylolisthesis means that one vertebra is slipping forward or backwards on another. This causes the hole where the nerve exits (foramen) to get smaller (also called foraminal stenosis). It also causes more wear and tear on the facet joint which can lead to arthritis or what’s called “facet hypertrophy”.
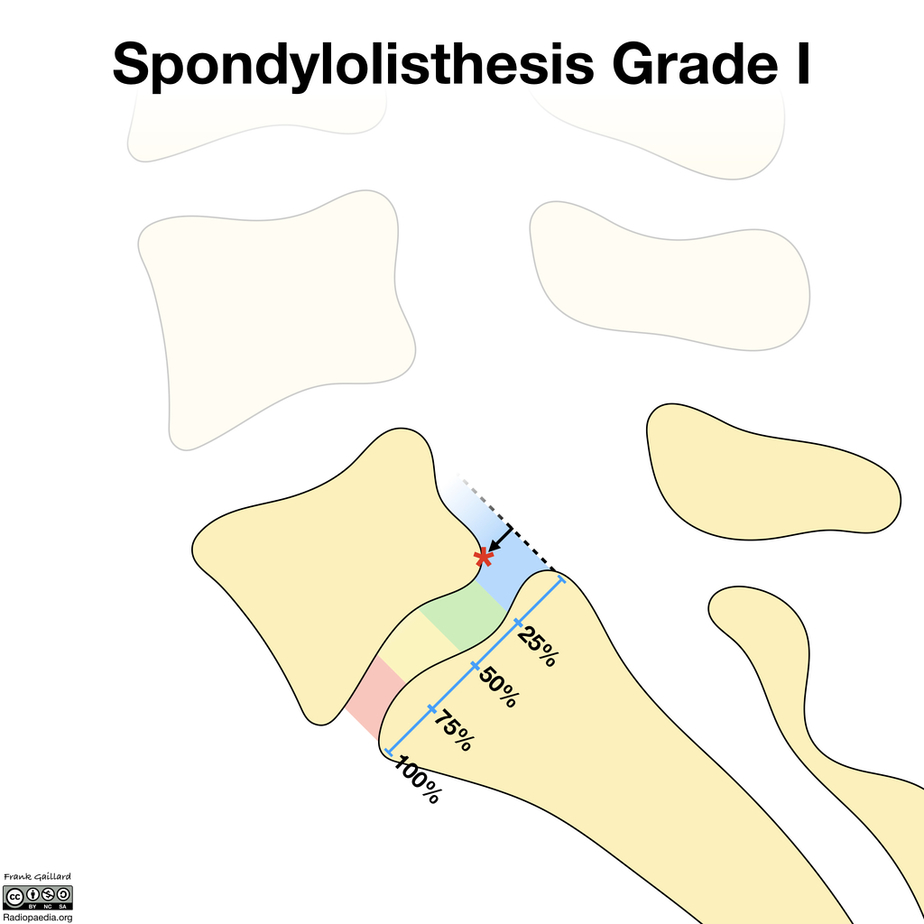
The amount of slippage is graded 1-4, with grade 1 meaning that the one vertebra has slipped up to 25% on the other vertebra. Grade 2 means that one bone has slipped from 25-50% with higher grades indicating more slippage. The vast majority of patients are grade 1 to 2.
What Causes It?
What causes this to happen? Some people are born with bones not properly connected (congenital spondylolisthesis), but most just have wear and tear arthritis which causes one vertebra to begin to shift (degenerative spondylolisthesis). When the bone isn’t connected this is also called spondylolysis and this issue is more common in men while degenerative spondylolisthesis is more common in women (1).
Symptoms of Spondylolisthesis
Spondylolisthesis may not have any symptoms. Some people have it without realizing it. If you do, lower back discomfort is usually the primary symptom. The discomfort might extend down your legs and into your buttocks. You could also get:
- Back stiffness.
- Back pain.
- Difficulty walking or standing for lengthy periods of time.
- Pain when bending over.
- Numbness, weakness, or tingling in the foot, hamstrings, calves, knees, and legs.
Big Toe Numbness
Believe it or not, one of those significant issues that can present as numbness stems from the low back. In the lumbar spine, the nerve that exits the spine at the L5 level branches down through the hip, thigh, knee, lower leg, and, yes, all the way into the foot and toes. So a pinched or irritated nerve at that L5 level in the back can create problems, such as pain, numbness, tingling, and so on, anywhere along the nerve branch. So what can irritate the L5 spinal nerve? The list is long, but it includes disc issues, such as herniated…
Read More About Big Toe NumbnessKnee Buckling
Knees can buckle, causing a sensation of one or both knees giving out that affects nearly 17% of adults. The knees are regarded to be one of the most essential (and biggest) joints in the human body because they play significant roles in basic activities such as walking and sitting. When our knees begin to feel unstable, weak, or begin giving out, it is easy to become stressed since we rely so heavily on them for movement. The knee can become stable from numerous types of injuries. The knee is kept stable by the following structures: Tendons attach the leg muscles…
Read More About Knee BucklingLeg Feels Disconnected
So what exactly causes the leg to feel disconnected? The hip joint is the connection point between the leg and the rest of the body. The femur in the leg and the acetabulum in the pelvis create the hip joint. So if the left SI joint, for example, in the back and the symphysis pubis joint in the front becomes unstable due to loose supporting ligaments, then the left leg, which is connected between the two joints, is likely to also feel a bit disconnected. Likewise, if the right SI joint were unstable, then the right leg might feel disconnected. How This Patient’s “Disconnected” Leg Was Fixed Despite “leg feels…
Read More About Leg Feels DisconnectedLeg Gives Out
Have you ever been walking and your leg gives out? It can be both surprising and alarming What would cause your leg to give out? Can sciatica cause your leg to give out? How do you treat weak legs? Let’s dig in.Weakness in the leg can arise from three principal sources: nerve problems, muscle weakness, and SI joint dysfunction. Weakness in the legs may indicate a significant nerve problem. In many cases, it may be the first indication of a nerve problem. There are three common causes of nerve injury: low back disorders, nerve compression as it descends down into the hip, thigh, and shin and medical conditions such as diabetes…
Read More About Leg Gives OutLower Back Pain When Sitting
After a long day on your feet sitting down is supposed to be way to relaxing. Unfortunately for some sitting for any length of time can be painful. Most people experience low back pain at some point in their life. The lifetime prevalence of low back pain is 85% (1). Let’s take a deeper look at the different types of pain and causes of low back pain when sitting. Pain can present in many different ways. It can be intermitent or constant. The quality of the low back pain can also vary depending upon the actual source of injury. Common examples include: Sharp and Stabbing, Dull and Aching, Throbbing/ Pulsating, Pins and Needles, Burning, Electrical
Read More About Lower Back Pain When SittingLower Back Pain When Standing
When you’re seated, the facet joints in your lower back are in an open and slightly flexed position. When you stand up, these joints compress. If they are painful or have arthritis, you’ll have pain as you stand up because this puts pressure on the painful joints. In addition, if there is any type of movement of one vertebra forward on another (called spondylolisthesis), then this shift will have occurred as you sit. This is called degenerative spondylolisthesis. When you get back up, the vertebrae will come back into position after a few seconds, leading to that awkward “walk it out period” that starts out painful and ends up more normal.
Read More About Lower Back Pain When StandingSI Joint Pain
The SI Joint is an important joint in the lower back that can cause pain and dysfunction. Pain is typically one-sided involving the low back and buttock but when severe can radiate down the leg. Each of us has a right and left SI joint. The pelvic ring consists of the two SI Joints and the symphysis pubis. Each is rich in supporting ligaments that provide stability for the joint. SI Joint pain is aggravated by ligament instability and muscle weakness. Physical therapy is the first line of treatment for SI Joint injuries. For best clinical results the stability of the joint and muscle strength must be evaluated and treated…
Read More About SI Joint PainTight Hamstrings & Calves
The hamstrings are a group of muscles in the upper leg. They are located on the backside of the upper leg and are comprised of three muscles: biceps femoris, semitendinosus, and semimembranosus. The calf muscles are located on the backside of the lower leg and are comprised of two muscles: the gastrocnemius and soleus. Tight hamstring and calf muscles can be painful, limiting someone mobility. They also make lower extremity muscles more vulnerable to injuries. Tight hamstrings and calves can arise from different sources which include: medication, muscle and tendon injury, overuse, muscle imbalance, dehydration, poor posture, low back injury…
Read More About Tight Hamstrings & CalvesUpper Back Pain Between The Shoulder Blades
Upper back pain between the shoulder blades is also known as interscapular pain. Fifteen percent of the population suffers from chronic upper back pain. Finding the source of interscapular pain can be tricky because the upper back houses many important structures like the heart, the upper lobes of the lung, the cervical spine, the scapulas, and a dozen or so of muscles and nerves.
Read More About Upper Back Pain Between The Shoulder BladesWeak in Knees
Weakness in the knee can be a symptom of many different knee conditions. Some of the most common causes of weakness in the knee include ligament tears, meniscus tears, and arthritis. Another important but often overlooked cause of knee weakness is irritation or injury of the nerves in the low back. If you are experiencing any type of weakness in your knee for long durations of time (3 weeks), it is important to see a doctor to determine the cause. Some of the most common symptoms of knee weakness include difficulty standing up from a seated position, difficulty walking, climbing or descending stairs…
Read More About Weak in KneesCan You Become Paralyzed from Spondylolisthesis?
One reason patients decide to embark on spondylolisthesis surgery recovery is that they’re told they could become paralyzed if they don’t have immediate surgery. However, it is very unlikely that you will become paralyzed from a prior spinal abnormality like spondylolisthesis, even if you’re in a car crash. For example, patients with spinal stenosis (where the hole for the spinal cord is too small) are often told that if they sustain significant trauma they may become paralyzed hence they need surgery now. However, research has shown that the risks from the surgery are much greater than any risk of paralysis (2).
Treatment Options for Spondylolisthesis
There are various non-surgical therapies available to help you manage and reduce discomfort. The following are among them:
- Rest.
- Physical therapy. You can increase the strength of the muscles surrounding the afflicted region by exercising in a way that minimizes strain on your back and increases mobility.
- Medication. The pain can be managed by any of a number of over-the-counter pain medications, including Tylenol or anti-inflammatory medicines. A doctor may also subscribe muscle relaxers.
- Epidural steroid injections. For patients suffering significant pain or numbness in the back or legs, an epidural steroid injection can reduce inflammation and relieve pain.
- Back brace
- Platelet-rich plasma injection (more specifically, the Perc-FSU procedure)
When conservative care ends, surgery is often the first thing that is called for. However, this shouldn’t be the case. Why? Let’s dig in.
ACDF Surgery
ACDF stands for “anterior cervical discectomy and fusion.” It is a surgical procedure performed on the neck to relieve pressure on the spinal cord or nerve roots caused by a damaged or degenerated disc. During the procedure, the surgeon removes the damaged disc and replaces it with a bone graft or synthetic implant. Metal plates and screws may be used to hold the vertebrae together during the fusion process. ACDF surgery can help relieve symptoms such as neck pain, numbness, tingling, and weakness in the arms or hands caused by nerve compression in the neck. It is a commonly performed procedure…
Read More About ACDF SurgeryCervical Disc Replacement
Cervical disc arthroplasty (CDA), also known as cervical disc replacement, is a surgical procedure used to treat cervical disc disease. The procedure involves removing the damaged or degenerated intervertebral disc in the cervical spine and replacing it with an artificial disc device. CDA is typically performed for patients with symptomatic cervical disc disease, such as disc herniation, degenerative disc disease, or spinal stenosis. The procedure is intended to relieve symptoms such as neck pain, arm pain, and numbness or tingling in the arms or hands. CDA is considered a less invasive and more motion-preserving alternative to traditional cervical spinal fusion surgery…
Read More About Cervical Disc ReplacementCervical Epidural Steroid Injection
The neck pain started out as a dull ache but steadily progressed. It becomes constant and oftentimes keeps you up at night. Turning your head can send an electrical current down your arm. Rest, medications and physical therapy failed to provide much relief. Your doctor referred you to a pain clinic for a Cervical Epidural steroid injection. The injection was performed at an ambulatory surgical center. Unfortunately, the pain is now worse. What is a Cervical Epidural injection? Are there different types of Cervical Epidural injections? What are…
Read More About Cervical Epidural Steroid InjectionCervical Fusion
Cervical Fusion is often recommended when chronic neck pain problems worsen over time. What exactly is it? Cervical Fusion is a major surgery that involves joining one or more of the spinal bones together using screws, bolts, and plates (1). The hardware may be placed in the front (anterior) or the back( posterior) of the Cervical spine. The disc between the spinal bones is often times removed and replaced with a bone graft or a spacer. The neck of composed of 7 boney building blocks that are numbered from 1-7. The letter C is associated with the numbers to designate the Cervical Spine.
Read More About Cervical FusionDisc Replacement Surgery
The surgeon first accesses the spinal column (for example, in the cervical spine, the surgeon would access the spine through an incision in the front of the neck). From here the surgery is quite aggressive as the disc is scraped and chiseled out of the disc space. Pins are screwed into the vertebrae above and below the disc space that will anchor the space in place as the surgeon works. A tool is inserted into the disc space and used to further separate the upper and lower vertebrae, enlarging the space. The vertebrae surfaces within the disc space are prepared…
Read More About Disc Replacement SurgeryL 4/5 Fusion Surgery
Spinal fusion is a major surgery where one or more spinal bones (vertebrae) are fused together using screws, bolts, and or plates. The hardware may be placed in the front (anterior) or the back (posterior) of the spine. The disc between the spinal bones is often times removed and replaced with bone or a spacer. L 4/5 refers to the level of the surgery. There are 5 spinal bones in the low back which are numbered from top to bottom L1, L2, L3, L4, and L5. Sandwiched between each of the spinal bones is a disc. The disc is named for the two spinal bones it is sandwiched between.
Read More About L 4/5 Fusion SurgeryL5 S1 Fusion Surgery
Spinal fusion is a major surgery where one or more spinal bones (vertebrae) are fused together using screws, bolts, and or plates. The hardware may be placed in the front (anterior) or the back (posterior) of the spine. The disc between the spinal bones is often times removed and replaced with bone or a spacer. L5 S1 Fusion refers to the level of the surgery. There are 5 spinal bones in the low back which are numbered from top to bottom L1, L2, L3, L4, and L5. Sandwiched between each of the spinal bones is a disc. The disc is named for the two spinal bones it is sandwiched between.
Read More About L5 S1 Fusion SurgeryNSAIDs
The other day I was evaluating a patient and reviewing the treatment options for their spine condition. After discussing prior treatments, we got to the topic of medications taken for pain relief. She explained that she mainly utilized anti-inflammatory (NSAID) medications and then she told me to hold much she takes and has been for many years…..she takes close to 2 grams (2000 milligrams) on a daily basis which equated to about 9-10 capsules of medication per day. I was shocked, considering she was pre-diabetic and with high blood pressure plus the kicker of it is that her PCP (primary care physician) is ok with this…
Read More About NSAIDsPerc-FSU – Trusted Alternative to Spinal Fusion
The Perc-FSU Procedure is an injection-based treatment that utilizes the patients’ own blood platelets to bring stability to the spine without the need for the rods, nuts, bolts, and hardware of fusion surgery. “Perc” stands for percutaneous, and “FSU” stands for “Functional Spinal Unit,” which means that the spine is treated as one functioning unit. Up and down the spine, the discs, facet joints, ligaments, and muscles that assist in stabilizing the spine are treated with image-guided injections of PRP and Platelet Lysate to help bring stability to the spine as a whole. It is the trusted alternative to spinal fusion.
Read More About Perc-FSU – Trusted Alternative to Spinal FusionPLIF Surgery
PLIF is a specific type of lumbar fusion surgery. It is an acronym that stands for the Posterior Lumbar Interbody Fusion (1). Posterior refers to the approach used by the surgeon. Posterior refers to the backside of the body vs anterior which refers to the front. Lumbar is the section of the spine involved. The spine is divided into cervical, thoracic, and lumbar. Lumbar is your low back. Interbody fusion refers to a specific type of fusion. For example, in interbody fusion, the disc is surgically removed and a bone graft and spacer is inserted between the spinal bones (vertebral bodies). The inserted bone graft is expected…
Read More About PLIF SurgeryThoracic Spine Surgery
Thoracic spine surgery is a major surgery aimed at treating injuries in the thoracic spine. Because of the complex anatomy and close proximity to the heart and lungs, there are significant surgical risks and complications. Surgery on the thoracic spine can take hours and may require deflating the lung in order to gain access to the thoracic injury. Recovery can be lengthy depending upon the specific thoracic spine surgery performed. There are several different types of thoracic spine surgery. The specific thoracic spine performed depends upon the underlying thoracic injury and a symptoms of the patient. For example, a thoracic disc herniation…
Read More About Thoracic Spine SurgeryTransforaminal Lumbar Interbody Fusion (TLIF)
Transforaminal Lumbar Interbody Fusion is a variant of the Posterior Lumbar Interbody Fusion (PLIF) technique described by Cloward in the 1950s. PLIF has been associated with the high incidences of neurological complications, up to 13.6% of permanent neurologic lesions in Barnes’ et al. study, in particular of the traversing nerve root (2,3) This is due to the fact that a great amount of traction on the dural sac is required to implant the interbody fusion devices. Surgeons have transitioned to TLIF in efforts to reduce complication rates. Success rates vary depending on what literature you read and recently all orthopedic surgery literature has come under fire…
Read More About Transforaminal Lumbar Interbody Fusion (TLIF)Is Surgery for Spondylolisthesis Successful?
There different types of surgeries performed for this condition and each has a different spondylolisthesis surgery recovery pathway. First up is fusion, which means that the doctor uses rods and screws to bolt the spine together. The discs, which are usually mobile shock absorbers, are removed and a bone or a spacer device is inserted in that spot. Another option is decompression surgery without fusion, where the doctor will remove bone, parts of the disc, or ligaments to “open up” the area around the spinal nerves.
If you opt for more aggressive spinal fusion surgery, one major decision you’ll have to make is whether to get fusion and opt for a longer recovery. Meaning the decompression is usually performed, but the surgeon can either fuse or not. The research on which is better shows no difference between decompression with or without fusion (9,10). So why is fusion often added? That’s a great question to which there is no easy answer.
Also, realize that the gold standard in medical research is comparing a surgery against a faked procedure known as a sham operation. No such research exists for spondylolisthesis surgery. Meaning we have no high-level research on whether the surgery is more effective than doing nothing.
What Does Spondylolisthesis Surgery Recovery Look Like?
Your spondylolisthesis surgery recovery will be longer starting with spending more time in the hospital (generally a few days) if you have fusion surgery. Fusion patients also need more narcotics for the first two months compared with decompression alone (11). In a worker’s comp setting, only 30-60% of patients who had the fusion surgery returned to full-time work (12).
What are the Complications of a Lumbar Fusion?
There are a several ways in which fusion surgery can fail and here are the categories:
- Non-union (failure of the bones to heal or grow together)
- Loosening or breakage of the hardware (screws, rods, and connectors)
- Pain caused by the hardware
- ASD (Adjacent segment disease)
First, the level being operated on and fused together with bone can fail to heal and this problem is called a non-union. For procedures that need more bone, like a fusion that is posterior-lateral, the non-union rates can be quite high from 26% to 36% (3, 4). The screws or rods can break or cause pain themselves and both common reasons a second surgery is undertaken after an initial fusion. Overall, a bit more than 1 in 10 patients who have a low back fusion require a second surgery to fix a problem with the first operation (5).
Adjacent segment disease (ASD) means that the spinal levels above or below get degenerated due to excessive force on those areas because of the solid fusion (6). At about 24 months after a back fusion, 12% of patients will get ASD (7). In addition, about 2-4% of the patients will get ASD for every year the patient is active after the fusion, so at 5-years after the first operation, up to 1 in 5 patients will get ASD (8). To understand more, watch my video below:
Can Spondylolisthesis Be Cured without Surgery?
I have a grade 1 degenerative spondylolisthesis, so I’m pretty experienced with this one. Have I had a fusion or decompression surgery? Nope. What did I have done?
As discussed, this problem usually happens because of loose ligaments. There are also arthritic facet joints and pinched nerves and weak muscles. Hence, I had the Perc-FSU (Percutaneous-Functional Spinal Unit) procedure where my own blood platelets were concentrated and injected precisely using x-ray guidance into the ligaments, joints, muscles, and around nerves. This allowed me to get more functional with fewer problems and combined with gains from physical therapy, I no longer throw my back out every time I lean forward. My x-rays also look better, no longer showing that pronounced slippage of L5 on S1. See the video below for information on that procedure:
The upshot? Spondylolisthesis surgery recovery can be rough. That’s why I decided to skip the surgery. Instead, I used Regenexx procedures for spine and cervical conditions. However, if you do need surgery, the research is clear that fusion isn’t required.
Doctors Who Assist with Spondylolisthesis

Christopher J. Centeno, MD
Christopher J. Centeno, M.D. is an international expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate in orthopedics.
Dr. Centeno is one of the few physicians in the world with extensive experience in the culture expansion of and clinical use of adult bone marrow concentrate to treat orthopedic injuries. His clinic incorporates a variety of revolutionary pain management techniques to bring its broad patient base relief and results. Dr. Centeno treats patients from all over the US who travel to Colorado to undergo innovative, non-surgical treatments. Dr. Centeno has chaired multiple international research-based conferences. He also maintains an active research-based practice, with multiple publications listed in the US National Library of Medicine. Dr. Centeno has also served as editor-in-chief of a medical research journal dedicated to traumatic injury.
Dr. Centeno trained at the Baylor College of Medicine, Texas Medical Center, and the Institute for Rehabilitation Research. He hails from both Florida and New York and currently resides in Boulder, Colorado with his wife and three children.

John Schultz, MD
John R. Schultz M.D. is a national expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate for orthopedic injuries. He is board certified in Anesthesiology and Pain Medicine and underwent fellowship training in both. Dr. Schultz has extensive experience with same day as well as culture expanded bone marrow concentrate and sees patients at the CSC Broomfield, Colorado Clinic, as well the Regenexx Clinic in Grand Cayman. Dr. Schultz emphasis is on the evaluation and treatment of thoracic and cervical disc, facet, nerve, and ligament injuries including the non-surgical treatment of Craniocervical instability (CCI). Dr. Schultz trained at George Washington School of…
Read more
John Pitts, M.D.
Dr. Pitts is originally from Chicago, IL but is a medical graduate of Vanderbilt School of Medicine in Nashville, TN. After Vanderbilt, he completed a residency in Physical Medicine and Rehabilitation (PM&R) at Emory University in Atlanta, GA. The focus of PM&R is the restoration of function and quality of life. In residency, he gained much experience in musculoskeletal medicine, rehabilitation, spine, and sports medicine along with some regenerative medicine. He also gained significant experience in fluoroscopically guided spinal procedures and peripheral injections. However, Dr. Pitts wanted to broaden his skills and treatment options beyond the current typical standards of care.
Read more
Jason Markle, D.O.
Post-residency, Dr. Markle was selected to the Interventional Orthopedic Fellowship program at the Centeno-Schultz Clinic. During his fellowship, he gained significant experience in the new field of Interventional Orthopedics and regenerative medicine, honing his skills in advanced injection techniques into the spine and joints treating patients with autologous, bone marrow concentrate and platelet solutions. Dr. Markle then accepted a full-time attending physician position at the Centeno-Schultz Clinic, where he both treats patients and trains Interventional Orthopedics fellows. Dr. Markle is an active member of the Interventional Orthopedic Foundation and serves as a course instructor, where he trains physicians from around the world.
Read more
Brandon T. Money, D.O., M.S.
Dr. Money is an Indiana native who now proudly calls Colorado home. He attended medical school at Kansas City University and then returned to Indiana to complete a Physical Medicine and Rehabilitation residency program at Indiana University, where he was trained on non-surgical methods to improve health and function as well as rehabilitative care following trauma, stroke, spinal cord injury, brain injury, etc. Dr. Money has been following the ideology behind Centeno-Schultz Clinic and Regenexx since he was in medical school, as he believed there had to be a better way to care for patients than the status quo. The human body has incredible healing capabilities…
Read moreOther Resources
The Spine Owner’s Manual: How to Avoid Back Pain & Life-Altering Surgery
This e-book from Dr. Chris Centeno focuses on the spine and how it functions within the human musculoskeletal system and the body as a whole. Everything in our bodies works together like a well-tuned symphony to support our well-being, and a strong spine (including all of its component parts, such as spinal nerves, ligaments, muscles, etc.) is critical to complete health.
Using the Regenexx SANS approach, The Spine Owner’s Manual provides a series of tests and clearly defined exercises that you can do on your own to measure and monitor your own spinal health. These musculoskeletal tests will allow you to monitor where your own body might be struggling to maintain proper stability, articulation, symmetry, and neuromuscular function.
Relevant Blog Posts
-
What Happens If You Have Back Pain From Golf?
Back pain is a common complaint among golfers, impacting both amateur enthusiasts and professional athletes. Golf, while seemingly low-impact, involves repetitive, high-intensity movements that can stress the spine and surrounding structures. Understanding the causes, symptoms, and preventative measures for golf-related back pain can help maintain performance and long-term health. Golf And Back Pain The golf…
-
Spinal Fusion Recovery: What to Expect
Navigating spinal fusion recovery can be a daunting prospect, given its impact on daily life and mobility. Understanding what to expect during this process is crucial for individuals undergoing this procedure. In this article, we’ll explore the typical timeline, challenges, and strategies for managing recovery after spinal fusion surgery, providing insights to help individuals prepare…
-
Back Cracking: The Truth of What’s Actually Happening in Your Body
Back cracking is a phenomenon that many people experience, often eliciting both curiosity and concern. Whether it’s the satisfying pop from a morning stretch or the deliberate twist during a yoga session, the sound and sensation of cracking your back can be oddly gratifying. But what exactly is happening inside your body when you hear…
-
Back Fusion
Spinal fusion, also known as back fusion, is a surgical procedure designed to help severe spinal instability that causes severe pain or nerve injuries. It involves permanently connecting two or more vertebrae in your spine to eliminate motion between them. This article will delve into the intricacies of spinal fusion, exploring the reasons behind the…
-
Understanding the Normal Curvature of the Spine
The human spine, a marvel of engineering, is not a straight column but rather a structure with gentle curves. These natural curves are essential for maintaining balance, allowing flexibility, and absorbing the shock of movement. The spine’s curvature plays a critical role in overall health, influencing posture, mobility, and the function of the nervous system. …
-
Spinal Anterior Longitudinal Ligament Function
Have you had a neck injury or whiplash trauma? Do you have neck pain, especially when looking up, and you don’t know the cause? Then you may want to learn about the cervical anterior longitudinal ligament (ALL). Anatomy of the Anterior Longitudinal Ligament The ALL is a strong, wide ligament that runs along the front…
References:
(1) Osti L, Buda M, Del Buono A. Fatty infiltration of the shoulder: diagnosis and reversibility. Muscles Ligaments Tendons J. 2014;3(4):351–354. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3793342/
(2) Murphy, Donald R et al. “Cervical spondylosis with spinal cord encroachment: should preventive surgery be recommended?.” Chiropractic & osteopathy vol. 17 8. 24 Aug. 2009, doi:10.1186/1746-1340-17-8
(3) Herkowitz HN, Kurz LT. Degenerative lumbar spondylolisthesis with spinal stenosis. A prospective study comparing decompression with decompression and intertransverse process arthrodesis. J Bone Joint Surg Am. 1991 Jul; 73(6):802-8. https://www.ncbi.nlm.nih.gov/pubmed/2071615/
(4) Tsutsumimoto T, Shimogata M, Yoshimura Y, Misawa H. Union versus nonunion after posterolateral lumbar fusion: a comparison of long-term surgical outcomes in patients with degenerative lumbar spondylolisthesis. Eur Spine J. 2008;17(8):1107–1112. doi: 10.1007/s00586-008-0695-9
(5) Greiner-Perth R, Boehm H, Allam Y, Elsaghir H, Franke J. Reoperation rate after instrumented posterior lumbar interbody fusion: a report on 1680 cases. Spine (Phila Pa 1976). 2004 Nov 15;29(22):2516-20. https://www.ncbi.nlm.nih.gov/pubmed/15543064
(6) Saavedra-Pozo FM, Deusdara RA, Benzel EC. Adjacent segment disease perspective and review of the literature. Ochsner J. 2014;14(1):78–83. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3963057/
(7) Zhong ZM1 Deviren V, Tay B, Burch S, Berven SH. Adjacent segment disease after instrumented fusion for adult lumbar spondylolisthesis: Incidence and risk factors. Clin Neurol Neurosurg. 2017 May;156:29-34. doi: 10.1016/j.clineuro.2017.02.020.
(8) Tobert DG, Antoci V, Patel SP, Saadat E, Bono CM. Adjacent Segment Disease in the Cervical and Lumbar Spine. Clin Spine Surg. 2017 Apr;30(3):94-101. doi: 10.1097/BSD.0000000000000442.
(9) Försth P, Ólafsson G, Carlsson T, Frost A, Borgström F, Fritzell P, Öhagen P, Michaëlsson K, Sandén B. A Randomized, Controlled Trial of Fusion Surgery for Lumbar Spinal Stenosis. N Engl J Med. 2016 Apr 14;374(15):1413-23. doi: 10.1056/NEJMoa1513721.
(10) Noorian S, Sorensen K, Cho W. A systematic review of clinical outcomes in surgical treatment of adult isthmic spondylolisthesis. Spine J. 2018 Aug;18(8):1441-1454. doi: 10.1016/j.spinee.2018.04.022.
(11) Vail D, Azad TD, O’Connell C, Han SS, Veeravagu A, Ratliff JK. Postoperative Opioid Use, Complications, and Costs in Surgical Management of Lumbar Spondylolisthesis. Spine (Phila Pa 1976). 2018;43(15):1080–1088. doi:10.1097/BRS.0000000000002509
(12) Anderson JT, Haas AR, Percy R, Woods ST, Ahn UM, Ahn NU. Workers’ Compensation, Return to Work, and Lumbar Fusion for Spondylolisthesis. Orthopedics. 2016 Jan-Feb;39(1):e1-8. doi: 10.3928/01477447-20151218-01
If you need stem cell therapy in Denver CO, please gives us a call at 303-429-6448.