The C1 and C2 vertebrae, also known as the atlas and axis, are the uppermost bones in the spinal column. They play a crucial role in supporting the skull and enabling head movements.
Damage or injury to these vertebrae often leads to pain, limitations to daily activities, and reduced quality of life. Many patients, without truly understanding the root cause of their pain, resort to long-term medication use to find relief. This not only masks the symptoms and delays diagnosis but can also exacerbate the condition. In time, untreated vertebral problems increase the probability of requiring surgery.
Our approach offers a way to break this cycle. At the Centeno-Schultz Clinic, trained physicians use advanced diagnostic methods and interventional orthobiologics to promote the body’s natural ability to heal. This can help patients avoid surgery and prolonged medication.
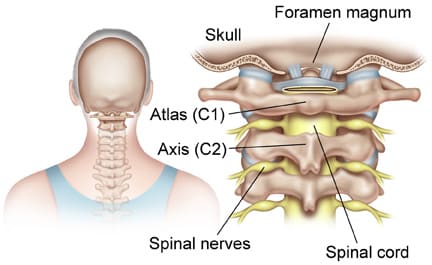
Location of Atlas and Axis Vertebrae
C1 and C2 are the first two vertebrae at the upper part of the cervical spine. Together, they form a complex structure that supports the skull, known as the atlantoaxial joint. This structure also provides an optimal range of motion without compromising stability.
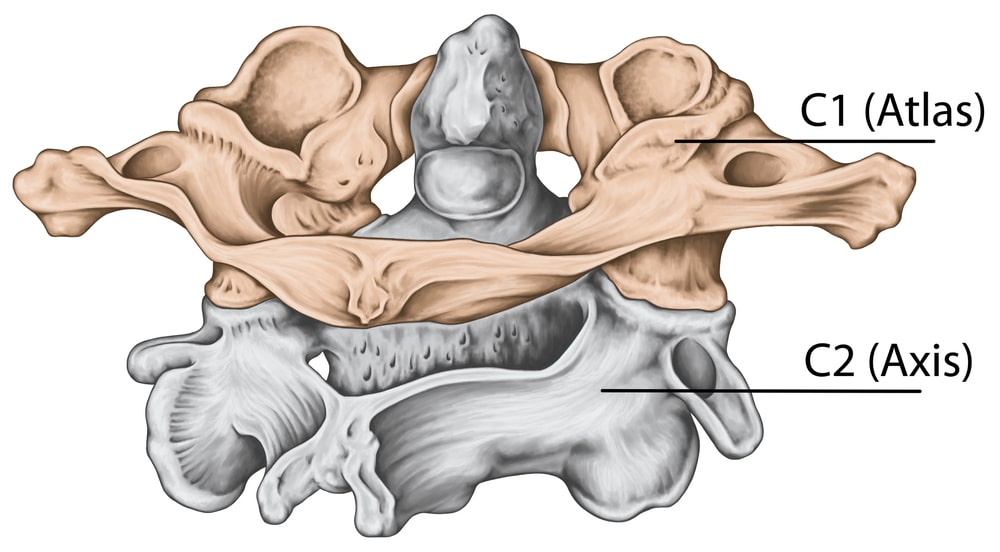
C1 Vertebra
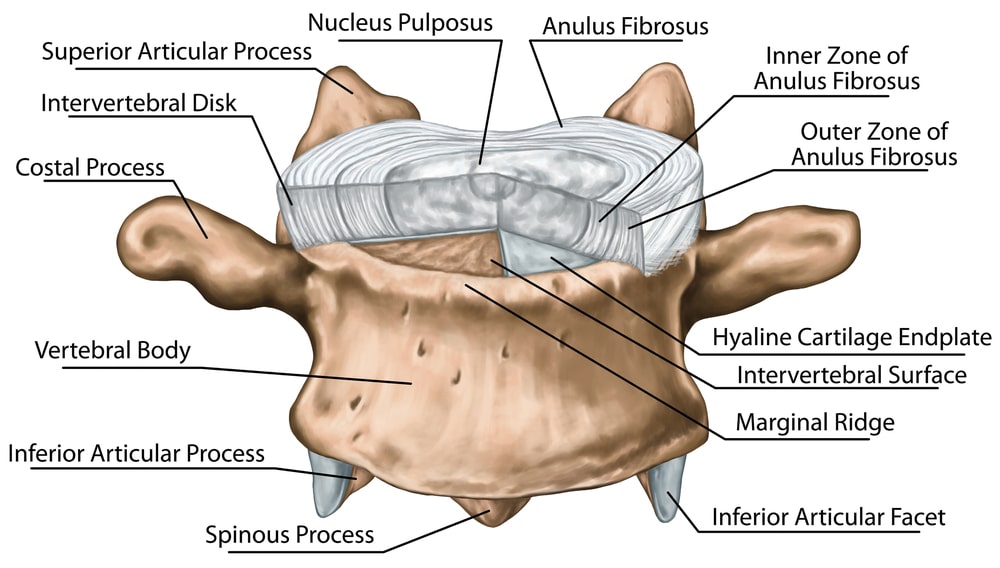
The C1 vertebra, called the atlas, is the first cervical vertebra. It is located just below the skull. It is unique in shape compared to other vertebrae because it has a ring-like structure and no vertebral body. The vertebral body is a thick, disc-shaped anterior portion of a vertebra, which has the role of distributing loads. Without a vertebral body, the C1 allows for greater range of motion of the neck and skull.
C2 Vertebra
The C2 vertebra, known as the axis, sits directly below the atlas, or C1. It is recognizable for a distinctive projective structure, known as the “peg,” “odontoid process,” or “dens.” This structure extends upwards into the atlas. It provides a stable point upon which the atlas bone can rotate.
Functions of Cervical Vertebrae
The cervical spine is a compact section of the spine, composed of seven vertebrae, C1 to C7. The cervical spine has many critical functions. It supports the skull, allowing for a broad range of head movements.
.
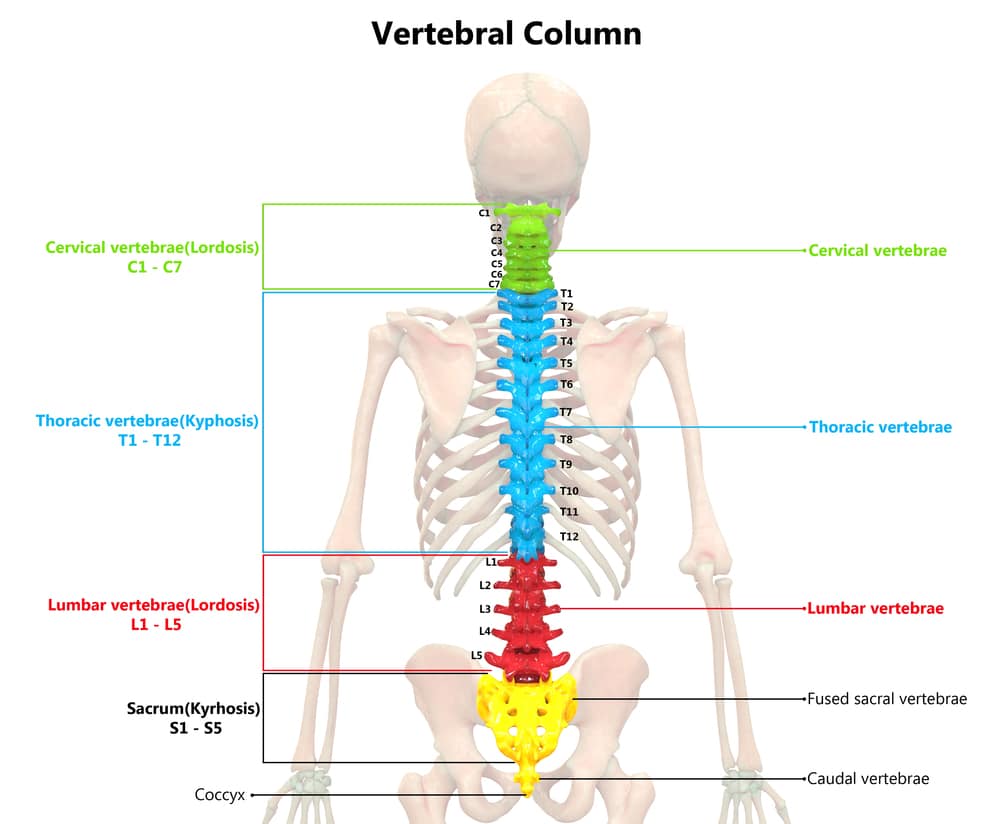
It also protects the upper section of the spinal cord, which houses several nerves and is essential for neural communication throughout the body. Vertebral arteries also run through the cervical spine, aiding in providing blood flow to the brain.
In particular, the C1 and C2 vertebrae have specific functions:
- C1 (Atlas) Vertebra:
The C1 is a stable but flexible platform balanced atop the spine. This platform provides support and stability to the skull. As noted above, this vertebra lacks a vertebral body. This characteristic allows for greater mobility compared to other vertebrae, facilitating movements like nodding and lateral head tilting.
Additionally, the C1 houses passageways for vital nerves and blood vessels critical for motor control, neural communication, and oxygen supply to the brain. These include:
- The spinal accessory nerve, crucial for controlling certain neck and shoulder muscles.
- The vertebral arteries, which supply blood to the brain.
- C2 (Axis) Vertebra:
The C2 supports rotational movements of the head and stabilizes the atlas. The C2’s dens, which fits into the C1 vertebra, acts as a pivot for the atlas. This allows the head to turn from side to side.
This vertebra also plays a role in securing the structural integrity of the cervical spine and protecting the nerves that transmit signals between the brain and the rest of the body.
Signs of Vertebral Pain
Cervical pain can be caused by injuries, overuse, or poor posture. Age-related wear and tear can also deteriorate components of the spine’s joints, such as the discs of cartilage that cushion the vertebrae during movement. Recognizing the signs of vertebral pain can help in seeking timely medical intervention and appropriate care.
Here are some of the symptoms to watch out for:
- Sharp, burning neck pain: This kind of pain may indicate nerve irritation or pinching. From the cervical vertebrae, eight pairs of cervical nerves exit the spine and innervate other parts of the body, providing motor and sensation signals to limbs and organs. When these nerves become compressed by herniated discs or bone spurs, they can produce intense, burning sensations.
- Throbbing pain up to the back or head: Throbbing pain results from tension headaches originating from neck strain, muscle overuse, or vertebral misalignment. When cervical nerves are affected, the pain can also radiate upward.
- Pain in the temple and/or behind the eyes: This is known as referred pain, a type of pain that derives from the cervical spine and spreads to other parts. It can occur for several reasons, including strain and poor posture. When nerves in the cervical region are compressed or pinched, they can project pain signals to nearby areas, including the temples and behind the eyes. This pain is commonly seen in conditions like cervicogenic headaches.
- Neck-tongue syndrome: This is a relatively rare condition estimated to affect around 0.22% of adults. It occurs when certain neck movements cause symptoms like sudden tingling or numbness of the tongue. This condition stems from irritation of the C2 nerve root, which is closely associated with the hypoglossal nerve, the nerve that controls tongue movements.
- Light sensitivity: Light sensitivity is a symptom closely associated with headaches caused by problems with neck tissues, such as tension or strain. These headaches include cervicogenic headaches and migraines.
- Tiredness: Tiredness can be a secondary symptom of chronic neck pain. Persistent discomfort and interrupted sleep patterns due to pain can lead to fatigue. Additionally, the body’s constant fight to manage pain and fight inflammation of neck tissues can drain energy reserves, leading to tiredness and inability to concentrate.
- Nausea: Typically, this symptom relates to disruption in the vestibular system. The vestibular system, which is found in the inner ear, helps control balance and the sense of position (proprioception). Neck movements can influence its ability to function properly, which can lead to nausea, queasiness, and balance issues. Nausea can also occur due to severe cervicogenic headaches, migraines, or nerve problems in the cervical spine.
Problems Stemming from C1 and C2 Damage
The C1 and C2 vertebrae can be affected by a range of conditions that cause damage, restricted mobility, and pain. These include:
- Arthritis: Arthritis occurs when inflammation in the body wears down the cushioning cartilage between the vertebrae. The degeneration reduces joint space, causing bones to rub together. This leads to pain, swelling, friction damage, limited range of motion, and if not treated, deformities like bone spurs. Osteoarthritis often affects the lumbar and cervical areas of the spine, with cervical osteoarthritis found in over 80% of people aged 55 and above.
- Spinal fractures: Spinal fractures in the C1 and C2 vertebrae typically stem from severe trauma, like car accidents or falls. Fractures can compromise spinal stability and may cause spinal cord injury or nerve damage, causing pain and disability.
- Vertebral artery injury: The vertebral arteries run through the cervical vertebrae. Injuries to these arteries, possibly from causes like trauma or vascular disease, can reduce blood flow to the brain. This may cause dizziness, headaches, or even stroke symptoms.
- Occipital neuralgia: This condition refers to the irritation or damage of the occipital nerves. These nerves run from the top of the spinal cord through the scalp. Occipital neuralgia can interfere with the nerves’ ability to carry signals from and to the brain, causing sharp pain and numbness. In the cervical spine, this can occur due to damage to the C1 or C2 vertebrae or severe trauma. Age-related degeneration can also narrow the joint space and cause deformities that compress the occipital nerves.
- Crowned dens syndrome: Crowned dens syndrome is characterized by the build-up of calcium around the dens of the C2 vertebra. This prevents the C1 from pivoting, limiting movement. The calcium deposits also cause inflammation, which causes pain and swelling.
- Trauma – motor vehicle accidents, sports-related injuries: Trauma to the C1 and C2 vertebrae can occur due to car accidents and sports injuries, often because of whiplash or direct blows to the neck. Traumatic injuries can disrupt the alignment and integrity of these vertebrae, causing pain, stiffness, and potentially neurological symptoms.
- Congenital abnormalities: Congenital abnormalities can increase the risk of nerve compression in the spine. This can cause pain, reduced neck mobility, and complications such as nerve damage. Common congenital abnormalities affecting the cervical spine include atlantoaxial instability, where the C1 and C2 vertebrae are excessively mobile. This condition is rare among healthy individuals, but it can affect between 25% and 80% of those with rheumatoid arthritis.
- Tumors: Benign or malignant tumors can grow in the cervical spine and affect the C1 and C2 vertebrae. They may exert pressure on the spinal cord or nerves, causing pain and neurological problems, as well as other symptoms across the body.
- Infections: Infections like osteomyelitis can affect the C1 and C2 vertebrae. Bacterial invasion can cause inflammation, bone destruction, and, potentially, the formation of abscesses. This can lead to severe pain and structural instability.
- Misalignments / Hypermobile: Misalignments can result from trauma, degenerative changes, poor posture, or hypermobility. Vertebrae that fall out of alignment can cause muscular strain, nerve irritation, and restricted neck movements, contributing to chronic pain and discomfort.
Effects of C1 and C2 Vertebrae Injuries
Injuries to the C1 and C2 can lead to both localized and systemic symptoms, which are felt in several parts of the body. Some of the effects of injuries to the cervical vertebrae include:
- Complete paralysis of arms and legs: In severe / rare cases, complete paralysis, or quadriplegia, can occur when injuries damage the spinal cord, the bundle of nerves that traverses the spine. The C1 and C2 vertebrae house crucial nerves. When they are damaged, the brain’s motor and sensation signals can’t reach the arms and legs, resulting in total paralysis.
- Muscle atrophy: Muscle atrophy occurs when nerve damage prevents nerve signals from traveling from the brain to the muscles. Without neural stimulation, muscles deteriorate due to disuse, decreasing in size and strength.
- Limited range of motion in head and neck: Injuries to the atlas and the axis can limit head and neck movement. The body’s inflammatory response to injury also causes pain and swelling, further reducing neck flexibility and rotation. If not properly addressed, this can lead to mobility problems.
- Difficulty in breathing without apparatus: Breathing difficulties arise when C1-C2 injuries affect the phrenic nerve, which controls the diaphragm. If nerve signals are disrupted, the diaphragm can fail to move properly, making mechanical ventilation necessary to maintain respiratory function.
- Problems in speaking: Speaking issues can result in spinal nerves in the C1 and C2 vertebrae becoming damaged. This can compromise the neural pathways responsible for muscle control in speech, leading to difficulties in articulating words or producing sound.
Non-surgical Medical Options
Non-surgical treatments for C1 and C2 injuries are often the first line of treatment for neck injuries. They aim to ease symptoms and support recovery without invasive procedures. Common treatments include:
- OTC medication: Over-the-counter medications, such as ibuprofen or acetaminophen, work by reducing inflammation and pain. However, prolonged use can lead to side effects, including an increased risk of heart attack, stroke, stomach, ulcers, and kidney dysfunction.
- Halo-thoracic brace: The halo-thoracic brace stabilizes the cervical spine by keeping the head and neck immobilized. This allows healing and prevents further injury. It is often part of a more comprehensive treatment plan.
- Sterno-occipital-mandibular immobilization: This device restricts head movement by anchoring to the sternum, occiput, and mandible. It helps keep the neck in alignment with the rest of the spine and prevents movement during the healing process. It is often used to stabilize cervical fractures and other traumatic injuries but can be cumbersome and impede daily activities like eating.
- Physical therapy: Physical therapy involves exercise and other non-invasive therapies to strengthen neck muscles and improve flexibility. A physical therapist may also use modalities like acupuncture, ultrasound, and electrical stimulation to support recovery.
- C1-C2 traction: C1-C2 traction involves gently stretching the cervical spine to relieve pressure and align vertebrae. It can reduce pain and spasms. However, it carries risks of increased pain or nerve compression if not properly performed.
- Injection: Injections such as corticosteroids can reduce inflammation and pain at the injury site. They provide quick relief but long-term use can cause complications like cartilage loss.
- The Regenexx approach: In some cases, musculoskeletal issues affecting the spine don’t require medications or surgery to heal. That’s because the body has an intrinsic ability to heal naturally.
The Regenexx approach leverages interventional orthobiologics to support this ability, providing a path to recovery that doesn’t involve drugs or invasive treatments. But you must understand that many of these injections need to be done only by the highest trained interventional doctors!
While most spine doctors can treat your spine, the upper cervical joints are more unique and not many spine physicians are trained in how to do this safely! Click the pages below to learn more:
- Injecting the C1-C2 Facet Joint Under Ultrasound
- CCJ Instability: Patients Don’t Know What Their Doctors Don’t Tell Them
At Centeno-Schultz Clinic, our physicians are highly trained and do these injections routinely on a weekly basis compared to other spine doctors that may do these injections once a year! To learn more, visit this page: Craniocervical Instability Cure | CCJ Instability Institute.
Surgical Treatments
Surgery may be required for C1 and C2 vertebrae injuries if non-surgical methods prove ineffective or if there is significant structural damage. Cases when surgery may be prescribed include severe spinal instability, compression of the spinal cord, or worsening neurological problems.
The type of surgical intervention prescribed varies according to the root cause of the problem and the patient’s needs. However, common interventions include:
- C1-C2 fusion: In a C1-C2 fusion surgery, the two vertebrae are permanently joined together by removing the cushioning cartilage between them. This surgery is typically used for conditions like severe arthritis, fractures, or instability from trauma. The fusion prevents movement, to alleviate pain and protect the spinal cord. However, this can significantly reduce neck mobility.
- Laminectomy: A laminectomy involves removing the lamina. The lamina acts as a “roof” for the spinal canal, which houses the spinal cord. It helps to alleviate pressure on the spinal cord or nerves due to the narrowing of the spinal canal. This condition is known as stenosis and can stem from bone spurs or herniated discs. While laminectomy is usually successful, around a quarter of patients are not entirely satisfied with the outcomes.
- Odontoid screw fixation: Odontoid screw fixation is employed to stabilize fractures of the odontoid process or dens (the peg-like structure on the C2 vertebra). It involves placing a screw through the mouth into the odontoid to promote bone healing. This surgery allows for rotation and less neck movement loss compared to fusion. Complications can include screw misplacement, nonunion of the fracture, and nerve injury.
- Transoral odontoidectomy. Transoral odontoidectomy is a procedure where the surgeon removes part of the C2’s dens through the mouth to relieve compression on the spinal cord. This complex surgery is used in severe cases of nerve compression that cause neurological problems and when other approaches are not possible. Risks are high because this surgery is highly invasive. It also involves significant postoperative care needs and lengthy recovery periods.
Neck Surgery Post-Recovery
After surgery, adequate care and rehabilitation are necessary to promote healing, restore function, and prevent complications.
Rest
Rest is crucial for recovery after neck surgery. It allows tissues to heal without undue strain or movements that could compromise surgery outcomes. Rest also prevents re-injury and reduces inflammation.
However, patients should always follow the instructions of their surgeon regarding immobilization. In some cases, keeping the neck still for too long can lead to muscle atrophy and delay healing. Additionally, a 2018 study shows that, following a type of neck surgery (anterior cervical discectomy and fusion), neck bracing didn’t offer any advantages.
Physical Therapy
Physical therapy helps restore strength, flexibility, and range of motion. Therapeutic exercises designed by a physical therapist specifically target the neck and surrounding muscles. Other non-invasive modalities, including ultrasound, electrical stimulation, and massage may be used.
These exercises promote muscle re-education, increase circulation, and reduce stiffness. However, it is critical to follow the therapist’s guidance to avoid overexertion and re-injury.
Healthy Lifestyle
Adequate nutrition and hydration provide the necessary vitamins and minerals for tissue repair and energy production. Additionally, avoiding smoking and limiting alcohol consumption can improve blood circulation, reduce inflammation, and boost tissue oxygenation, all of which are crucial for recovery.
Prognosis
The prognosis for C1 and C2 vertebrae issues varies greatly and depends on several factors:
- The patient’s general health
- How quickly diagnosis and intervention are carried out
- The type of treatment used
- Postoperative care
- Adherence to the physician’s recommendations
- Age and lifestyle
Surgical interventions to the cervical spine require long recovery times. Although most patients can begin to move their neck gently after a few weeks of the surgery, full recovery can take six to 12 months. Even after full recovery, surgery does not guarantee entirely pain-free outcomes.
Possible Complications
Medical procedures involving the spine, particularly the C1 and C2 vertebrae, carry certain risks, even with modern techniques and advancements. Understanding these complications helps in making informed decisions about pursuing such interventions.
- Bleeding: Bleeding is a common risk during and after spinal procedures. It can create pressure in the spinal area, impacting recovery and leading to further complications.
- Allergic reaction: Materials used during the procedure, such as anesthesia or contrast dyes, may trigger allergic reactions. Allergy symptoms can range from mild irritations to severe reactions requiring immediate medical intervention.
- Infection: Despite sterile environments, infections can occur if bacteria enter the surgical site. Infections can reduce recovery times, affect surgical outcomes, and, in some cases, they can be life-threatening. The spine’s proximity to critical spinal cord nerves makes this a particularly serious complication.
Have Yourself Examined
Ongoing or worsening neck pain may indicate an underlying, serious medical condition. It’s vital to seek medical attention and find an adequate line of treatment without delay.
Get yourself evaluated and know if your condition can be treated with non-surgical procedures.
