Are Hand Numbness and Tingling Signs of Cervical Radiculopathy?
Get Help With Hand Numbness and Tingling
A 2023 study estimates that pain complaints account for 50-80% of emergency department visits – and up to 50% of those cases relate to what’s known as neuropathic pain, or nerve pain. This refers to paresthesia (or “pins and needles”), burning sensations, and numbness, symptoms that often indicate damage or disease of a somatosensory nerve.
However, these symptoms are often non-specific: they don’t usually point to a specific disease and can indicate many different conditions of the peripheral nervous system, from neuropathy to cervical radiculopathy.
The lack of accurate diagnosis and confusion about what’s causing the symptoms often result in patients being prescribed treatments like generic pain medications and surgeries. These often fail to target the root cause of the disease and expose patients to unnecessary risks and side effects.
Fortunately, thanks to advances in healthcare technologies and pain management research, today’s patients can access non-invasive, non-drug, and non-surgical treatment options that effectively target the root cause of hand numbness and tingling. Discover the Centeno-Schultz Clinic (CSC) approach in this guide.
Conditions That May Cause Tingling in the Hands
Tingling is a symptom often referred to as paresthesia. The word “paresthesia” comes from the Greek words “para” meaning “abnormal” and “aesthesis” meaning “sensation” or “feeling.”
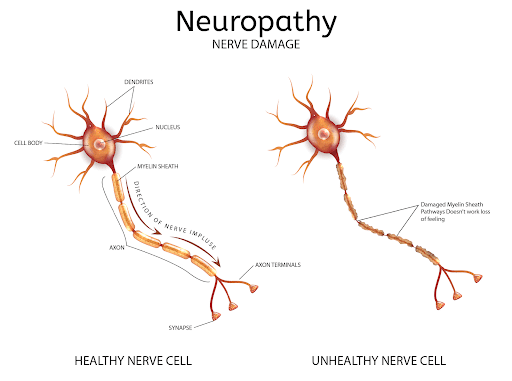
This symptom often emerges as a consequence of damage, lesions, or disease of one or more nerves. When nerves become damaged, their two-way line of communication with the brain is impaired, and signals are unable to reach the central nervous system and be processed as they are supposed to.
This leads to a cascade of symptoms that are often associated with one another or occur together, including:
- Pins and needles sensations
- Numbness
- Burning feeling
- Electric shock sensations
- Weakness in the hand
Although these symptoms are usually associated with damage to a nerve, the cause of the damage may not always be obvious. Common culprits can vary from temporary problems like vitamin deficiencies to progressive conditions like degenerative disc disease, peripheral neuropathy, and cervical radiculopathy.
In-Depth: Neuropathy vs Radiculopathy
Although both conditions affect the functioning of nerves and their capability to transmit signals to the brain, it is important to note the differences between the two:
- Neuropathy refers to damage or dysfunction in the peripheral nerves, resulting in symptoms such as pain, tingling, and muscle weakness. The term stems from the Greek words “neuro,” meaning nerve, and “pathy,” meaning disease. Causes of neuropathy tend to be more systemic or widespread.
- Radiculopathy involves nerve root compression, often due to a herniated disc or bone spur, causing radiating pain, numbness, and weakness. It derives from the Latin term “radicula,” meaning little root, and the Greek “pathy,” meaning disease. Causes of radiculopathy are focal to a specific area somewhere along the nerve that is causing problems.
Whatever the cause, it is important not to underestimate these strange sensations. They may seem mild at first but, if they indicate a progressive underlying disease, they are likely to continue worsening and may eventually lead to reduced function and disability.
It is also important to keep in mind that damage to nerves follows the “dying-back” phenomenon, by which the nerves that are located further from vital organs and the spinal cord (i.e.: the ones in the hands and feet) are the first ones to be affected.
In other words, you may experience tingling and numbness in the hands and feet at first, but as nerve damage progresses, these sensations can begin to spread and intensify.
Below, we’ll look in more detail at the possible causes of hand numbness and tingling.
Vitamin Deficiencies
Vitamin deficiencies, particularly of B vitamins like B12 (cobalamin), B9 (folate), and B6 (pyridoxine), are common and can lead to various neurological problems. These vitamins are crucial for the development, myelination, and function of the central nervous system, as well as for the formation of healthy red blood cells and DNA synthesis.
These deficiencies disrupt the myelin, which is the protective sheath around nerves. Damage to the myelin causes the electrical signals transmitted along the nerves to be slowed down or disrupted. This can lead to muscle weakness, sensory changes – like numbness and tingling – and impairments in bodily functions.
It is estimated that, today, around 3.6% of the population has a vitamin B12 deficiency, while around 11% has sub-optimal levels of Vitamin B6.
Chronic and Systemic Diseases
Chronic and systemic diseases, including diabetes and multiple sclerosis, significantly impact nerve function, even though the mechanisms through which they cause nerve damage may differ.
For example, diabetes, which is prevalent in over 400 million people worldwide, can cause diabetic peripheral neuropathy, a condition where high blood sugar levels damage blood vessels, which become unable to deliver oxygen and nutrients to peripheral nerves, causing the nerves’ death. Studies estimate that around 51% of patients with diabetes also have symptoms of neuropathy.
Similarly, multiple sclerosis (MS), a condition that affects the central nervous system (i.e.: the brain and spinal cord), can result in demyelination. Loss of the myelin around nerves interrupts nerve signal transmission, leading to symptoms ranging from hand numbness to impaired limb function.
Substance Abuse
Substance abuse, particularly of alcohol and certain drugs, is a major cause of neuropathy, with several mechanisms involved. Firstly, chronic alcohol consumption impacts nutrient absorption, leading to nutritional deficiencies (e.g., thiamine, B6, and B12 deficiencies), which, as we’ve seen above, can cause nerve demyelination.
Additionally, these substances, as well as tobacco products, have been seen to have neurotoxic effects – which means that they directly cause the malfunction and death of nerves.
Research estimates that, in the U.S., up to 66% of patients with chronic alcohol use disorder have some form of alcoholic neuropathy.
Toxins
Toxin exposure, including heavy metals like lead, mercury, and arsenic, as well as certain chemicals like pesticides, can have direct toxic effects on the nerves, causing demyelination and the death of nerves in the peripheral nervous system (axonal degeneration).
Although anyone can suffer exposure to these chemicals, the demographics with the highest risk include:
- Industrial and agricultural workers
- Individuals with occupational exposure
- Those in environments with high toxin levels (e.g.: highly polluted areas)
Infections
Contracting certain infections can have a detrimental impact on the nervous system as a whole, due to several mechanisms. Here, we’ll look at some of the most common ones:
- Lyme disease. Caused by the bacterium Borrelia burgdorferi, this disease triggers the immune system’s inflammatory response. In turn, ongoing inflammation can lead to the breakdown of nerve fibers and the surrounding protective tissues.
- HIV. HIV can cause nerve damage through direct invasion of nerve cells by the virus or secondary reactions, including systemic inflammation.
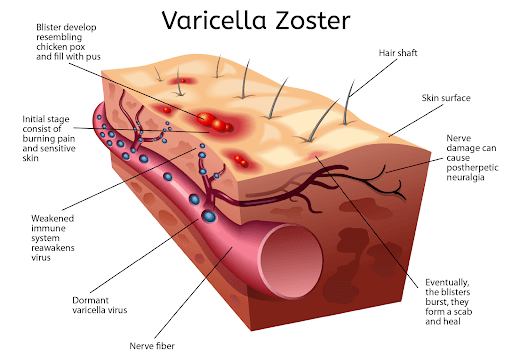
Certain HIV medications (such as didanosine, also known as Videx) have also been seen to have neurotoxic effects, leading to temporary neuropathy and associated symptoms (i.e.: numbness and tingling). It is estimated that 30-60% of people with HIV also have some form of neuropathy. - Herpes zoster (shingles). Herpes zoster, known as shingles, is caused by the reactivation of the varicella-zoster virus and can lead to nerve inflammation and damage. Debilitating post-herpetic neuralgia occurs in 13-40% of shingles cases, and can last for weeks, months, or even years after the infection.
Nerve Entrapment
Nerve entrapment happens when a nerve is compressed in a narrow space and becomes unable to transmit signals to the brain. This can happen because the surrounding tissues become inflamed and swollen, or following trauma injuries (e.g.: a fracture of the wrist that changes the carpal tunnel, which houses the median nerve).
Lifestyle, diseases, and physiological factors – such as joint conditions like osteoarthritis, repetitive movements, being pregnant, or consuming substances that cause inflammation – can all lead to nerve entrapment.
The two most common conditions that may lead to hand numbness and tingling include:
- Carpal tunnel syndrome: This affects the median nerve as it passes through the carpal tunnel at the wrist, causing numbness and tingling in the thumb, index, and middle fingers. It is common in repetitive wrist movements like typing, in pregnant women, and in patients with arthritis and diabetes.
- Cubital tunnel syndrome: Trapping the ulnar nerve at the elbow, this condition results in tingling and numbness in the ring finger and little finger. It is often seen in people who frequently bend their elbows or participate in sports that involve throwing.

Cervical Radiculopathy May Be the Issue
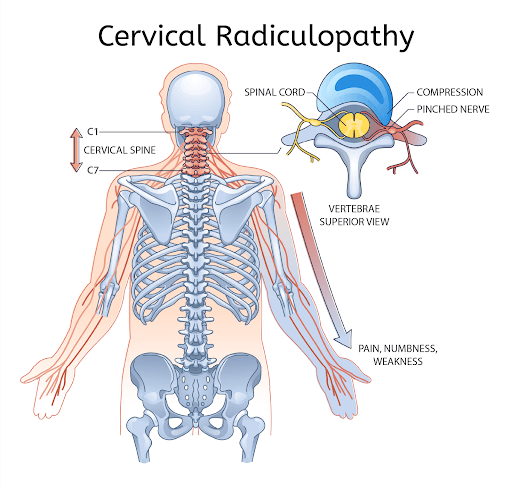
Cervical radiculopathy – or “pinched nerve” – is one of the most common and probable causes of hand tingling and numbness. This condition affects 85 persons per 100,000, and hand numbness and tingling are among its main, best-known symptoms.
Cervical radiculopathy occurs when a nerve root in the cervical spine (neck) becomes compressed or irritated. A nerve root is the initial segment of a nerve, or the segment closest to the spine as the nerve exits the spinal cord. Because the nerve is affected at the root, symptoms will be felt across the length of the nerve, as well as in the areas (e.g.: muscles) innervated by it.
This condition can happen due to herniated discs, bone spurs, or degenerative disc disease, which can cause hard material to protrude from its place and trap, irritate, or inflame the nerves as they exit the spinal cord.
We’ll look at this condition in more detail below.
How Cervical Radiculopathy Causes Hand Numbness and Tingling
As seen above, cervical radiculopathy is a condition that results from the compression of nerve roots in the cervical spine.
The parts of the spine most commonly affected are the C5, C6, and C7 vertebrae. These areas are the exit points for the nerves that are responsible for sensory and motor functions in the shoulder, arm, and hand.
The pinching, irritation, or inflammation of these nerves interrupts the normal transmission of signals, causing the brain to perceive irregular sensations and cause symptoms like tingling or numbness. When motor nerves are affected, patients may also experience loss of muscle and grip strength, as well as involuntary muscle movements such as twitching, cramps, and fasciculations.
Here are some of the mechanisms of action of this cervical radiculopathy – or how it causes numbness and tingling in the hand:
- Nerve root compression: The intervertebral discs, or cervical vertebrae, may herniate, protrude, or slip out of position, causing the nerve root to be pinched or compressed. This phenomenon can also be caused by malformations of the spine and conditions like bone spurs (abnormal bone formations formed by the body in an attempt to restore damaged cartilage), which are often a consequence of joint conditions like arthritis. This pressure disrupts the normal functioning of the nerve.
- Inflammation and ischemia: Compression of a nerve root often leads to inflammation, while swelling and compressed nearby structures (such as blood vessels) may lead to reduced blood flow, a condition known as ischemia. Inflammation can cause damage to the nerves’ myelin, while impaired blood and oxygen flow to the nerves can cause them to die off.
Symptoms such as hand numbness and tingling in cervical radiculopathy arise due to the impaired transmission of nerve signals. Some key indicators that cervical radiculopathy may be at the root of your hand tingling and numbness include:
- The symptoms may not be constant and may only occur intermittently, but they are likely to get worse without treatment.
- Symptoms are often triggered or worsened by certain postures, such as bending the neck forward or holding it in extended positions.
- Activities involving repetitive neck movements – like driving or using a computer – may exacerbate symptoms.
Although cervical radiculopathy may affect anyone at any stage of life, it is more common among those between the ages of 40 and 50. Risk factors include consuming alcohol, having a sedentary lifestyle, smoking tobacco, and having a condition such as diabetes.
Signs That You Should Get Your Hands Checked
Temporary numbness and pins and needles are something we all experience, such as when we fall asleep in an awkward position, due to pressure on the sensory nerves or small blood vessels in the hand or arm. Even persistent tingling in the hands may be harmless and temporary if caused by minor injuries or repetitive stress.
However, if caused by an underlying progressive disease, these symptoms can get worse and, without treatment, lead to impaired hand function and even disability.
Because of this, you should not hesitate to see a doctor if you notice the following signs:
- Numbness and tingling don’t go away within a few hours: If the sensation doesn’t resolve after a few hours, it could indicate nerve damage or compression that needs a professional diagnosis.
- Strange sensations that spread to other parts of the body: When tingling spreads beyond the hands, it might suggest a systemic issue, such as a neurological disorder.
- Paralysis: Sudden paralysis alongside tingling can be a sign of a serious condition such as a stroke. In this case, immediate medical care is vital.
- Confusion: Tingling accompanied by confusion or altered mental state may indicate a transient ischemic attack (TIA) or other severe neurological condition.
- Dizziness: Experiencing dizziness along with tingling might point to cardiovascular problems that may need urgent attention.
- Loss of balance and coordination: These symptoms together can suggest severe issues with the cerebellum or spinal cord.
- Loss of control over bowel or bladder: This can be a sign of cauda equina syndrome, a rare but serious condition that needs immediate treatment to prevent permanent damage.
- Weakness in arms, legs, and feet: Generalized weakness along with hand tingling might indicate a condition affecting the central nervous system such as multiple sclerosis.
- Muscle spasms: Persistent muscle spasms with tingling could be due to electrolyte imbalances or neurological problems that shouldn’t be ignored.
If you also suffer from comorbidities like diabetes, you should immediately seek medical attention, as untreated neuropathy and nerve damage can lead to severe complications, like foot ulcers.
How Doctors Check If the Tingling Sensation Is Spine-Related
Doctors can use various diagnostic tools to determine if hand numbness and tingling are related to cervical radiculopathy. The diagnostic tools below also allow healthcare providers to exclude other conditions and get insights that will then guide treatment planning.
Physical Examination
Physical examination involves several tests to evaluate muscle strength, reflexes, and sensation in the arms and hands. These tests aim to check whether there’s a problem with the nerves in the hands or if the condition is related to degenerative or neurological diseases, like multiple sclerosis.
One of these tests is Spurling’s test, where the doctor gently presses down on the head while it is tilted to one side to check whether certain movements worsen the symptoms. Your doctor may also test the functioning of the nerves in your hand and your grip strength and may use a pinprick or tuning fork to test your arm movement.
Some doctors have the ability to evaluate the peripheral nerves with ultrasounds as well to look for swelling or compression of the nerve.
Assessment of Medical History
The next step involves discussing the onset, duration, and intensity of symptoms like hand numbness and tingling. During this step, you may be asked to answer questions about family history, daily activities, work habits, and any previous injuries or health conditions – like arthritis and diabetes – that may indicate a higher risk of nerve damage.
Blood Tests
Blood tests, while not directly diagnosing cervical radiculopathy, help rule out other conditions that may cause similar symptoms.
Some examples include:
- Tests for blood sugar levels to identify diabetes, which might contribute to peripheral neuropathy.
- Inflammatory markers like ESR (erythrocyte sedimentation rate) and CRP (C-reactive protein) help detect underlying inflammatory or autoimmune conditions, such as rheumatoid arthritis.
- Vitamin deficiencies (especially B12) tests help evaluate whether the cause of hand tingling is connected to nutritional imbalances or malabsorption of nutrients.
Depending on the test results and the conclusions drawn from your physical examination and medical history assessment, your doctor may draw conclusions and make hypotheses that may warrant further tests – like the ones below.
Thyroid Tests
Thyroid tests help rule out thyroid dysfunction as a cause of neuropathy.
Thyroid dysfunction, including both hypothyroidism and hyperthyroidism, can cause nerve damage and, in turn, hand tingling and numbness. When the thyroid produces too little or too much hormone, it affects the metabolism of nerves, leading to their malfunction.
Relevant tests include:
- Thyroid stimulating hormone (TSH): Measures the hormone that stimulates thyroid activity.
- Free T4 (thyroxine): Evaluates the active hormone produced by the thyroid gland.
- Anti-thyroid antibodies: Detects autoimmune thyroid conditions like Hashimoto’s thyroiditis, which may cause neuropathic symptoms due to inflammation.
Toxicology Reports
Toxicology reports analyze exposure to neurotoxic substances that may cause hand numbness and tingling.
These reports involve blood and urine tests to detect heavy metals like lead, mercury, and arsenic, and other toxins like solvents. Your doctor may also recommend a hair analysis to detect long-term exposure to neurotoxic compounds, such as those contained in drugs and pollution.
These tests are essential to determine whether your symptoms are caused by exposure to toxic agents and also to determine what these toxic agents are. Based on this knowledge, your healthcare provider may recommend lifestyle changes (e.g.: quitting smoking or limiting alcohol consumption), assess your work and home environment, and use personal protective equipment when needed.
Examination of Spinal Fluid
The examination of spinal fluid – a test also known as cerebrospinal fluid (CSF) analysis – involves extracting a small sample through a lumbar puncture. This is a procedure also called spinal tap, which involves inserting a needle into the lower back to diagnose conditions affecting the brain and spinal cord.
This test helps diagnose conditions affecting the central nervous system, including infections, inflammation, and potential cancers relating to the brain or spinal cord. For example, elevated white blood cells or proteins in CSF indicate inflammation or infection, which may contribute to nerve root irritation.
Similarly, detecting abnormal cells can pinpoint malignancies (e.g.: tumors, schwannomas, or neurofibromas) impacting spinal nerves and mimicking cervical radiculopathy.
Scans
Scans can help obtain images of the inner aspect of the hand, arm, or cervical spine. They are often recommended to confirm the hypothesis your doctor has formed through the tests above and pinpoint the exact issues. The most commonly used scans include:
- X-rays. X-rays create images of the spine using electromagnetic radiation. They help visualize bone structure and alignment of the spine, helping doctors identify structural anomalies like bone spurs or vertebral degeneration.
- CT scans. CT scans use X-ray technology to generate detailed cross-sectional images of the spine. They offer more detail than X-rays, helping detect more subtle bone abnormalities or fractures that can cause nerve compression.
- Spine magnetic resonance imaging. Spine MRI employs magnetic fields to produce detailed images of spinal soft tissues, such as cartilage, nerve roots, and blood vessels, which wouldn’t be visible through X-rays. These scans help determine whether your symptoms are caused by disk injuries, joint issues, or rarer things like a tumor, mass, or bleed. .
- Neck vessel ultrasound. Ultrasound of neck vessels uses sound waves to visualize blood flow in the carotid arteries and veins. It helps detect vascular issues that might indirectly cause nerve irritation or damage.
- Angiogram. An angiogram involves injecting a contrast dye into blood vessels to visualize blood flow using X-rays. Like the ultrasound tests seen above, it helps identify vascular abnormalities that could compress nerves.
- Nerve Conduction Studies and Electromyography. Nerve conduction studies measure electrical impulses to the nerve to look for changes in the conduction amplitudes or speeds of the nerves. EMG tests measure muscle electrical activity. By inserting fine needles into muscles, this test detects abnormal muscle responses that indicate nerve dysfunction, such as the inability of nerves to carry signals.
Will the Numbness and Tingling Go Away on Their Own?
As we’ve seen above, the likelihood of hand numbness and tingling going away on their own depends on what’s causing your symptoms. If you have experienced a mild injury to the wrist or elbow, or you have inadvertently compressed the nerves in these areas, you may regain your full hand function within hours or days.
However, if the symptoms persist and you are not sure what’s causing them, you should seek an accurate diagnosis. Your doctor will be able to tell you more about what to expect.
For example, temporary irritation of nerves due to improper or repetitive movements can go away in just a few weeks with lifestyle changes, proper posture, exercise, and physical therapy. Similarly, if your symptoms are caused by medications like HIV drugs or chemotherapy, you’ll be able to improve your hand function once your treatment has ended, but this can take time. Research shows that up to 80% of early-stage breast cancer patients who develop chemotherapy-induced peripheral neuropathy (CIPN) experience symptoms for 1-3 years after their treatment.
However, for conditions that tend to progress over time – such as cervical radiculopathy – you’ll need to tackle the root cause of your symptoms with adequate treatment plans. Studies show that 85% of those experiencing acute cervical radiculopathy make a full recovery within 8-12 weeks.
Exploring Your Options
Given the advances in healthcare technology and research, most of the causes of hand numbness and tingling can be effectively addressed with ad hoc treatment plans. Nonetheless, when experiencing these symptoms, obtaining an accurate diagnosis, and understanding your treatment options are crucial steps to take.
That’s because without understanding what’s causing your symptoms, you may unnecessarily expose yourself to the risks and side effects of treatments that are ineffective. And, even if you and your doctor have been able to pinpoint the cause of your symptoms, not looking further than conventional treatments can cause you to miss out on less invasive and more efficient alternatives.
Below, you’ll find both traditional and unconventional treatment options worth exploring.
Medications
Pain medications tend to be the go-to option for many patients experiencing tingling and numbness – or burning sensations – in the hand. However, it is important to keep in mind that using these medications in the long term without understanding the cause of your symptoms isn’t just ineffective, it’s also unsafe.
Although medications can mask the pain short-term, they don’t treat the root cause of your condition, unnecessarily exposing you to side effects.
NSAIDs
Non-steroidal anti-inflammatory drugs (NSAIDs) are a common choice for managing cervical radiculopathy symptoms. These drugs, including ibuprofen and naproxen, work by reducing inflammation, thus providing short-lived pain relief. They can be beneficial for alleviating mild to moderate pain and are available over-the-counter or by prescription, making them an accessible option for most patients.
Nonetheless, long-term use of NSAIDs carries risks such as gastrointestinal issues, cardiovascular problems, kidney disease, and addiction. Always consult with a healthcare provider to determine the appropriate dosage and duration, and avoid relying on these medications if you don’t know what’s causing your symptoms.
Steroids
Steroids, often in the form of oral corticosteroids or injections, are the synthetic version of cortisol, a hormone naturally produced by the body, which helps in regulating inflammation. They offer more powerful and longer-lasting anti-inflammatory effects than NSAIDs by reducing inflammation around the affected nerve root.
Nonetheless, research is now showing that these drugs, when taken regularly, can lead to non-neglectable side effects, from adrenal insufficiency (malfunctioning of the glands that produce cortisol) to cartilage damage.
Steroids can also be injected locally around irritated nerves in the neck, shoulder, elbow, wrist or hand. Again these steroid injection only temporarily help inflammation and pain but they still have the potential side effects above as well as the risk of local tissue injury.
Surgical Options
Surgical options should always be seen as the last resort – but they may become necessary when non-surgical treatments fail to alleviate symptoms or the condition severely impacts life quality.
Depending on what’s causing your symptoms, your doctor may recommend one of several procedures to decompress nerves if your symptoms are caused by cervical radiculopathy. These include:
- ADR. Artificial disc replacement (ADR) involves replacing a damaged disc in the spine with an artificial one. The synthetic disc is designed to maintain flexibility and normal motion in the spine while correcting protruding surfaces that are pressing on nearby nerves.
- ACDF. Anterior cervical discectomy and fusion (ACDF) involves removing a damaged disc and fusing the adjacent vertebrae to stabilize the spine. It’s usually an option recommended for patients with severe disc degeneration or multiple affected discs.
Surgery always carries risks such as infection, bleeding, or nerve damage. Additionally, success rates vary, and, even if offering symptom improvement, they may not fully restore function, causing patients to require additional interventions.
Non-Surgical Options
Non-surgical treatments can provide effective relief for cervical radiculopathy without the risks associated with surgery and the common side effects of medications like NSAIDs and corticosteroid injections. At the Centeno-Schultz Clinic, a leading institution in regenerative orthopedics, these options include advanced techniques like platelet-rich plasma (PRP), platelet lysate (PL) and bone marrow concentrate (BMC) containing stem cells treatments
PRP involves using a patient’s own blood to accelerate healing. Blood is processed to concentrate platelets, the blood components that promote healing by releasing growth factors and bioactive proteins to repair tissues. The solution of concentrated platelets is then injected into the affected area. This promotes tissue repair and reduces inflammation.
PL is a specialized PRP product that requires a specialized lab and staff that is rare to find, but present at the Centeno Schultz Clinic. It involves the same processing as PRP, but additional steps are taken to lyse or burst open the platelets for an immediate release of growth factors. These growth factors are particularly beneficial around nerves and cause less inflammation. A combination of PRP and PL is typically used to treat cervical radiculopathy at the Centeno Schultz Clinic.
PRP is particularly recommended for those seeking a non-surgical solution with minimal downtime.
At CSC, PRP for cervical radiculopathy is used in combination with a whole range of therapies, including physical therapy, lifestyle modifications, and other non-invasive interventions. These approaches are integrated to create a comprehensive treatment plan aimed at helping patients effectively manage symptoms, tackle the root of pain, and improve quality of life.
Have Peace of Mind When Treating Hand Numbness
Hand numbness and tingling – especially as your symptoms begin to progress – can significantly impact daily life, but early diagnosis and treatment can offer relief. By seeking immediate medical attention, you can confirm if cervical radiculopathy is the cause or rule out other conditions and take steps to manage symptoms effectively and prevent progression.
Lastly, having a full picture of the treatment options available to you can help you make the best decisions for your health and take steps to address the root cause of pain to restore your quality of life.