TFCC Tear
Causes, Symptoms, Treatments, & Other Resources
What is a TFCC tear and does it need surgery? Can a TFCC heal without surgery? I am a physician who had a TFCC tear diagnosed on MRI. I never got surgery, why? How did I heal this problem? Let’s dig in.
What Is a TFCC Tear?
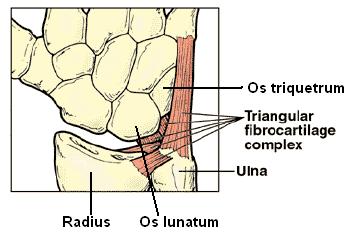
TFCC stands for Triangular Fibrocartilage Complex. It’s basically a triangular-shaped spacer with wrist ligaments that lives on the pinky finger (ulnar) side of your wrist (1). This complex of ligaments stabilizes the bones on that side and adds cushioning. The TFCC can become torn with a fall on an outstretched hand, other trauma, or just wear and tear.
Instability is another feature of TFCC tears (2). The TFCC is part of an extensive group of ligaments that help stabilize both the small wrist bones and the ulna bone. If these become stretched and allow too much movement, this is called instability. These wrists are more likely to get beat up over time due to all of this extra motion.
Causes of TFCC Tears
A TFCC tear can be caused by a variety of issues in two separate locations. The first form of TFCC damage is natural wear, while the latter is usually caused by trauma. Natural wear tears are the most frequent and are generally not seen in youngsters. They become more prevalent with age. Tears from injury can come from:
- Falling on your hand or wrist
- A twisting injury
- A fracture at the end of the radius
Symptoms
The most common indication of a TFCC rupture is wrist pain, which may radiate throughout the entire wrist. You might feel discomfort in your whole wrist or only when you move your wrist or apply pressure to it.
Hands Stiff in the Morning
Hand stiffness can make simple tasks overwhelming. Why are my hands stiff in the morning? What are the treatment options for hand stiff in the morning? Are there new, natural treatment options to treat hands that are stiff in the morning? Our hands are central to virtually everything we do. Stiffness can compromise function and cause pain. What are the causes of hand stiffness in the morning? There are many which include: excessive daily wear and tear, medications that can cause hand swelling and stiffness. Common examples include hormones, calcium channel blockers for high blood pressure, steroids, anti-depressants, and NSAIDs, Diets high in salt, alcohol, and trauma.
Read More About Hands Stiff in the MorningThumb Pain
Thumb pain can be disabling. A general understanding of the anatomy of the wrist and hand helps one understand possible sources of thumb pain. There are many bones in the hand but for this discussion, we will limit it to two major groups: the carpals and metacarpals. The carpals are eight small bones bound in two rows of four bones each. The metacarpals are five in number and make up our palm region. They lie between the carpals and the fingers (phalanges). The joint space between the carpal bones and the proximal base of the metacarpals make up the CMC (carpometacarpal) joint.
Read More About Thumb PainCan a TFCC Tear Heal Without Surgery?
First, you must realize that the TFCC is a bit like a knee meniscus, with a zone that has better blood supply towards the outside of the wrist and a zone with poor blood supply towards the inside. Only tears toward the outside will likely heal on their own, as these have a good blood supply. About 30% of TFCC tears will heal on their own by about 6-months. (11)
Is a TFCC Tear Painful?
A traumatic tear (i.e. due a fall) can be very painful for weeks to months. The average wear and tear degenerative TFCC tear is usually associated with mild to moderate chronic pain on the ulnar side of the wrist. Usually activity with the hand such gripping things or manipulating objects that require force can be painful.
What Is a TFCC Repair?
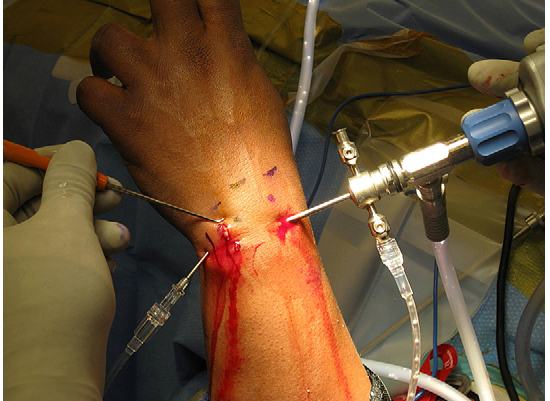
There are two main surgical approaches, debridement and repair. Debridement means cutting out torn pieces of the torn TFCC (4). Repair means sewing a tear together that’s in the outside part of the TFCC that has a better blood supply. Both can be done with open surgery or arthroscopy (using a “scope” as in the picture above). There are three main surgical techniques: inside-out, outside-in, and all-inside.(3) In addition, some surgeons try to shorten the ulna bone, but the research shows that this is likely not needed (9).
Does surgery work? Debridement in one study didn’t produce better grip strength or pain relief (6). In another, only 40% of patients were satisfied (7). In yet another, tears that were due to wear and tear and those patients who had a long ulnar bone were associated with poor surgical results. (12) Having said that other studies have shown good results (8).
As far as repair versus debridement, one is unlikely to better than the other and neither have any high-level research to support that they work well versus a sham procedure (10). Meaning we have no gold standard research that shows us that either TFCC surgery is better than doing nothing. This is interesting as these are common surgeries,
What Is the Recovery Time for Wrist Surgery?
Recovery can take from 6 weeks to 4 months. You will be expected to begin using your fingers as soon as possible and while in a splint to keep them from getting stiff. Icing 3-5 times a day is used to reduce swelling for the first few weeks. As far as nighttime, your wrist will need to be kept elevated while you sleep.
Perc-TFCC Ligamentoplasty – Quicker Recovery for Some Patients
We have been using the Percutaneous TFCC Ligamentoplasty procedure for many years to help reduce recovery and eliminate the need for surgery in patients with TFCC tears with and without instability. This involves a precise ultrasound-guided injection of your own high dose platelet-rich plasma or stem cells into the TFCC and associated ligaments. The goal is to promote healing without the need for surgery.
I’m a big fan of this procedure after having it performed on my own right wrist. One day I was walking out of a convenience store and my shoe ties became accidentally locked and I went down hard on my right hand. After severe pain and barely being able to perform procedures for weeks, an MRI showed a TFCC tear. I also had wrist instability. Instead of surgery, I had the Perc-TFCC Ligamentoplasty procedure and never looked back. I now lift heavy weights without any issue and instead of being in a big cast or brace, I was able to return to work immediately and had an active recovery. Meaning, my recovery period, apart from a few days of wrist aching, was vastly quicker than if I had chosen surgery.
The upshot? TFCC tears can be painful and frustrating and many times surgery is recommended. However, you may be able to avoid invasive surgery with newer injection-based and image-guided procedures.
Doctors Who Treat TFCC Tears

Christopher J. Centeno, MD
Christopher J. Centeno, M.D. is an international expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate in orthopedics.
Dr. Centeno is one of the few physicians in the world with extensive experience in the culture expansion of and clinical use of adult bone marrow concentrate to treat orthopedic injuries. His clinic incorporates a variety of revolutionary pain management techniques to bring its broad patient base relief and results. Dr. Centeno treats patients from all over the US who travel to Colorado to undergo innovative, non-surgical treatments. Dr. Centeno has chaired multiple international research-based conferences. He also maintains an active research-based practice, with multiple publications listed in the US National Library of Medicine. Dr. Centeno has also served as editor-in-chief of a medical research journal dedicated to traumatic injury.
Dr. Centeno trained at the Baylor College of Medicine, Texas Medical Center, and the Institute for Rehabilitation Research. He hails from both Florida and New York and currently resides in Boulder, Colorado with his wife and three children.

John Schultz, MD
John R. Schultz M.D. is a national expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate for orthopedic injuries. He is board certified in Anesthesiology and Pain Medicine and underwent fellowship training in both. Dr. Schultz has extensive experience with same day as well as culture expanded bone marrow concentrate and sees patients at the CSC Broomfield, Colorado Clinic, as well the Regenexx Clinic in Grand Cayman. Dr. Schultz emphasis is on the evaluation and treatment of thoracic and cervical disc, facet, nerve, and ligament injuries including the non-surgical treatment of Craniocervical instability (CCI). Dr. Schultz trained at George Washington School of…
Read more
John Pitts, M.D.
Dr. Pitts is originally from Chicago, IL but is a medical graduate of Vanderbilt School of Medicine in Nashville, TN. After Vanderbilt, he completed a residency in Physical Medicine and Rehabilitation (PM&R) at Emory University in Atlanta, GA. The focus of PM&R is the restoration of function and quality of life. In residency, he gained much experience in musculoskeletal medicine, rehabilitation, spine, and sports medicine along with some regenerative medicine. He also gained significant experience in fluoroscopically guided spinal procedures and peripheral injections. However, Dr. Pitts wanted to broaden his skills and treatment options beyond the current typical standards of care.
Read more
Jason Markle, D.O.
Post-residency, Dr. Markle was selected to the Interventional Orthopedic Fellowship program at the Centeno-Schultz Clinic. During his fellowship, he gained significant experience in the new field of Interventional Orthopedics and regenerative medicine, honing his skills in advanced injection techniques into the spine and joints treating patients with autologous, bone marrow concentrate and platelet solutions. Dr. Markle then accepted a full-time attending physician position at the Centeno-Schultz Clinic, where he both treats patients and trains Interventional Orthopedics fellows. Dr. Markle is an active member of the Interventional Orthopedic Foundation and serves as a course instructor, where he trains physicians from around the world.
Read more
Brandon T. Money, D.O., M.S.
Dr. Money is an Indiana native who now proudly calls Colorado home. He attended medical school at Kansas City University and then returned to Indiana to complete a Physical Medicine and Rehabilitation residency program at Indiana University, where he was trained on non-surgical methods to improve health and function as well as rehabilitative care following trauma, stroke, spinal cord injury, brain injury, etc. Dr. Money has been following the ideology behind Centeno-Schultz Clinic and Regenexx since he was in medical school, as he believed there had to be a better way to care for patients than the status quo. The human body has incredible healing capabilities…
Read moreOther Resources
-
Tendonitis vs Carpal Tunnel: Identifying Important Differences
Tendonitis and carpal tunnel syndrome are two distinct clinical conditions that affect the wrist and hand. Dr. Schultz discusses what tendonitis and carpal tunnel syndrome are, the major causes, common symptoms, treatment options, and the important difference between the two.
-
KT Tape Wrist: Is There A Better Solution?
Wrist ligaments are important for the stability and vitality of the wrist. KT Tape is used extensively for wrist injuries. Dr. Schultz discusses what KT Tape is, its proposed benefits, how to apply and better option for treating wrist ligament injuries.
-
5 Causes of Numbness After Carpal Tunnel Surgery
Carpal Tunnel Syndrome is a medical condition that causes pain and numbness in the hand and fingers. It arises from compression of the median nerve. Dr. Schultz discusses the 5 major causes of numbness after Carpal Tunnel Surgery, their causes, and a novel, nonsurgical treatment option for carpal tunnel syndrome.
-
Will Ulna Shortening Surgery Fix Your Wrist Pain?
Ulnar shortening is one of those procedures that is on our no-no list of surgeries. Unfortunately, however, we occasionally encounter a patient whose orthopedic surgeon has recommended this as a solution to the patient’s problem. The patient, who’s in pain and thinking all other treatment options have been exhausted, is sometimes very close to pulling…
-
Wrist Ligaments: 5 Key Facts You Need to Know
Wrist ligaments provide important stability for the wrist and are receptible to injury. Dr. Schultz discusses 5 key facts you need to know about wrist ligaments, injuries and treatment options.
-
Intersection Syndrome: The Cause Of Your Wrist Pain
Intersection Syndrome is a painful medical condition that involves the backside of the wrist and forearm. Dr. Schultz discusses what is intersection syndrome, what causes it, how it is diagnosed, and treatment options.
References:
(1) Pang EQ, Yao J. Ulnar-sided wrist pain in the athlete (TFCC/DRUJ/ECU). Curr Rev Musculoskelet Med. 2017;10(1):53–61. doi: 10.1007/s12178-017-9384-9
(2) Atzei, A., Luchetti, R., & Garagnani, L. (2017). Classification of ulnar triangular fibrocartilage complex tears. A treatment algorithm for Palmer type IB tears. Journal of Hand Surgery (European Volume), 42(4), 405–414. https://doi.org/10.1177/1753193416687479
(3) Trumble TE, Gilbert M, Vedder N. Arthroscopic repair of the triangular fibrocartilage complex. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 1996;12:588–597. https://www.ncbi.nlm.nih.gov/pubmed/8902134
(4) Osterman AL. Arthroscopic debridement of triangular fibrocartilage complex tears. Arthroscopy. 1990;6:120–124. https://www.ncbi.nlm.nih.gov/pubmed/2363779
(5) Cooney WP, Linscheid RL, Dobyns JH. Triangular fibrocartilage tears. The Journal of Hand Surgery. 1994;19:143–154. https://www.ncbi.nlm.nih.gov/pubmed/8169359
(6) Nishizuka T, Tatebe M, Hirata H, Shinohara T, Yamamoto M, Iwatsuki K. Simple debridement has little useful value on the clinical course of recalcitrant ulnar wrist pain. Bone Joint J. 2013;95-B:1687–1696. https://www.ncbi.nlm.nih.gov/pubmed/24293601
(7) Minami A, Ishikawa J, Suenaga N, Kasashima T. Clinical results of treatment of triangular fibrocartilage complex tears by arthroscopic debridement. J Hand Surg. Am. 1996;21:406–411. https://www.ncbi.nlm.nih.gov/pubmed/19631508
(8) Saito T, Malay S, Chung KC. A Systematic Review of Outcomes after Arthroscopic Débridement for Triangular Fibrocartilage Complex Tear. Plast Reconstr Surg. 2017;140(5):697e–708e. doi: 10.1097/PRS.0000000000003750
(9) Jung KJ, Nho JH2, Kim JH2, Kim BS3, Gong HS4. Triangular Fibrocartilage Complex Repair and Ulna Variance: A Systematic Review. J Hand Surg Asian Pac Vol. 2018 Sep;23(3):313-319. doi: 10.1142/S2424835518300025. can tfcc tear heal without surgery
(10) Andersson JK, Åhlén M, Andernord D. Open versus arthroscopic repair of the triangular fibrocartilage complex: a systematic review. J Exp Orthop. 2018;5(1):6. Published 2018 Mar 13. doi: 10.1186/s40634-018-0120-1
(11) Lee JK, Hwang JY, Lee SY, Kwon BC. What is the Natural History of the Triangular Fibrocartilage Complex Tear Without Distal Radioulnar Joint Instability? Clin Orthop Relat Res. 2019 Feb;477(2):442-449. doi: 10.1097/CORR.0000000000000533.
(12) Roh YH, Hong SW, Gong HS, Baek GH. Prognostic Factors of Arthroscopic Debridement for Central Triangular Fibrocartilage Complex Tears in Adults Younger Than 45 Years: A Retrospective Case Series Analysis. Arthroscopy. 2018 Nov;34(11):2994-2998. doi: 10.1016/j.arthro.2018.05.044.
Related Queries
can tfcc tear heal without surgery