Alternatives To Surgery For A Herniated Disc
Am I a Candidate?Disc herniations can be quite painful and regrettably many patients jump straight to surgery for these. However, after a certain amount of time, a pain similar to preoperative pain returns and patients start to search for alternatives to surgery. Many times surgery is unavoidable and necessary while others may have been avoidable.
Today, let’s dive into the details of disc herniations, when surgery is necessary or not. Finally, we will discuss some alternatives to surgery.
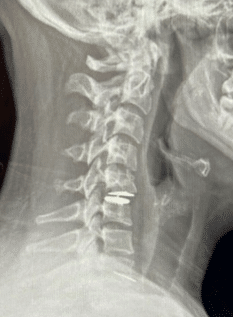
What Is Cervical Disc Herniation Surgery?
Before we discuss surgery, let’s first understand what a herniated disc is.
The spine is made up of individual bones called vertebrae. Between each vertebra, there is a cushion-like structure called a disc that acts as a shock absorber.
A herniated disc, also known as a slipped or ruptured disc, occurs when the soft inner part of the disc protrudes through the outer layer and presses on the spinal nerves. Learn more about what a cervical disc is here.
A disc herniation, also known as a slipped or ruptured disc, occurs when the soft inner part of a spinal disc protrudes through the outer layer and presses on the spinal nerves. While the exact cause of disc herniation is not always clear, there are several factors that can increase the risk of developing this condition.
Causes
- Age: As we age, the discs in our spine can become less flexible and more prone to injury. This can increase the risk of a herniated disc.
- Genetics: Some people may have a genetic predisposition to developing herniated discs.
- Trauma: A sudden injury, such as a fall or car accident, can cause a herniated disc.
- Repetitive Motion: Activities that involve repetitive motion, such as lifting heavy objects or twisting the spine, can increase the risk of a herniated disc.
- Obesity: Being overweight or obese can put extra pressure on the spine and increase the risk of a herniated disc.
- Smoking: Smoking can decrease blood flow to the spinal discs, which can weaken them and increase the risk of a herniated disc.
- Poor Posture: Poor posture can put extra strain on the spine and increase the risk of a herniated disc.
- Degenerative Disc Disease: This is a condition where the discs in the spine gradually break down over time, which can increase the risk of a herniated disc.
Symptoms
Symptoms of a herniated disc can include:
- Pain, which can be described as sharp, stabbing, burning, or shooting.
- Numbness
- Tingling
- Weakness in the back, legs, or arms
These symptoms can range from mild to severe and can be debilitating if left untreated. They can also be made worse by certain positions. With disc injuries, sitting can be the most uncomfortable position because it can cause increased pressure on the disc. When the disc is damaged, pressure pushes on the nerves around it, worsening pain!
When Do Doctors Recommend Surgery?
Pain is NOT an indication to have surgery!
I see this far too often: A patient comes in for an evaluation with a history of fusion / disc replacement / laminectomy surgery. When I dive into reasoning why surgery was performed, many times, it was for pain relief and that patient had not first considered conservative therapy!
There exists excellent long-term data showing no difference in pain relief PLUS 1 in 10 patients that undergo spinal surgery end up developing worse or new symptoms from the surgery.
But when do I send patients for surgery?
The absolute #1 indication for surgery is progressive weakness! Weakness is a sign and symptom of mechanical nerve compression and should be taken seriously. Many patients want to try to avoid surgery, but in these cases, I do not recommend trying any injection-based treatments or physical therapy alone. Surgery is needed with these.
Factors To Consider Before Undergoing Cervical Disc Herniation Surgery
Cervical disc herniation is a condition where a spinal disc in the neck protrudes out of its normal position and presses on the nerves in the spinal cord, causing pain, numbness, and weakness. In some cases, surgery may be recommended to alleviate these symptoms.
However, before undergoing cervical disc herniation surgery, there are several important factors to consider:
- Severity of Symptoms: Surgery is typically recommended for individuals with severe and disabling symptoms that do not respond to conservative treatments such as physical therapy, medications, and less invasive injection-based therapies.
- Duration of Symptoms: It’s important to consider how long the symptoms have been present.
- Age and Overall Health: The age and overall health of the individual can affect the risks associated with surgery. Older individuals or those with underlying medical conditions may be at a higher risk for complications during or after surgery.
- Type of Surgery: There are several types of surgeries available for cervical disc herniation, and the type of surgery recommended may depend on the location and severity of the herniation. It’s important to discuss the risks and benefits of each type of surgery with your surgeon.
Success Rates
The success rate of cervical disc herniation surgery can vary depending on the type of surgery and the individual’s health. It’s important to discuss the success rates with a qualified healthcare provider.
If you are having surgery for pain relief, remember that several long-term RCTs demonstrate that relief from surgery is comparable to relief from physical therapy. But, if having progressive neurologic weakness then surgery has a good chance at stopping the progression.
Potential Risks
Risks and complications: As with any surgery, cervical disc herniation surgery carries risks, such as infection, bleeding, nerve damage, and complications from anesthesia. It’s important to discuss these risks with your surgeon and weigh them against the potential benefits of surgery.
In addition to the added risks, 1 in 10 patients end up with worse pain after surgery when compared to pain prior to the surgery.
Benefits
Neck surgery for pain relief can be effective for some individuals, but it’s important to note that the success rate depends on several factors, including the type of surgery, the underlying cause of the pain, and the individual patient’s health and circumstances.
Additionally, there are risks associated with any surgery, including the risk of the surgery not being effective or making the pain worse. Studies have shown that the success rate of neck surgery for pain relief varies depending on the type of surgery and the underlying condition being treated.
For example, a study published in the Journal of Neurosurgery: Spine found that the success rate of anterior cervical discectomy and fusion (ACDF) surgery for the treatment of cervical disc herniation was around 85%.
Another study published in The Spine Journal found that patients who underwent cervical laminoplasty for the treatment of cervical myelopathy (a condition where the spinal cord becomes compressed) had a success rate of around 70%.
Recovery Time
Recovery time: Recovery time can vary depending on the type of surgery and the individual’s health. It’s important to consider the impact of the recovery time on daily activities and work.
Life After Herniated Cervical Disc Surgery
The biggest problem with either fusion or disc replacement surgery is the ASD (Adjacent Segment Disease). A search of the US National Library of Medicine search was a 5-year randomized controlled trial of disc replacement versus fusion in the neck. It concluded that there is no difference in the rate of ASD between the procedures (6).
Even more research:
This study demonstrated that the way the spine bones move is changed by ADR (7). Meaning, they don’t move in the way they were designed.
This high-level meta-analysis concluded that a reduction in ASD can’t yet be proven when ADR is compared to fusion (8).
This Swedish registry study also concluded no difference in ASD rates between ADR and fusion at 5 years (9).
Now compare those studies showing that ADRs don’t prevent ASD to this 2018 recent review of the literature that seemed to be a glowing review of the technology (10). However, the supervising author on this one is a US neurosurgeon, so I looked up his page on the ProPublica website to see if he had received money from device manufacturers.
Sure enough, he’s listed as receiving more than a million dollars in device-company payments.
There are other studies comparing specific ADR devices to fusion, which all seem to show better results. However, most of these seem supported by a specific manufacturer of a specific device.
I wanted to look up more physicians involved in these studies, but it seems like most of the device-company-sponsored studies are performed in China, making those physicians and their payments outside of the reach of US Internet searches.
Even those studies aren’t all glowing. Take, for example, this 5-year study performed on the Prestige-LP device (11). This seemed to show that the Prestige artificial disc was better than a fusion spacer in terms of a reduction in ASD (8.3% vs. 22%). However, exactly one-third of patients who got the Prestige device had heterotopic ossification as a side effect of the device. What’s that? Very concerning abnormal bone growth.
Is There Really An Alternative To Cervical Disc Herniation Surgery?
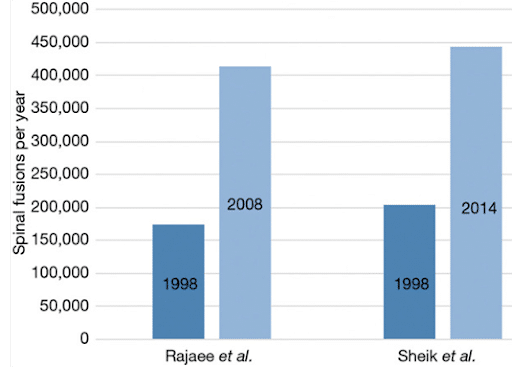
While surgery avoidance is critical for long-term success of patients, traditional medicine has not done a great job at reducing surgical conversion rates over the last 50 years.
Looking at the total number of fusion surgeries over time, each decade continues to double to rate previously. Which means that steroids and physical therapy are not changing the conversions over time.
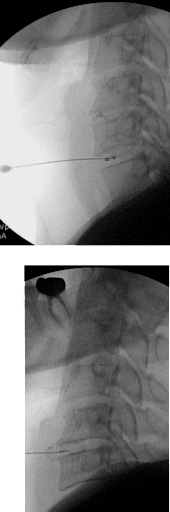
The idea of injecting something into a disc to attempt to heal the disc injury has been postulated over the last 20 years and we know that this can help disc herniation, annular tears and disc protrusions but cannot help disc height!
Platelet-Rich Plasma Solutions
PRP = platelet rich plasma which is probably the most studied treatment.
The use of PRP injected into the disc has been the subject of several studies. Lutz et al. have published several papers on leukocyte-rich PRP (LR-PRP) injected into the discs of DDD patients with excellent results compared to placebo saline injections (12,13).
That procedure has since been optimized further by substituting higher-dose PRP (14). The idea that a higher platelet concentration leads to better clinical results was also reported by Jain et al. (15).
Bone Marrow Concentrate
Bone Marrow Concentrate, or BMC, is created by isolating the fraction of bone marrow aspirate containing mesenchymal stem cells.
The research on injecting BMC into low back discs goes back a number of years and was first published by Pettine et al.
This response depended on the number of cells delivered, meaning the patients injected with a higher number of stem cells (as determined by CFU-f) reported superior outcomes.
Wolff et al. have also reported solid clinical results using BMC injected into lumbar discs. Finally, Atluri et al. reported excellent results using disc and functional spinal unit injections with BMC.
The outcome of intradiscal injection of culture-expanded mesenchymal stem cells has also been reported in the literature.
Our group has also published positive case series results using culture-expanded cells.
Why Second Opinion Is Crucial When Examining Your Treatment Options
Second opinions from experts in cervical disc treatments are critical. Our Cervical Spine Experts: Drs Jason Markle and John Pitts have been treating cervical discs longer than anyone in the country. They can discuss if you are a candidate for this minimally invasive treatment to avoid the need for cervical disc surgery! If you’d like a second opinion from them, please go to this page.
Discuss your options and get the help you need for successful recovery. Request an appointment today!

Christopher J. Centeno, MD
Christopher J. Centeno, M.D. is an international expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate in orthopedics.
Dr. Centeno is one of the few physicians in the world with extensive experience in the culture expansion of and clinical use of adult bone marrow concentrate to treat orthopedic injuries. His clinic incorporates a variety of revolutionary pain management techniques to bring its broad patient base relief and results. Dr. Centeno treats patients from all over the US who travel to Colorado to undergo innovative, non-surgical treatments. Dr. Centeno has chaired multiple international research-based conferences. He also maintains an active research-based practice, with multiple publications listed in the US National Library of Medicine. Dr. Centeno has also served as editor-in-chief of a medical research journal dedicated to traumatic injury.
Dr. Centeno trained at the Baylor College of Medicine, Texas Medical Center, and the Institute for Rehabilitation Research. He hails from both Florida and New York and currently resides in Boulder, Colorado with his wife and three children.

John Schultz, MD
John R. Schultz M.D. is a national expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate for orthopedic injuries. He is board certified in Anesthesiology and Pain Medicine and underwent fellowship training in both. Dr. Schultz has extensive experience with same day as well as culture expanded bone marrow concentrate and sees patients at the CSC Broomfield, Colorado Clinic, as well the Regenexx Clinic in Grand Cayman. Dr. Schultz emphasis is on the evaluation and treatment of thoracic and cervical disc, facet, nerve, and ligament injuries including the non-surgical treatment of Craniocervical instability (CCI). Dr. Schultz trained at George Washington School of…
Read more
John Pitts, M.D.
Dr. Pitts is originally from Chicago, IL but is a medical graduate of Vanderbilt School of Medicine in Nashville, TN. After Vanderbilt, he completed a residency in Physical Medicine and Rehabilitation (PM&R) at Emory University in Atlanta, GA. The focus of PM&R is the restoration of function and quality of life. In residency, he gained much experience in musculoskeletal medicine, rehabilitation, spine, and sports medicine along with some regenerative medicine. He also gained significant experience in fluoroscopically guided spinal procedures and peripheral injections. However, Dr. Pitts wanted to broaden his skills and treatment options beyond the current typical standards of care.
Read more
Jason Markle, D.O.
Post-residency, Dr. Markle was selected to the Interventional Orthopedic Fellowship program at the Centeno-Schultz Clinic. During his fellowship, he gained significant experience in the new field of Interventional Orthopedics and regenerative medicine, honing his skills in advanced injection techniques into the spine and joints treating patients with autologous, bone marrow concentrate and platelet solutions. Dr. Markle then accepted a full-time attending physician position at the Centeno-Schultz Clinic, where he both treats patients and trains Interventional Orthopedics fellows. Dr. Markle is an active member of the Interventional Orthopedic Foundation and serves as a course instructor, where he trains physicians from around the world.
Read more
Brandon T. Money, D.O., M.S.
Dr. Money is an Indiana native who now proudly calls Colorado home. He attended medical school at Kansas City University and then returned to Indiana to complete a Physical Medicine and Rehabilitation residency program at Indiana University, where he was trained on non-surgical methods to improve health and function as well as rehabilitative care following trauma, stroke, spinal cord injury, brain injury, etc. Dr. Money has been following the ideology behind Centeno-Schultz Clinic and Regenexx since he was in medical school, as he believed there had to be a better way to care for patients than the status quo. The human body has incredible healing capabilities…
Read moreReferences:
- Bydon M, De la Garza-Ramos R, Macki M, Baker A, Gokaslan AK, Bydon A. Lumbar fusion versus nonoperative management for treatment of discogenic low back pain: a systematic review and meta-analysis of randomized controlled trials. J Spinal Disord Tech. 2014 Jul;27(5):297-304. doi: 10.1097/BSD.0000000000000072. PMID: 24346052.
- Wang QL, Tu ZM, Hu P, Kontos F, Li YW, Li L, Dai YL, Lv GH, Wang B. Long-term Results Comparing Cervical Disc Arthroplasty to Anterior Cervical Discectomy and Fusion: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Orthop Surg. 2020 Feb;12(1):16-30. doi: 10.1111/os.12585. Epub 2019 Dec 21. PMID: 31863642; PMCID: PMC7031601.
- Success rate of anterior cervical discectomy and fusion (ACDF) surgery for the treatment of cervical disc herniation: Pumberger, M., Chiu, Y. L., Ma, Y., Girardi, F. P., & Vougioukas, V. I. (2014). Reoperation rate after anterior cervical discectomy and fusion using a polyetheretherketone cage with and without anterior plate: a 10-year follow-up. The Spine Journal, 14(10), 2273-2278.
- Success rate of cervical laminoplasty for the treatment of cervical myelopathy: Tetreault, L. A., Rhee, J. M., & Wilson, J. R. (2013). National trends in the management of central canal stenosis: a Canadian population-based study. The Spine Journal, 13(7), 823-828.
- Risk of worsening symptoms after ACDF surgery for the treatment of cervical disc herniation: Epstein, N. E. (2010). Anterior cervical discectomy and fusion with and without instrumentation: review, complications, and rate of pseudarthrosis. Journal of Neurosurgery: Spine, 13(5), 580-593.
- MacDowall A, Canto Moreira N, Marques C, Skeppholm M, Lindhagen L, Robinson Y, Löfgren H, Michaëlsson K, Olerud C. Artificial disc replacement versus fusion in patients with cervical degenerative disc disease and radiculopathy: a randomized controlled trial with 5-year outcomes. J Neurosurg Spine. 2019 Jan 11;30(3):323-331. doi: 10.3171/2018.9.SPINE18659. PMID: 30641852.
- Wachowski MM, Weiland J, Wagner M, Gezzi R, Kubein-Meesenburg D, Nägerl H. Kinematics of cervical segments C5/C6 in axial rotation before and after total disc arthroplasty. Eur Spine J. 2017 Sep;26(9):2425-2433. doi: 10.1007/s00586-017-5073-z. Epub 2017 Apr 4. PMID: 28378073.
- Yang X, Janssen T, Arts MP, Peul WC, Vleggeert-Lankamp CLA. Radiological follow-up after implanting cervical disc prosthesis in anterior discectomy: a systematic review. Spine J. 2018 Sep;18(9):1678-1693. doi: 10.1016/j.spinee.2018.04.021. Epub 2018 May 8. PMID: 29751126.
- MacDowall A, Skeppholm M, Lindhagen L, Robinson Y, Löfgren H, Michaëlsson K, Olerud C. Artificial disc replacement versus fusion in patients with cervical degenerative disc disease with radiculopathy: 5-year outcomes from the National Swedish Spine Register. J Neurosurg Spine. 2018 Nov 2;30(2):159-167. doi: 10.3171/2018.7.SPINE18657. PMID: 30485205.
- Chang CC, Huang WC, Wu JC, Mummaneni PV. The Option of Motion Preservation in Cervical Spondylosis: Cervical Disc Arthroplasty Update. Neurospine. 2018 Dec;15(4):296-305. doi: 10.14245/ns.1836186.093. Epub 2018 Dec 14. PMID: 30545210; PMCID: PMC6347355.
- Gao X, Yang Y, Liu H, Meng Y, Zeng J, Wu T, Hong Y. A Comparison of Cervical Disc Arthroplasty and Anterior Cervical Discectomy and Fusion in Patients with Two-Level Cervical Degenerative Disc Disease: 5-Year Follow-Up Results. World Neurosurg. 2019 Feb;122:e1083-e1089. doi: 10.1016/j.wneu.2018.10.231. Epub 2018 Nov 9. PMID: 30415055.
- Tuakli-Wosornu YA, Terry A, Boachie-Adjei K, Harrison JR, Gribbin CK, LaSalle EE, Nguyen JT, Solomon JL, Lutz GE. Lumbar Intradiskal Platelet-Rich Plasma (PRP) Injections: A Prospective, Double-Blind, Randomized Controlled Study. PM R. 2016 Jan;8(1):1-10; quiz 10. doi: 10.1016/j.pmrj.2015.08.010. Epub 2015 Aug 24. PMID: 26314234.
- Cheng J, Santiago KA, Nguyen JT, Solomon JL, Lutz GE. Treatment of symptomatic degenerative intervertebral discs with autologous platelet-rich plasma: follow-up at 5-9 years. Regen Med. 2019 Sep;14(9):831-840. doi: 10.2217/rme-2019-0040. Epub 2019 Aug 29. PMID: 31464577; PMCID: PMC6770415.
- Lutz C, Cheng J, Prysak M, Zukofsky T, Rothman R, Lutz G. Clinical outcomes following intradiscal injections of higher-concentration platelet-rich plasma in patients with chronic lumbar discogenic pain. Int Orthop. 2022 Jun;46(6):1381-1385. doi: 10.1007/s00264-022-05389-y. Epub 2022 Mar 28. PMID: 35344055; PMCID: PMC9117340.
- Jain D, Goyal T, Verma N, Paswan AK, Dubey RK. Intradiscal Platelet-Rich Plasma Injection for Discogenic Low Back Pain and Correlation with Platelet Concentration: A Prospective Clinical Trial. Pain Med. 2020 Nov 1;21(11):2719-2725. doi: 10.1093/pm/pnaa254. PMID: 32869064.
- Centeno C, Markle J, Dodson E, Stemper I, Williams CJ, Hyzy M, Ichim T, Freeman M. Treatment of lumbar degenerative disc disease-associated radicular pain with culture-expanded autologous mesenchymal stem cells: a pilot study on safety and efficacy. J Transl Med. 2017 Sep 22;15(1):197. doi: 10.1186/s12967-017-1300-y. PMID: 28938891; PMCID: PMC5610473.
- Elabd C, Centeno CJ, Schultz JR, Lutz G, Ichim T, Silva FJ. Intra-discal injection of autologous, hypoxic cultured bone marrow-derived mesenchymal stem cells in five patients with chronic lower back pain: a long-term safety and feasibility study. J Transl Med. 2016 Sep 1;14(1):253. doi: 10.1186/s12967-016-1015-5. PMID: 27585696; PMCID: PMC5009698.
Am I a Candidate?
To answer this question, fill out the candidate form below to request a new patient evaluation, and a patient advocate will reach out to you to determine your next steps. Your one-hour, in-office or telemedicine evaluation will be with one of the world’s experts in the field of Interventional Orthopedics.