Anterior Cervical Discectomy And Fusion (ACDF) For Neck Pain
Am I a Candidate?Anterior cervical discectomy and fusion (ACDF) surgery is a surgical procedure used to treat cervical radiculopathy in the neck region. It is also an effective treatment for those with severe neck pain due to spondylosis, tumors, fractures, and herniated discs.
We’ll discuss the details of the ACDF surgery, including what the procedure involves, the risks, complications, and success rates.
What Is Anterior Cervical Discectomy And Fusion?
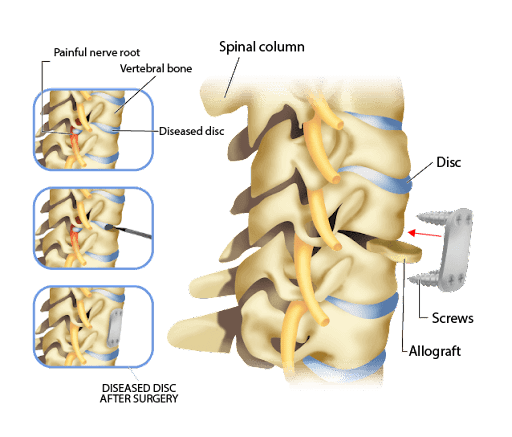
There are two stages of the ACDF surgery: discectomy and spinal fusion. In an anterior cervical discectomy and fusion surgery, the diseased disc is first removed and a bone graft is inserted in its place. The graft is then held in place by a plate and fused with the cervical vertebra above and below. These stages are explained further below:
- Discectomy: Discectomy starts with an incision in the front of the neck. The surgeon will move aside the thin layer of platysma muscle under the skin. They then separate the prevertebral fascia, a thin layer of fibrous tissue surrounding the spine.
The surgeon will generally confirm they are working on the right disc using x-ray guidance. Once this is confirmed, the surgeon will make an incision in the outer part of the disc, called the annulus fibrosus. The soft inner core (called the nucleus pulposus) is then removed.
All the other damaged parts of the disc are also extracted. If there are any bony spurs or disc components that have extruded through the posterior ligament, they are removed as well. There can be a single level disc replacement where a single disc is removed. There can also be a two level disc replacement where two successive discs are replaced.
- Spinal Fusion: The next step of the ACDF procedure is spinal fusion. Here, a bone graft or a “cage” is inserted into the space vacated by the extracted disc. This prevents the disc space from collapsing. It also provides room for new bone to form a bridge between the two spinal vertebrae.
A small metallic plate is then fixed with screws to the front of the vertebra above and below. This makes the vertebral column more stable while the bones fuse and heal.
Common Cervical Conditions Treated With ACDF
There are a variety of conditions that are treated with ACDF. They are listed below:
- Bulging / Herniated Cervical Disc: Bulging or herniated discs can lead to severe neck pain and cervical radiculopathy. When the herniated disc is removed in an ACDF surgery and replaced with a graft, it can eliminate the nerve compression from the affected disc.
- Degenerative Disc Disease (DDD): In DDD, the disc gradually degenerates and can herniate over time. ACDF can be used to remove a severely degenerated disc that is pressing on a nerve and causing weakness, changes in sensation, and restricted movement.
- Spondylosis: Spondylosis is a painful condition caused by wear and thinning of the intervertebral discs. Bony spurs may also develop. Bony spurs are tiny outgrowths of bone that usually occur where two bones meet. Bony spurs can develop during the healing process after injury or from wear due to age.
The ACDF procedure can be used to both replace the disc and remove any bony spurs. This can alleviate the pain andreduce the risk of symptoms in the future.
- Tumors: Cancers and tumors of the intervertebral bones and spinal cord can affect the spine. As the tumor grows, it can compress the discs and invade adjacent structures, gradually invading the blood vessels and nerves.
During an ACDF procedure, tumors and any affected discs can be removed and replaced with a bone graft to relieve the nerve compression. - Fractures: Vertebrae fractures due to herniated discs or tumors can be treated with ACDF surgery. In the fusion stage of the procedure, the fractured bodies can be fused together by the metal plate. As the bone heals, this metal plate will bridge the fracture.
The Ideal Candidate For ACDF Surgery
When to have ACDF surgery is a question that depends on multiple factors like severity of symptoms and the intensity of pain. Anterior cervical discectomy and fusion surgery is ideal for the following candidates:
- If imaging reveals a single or multiple herniated or degenerative discs
- When there are severe neurological symptoms in the hand or arm, such as weakness, loss of reflexes, and paresthesia
- If the pain in the arm is more severe than the pain in the neck
- If conservative treatment with medications and physical therapy has failed
How Does ACDF Surgery Work?
ACDF surgery works by decompressing the affected nerves in the spine. Conditions such as DDD, herniated discs, and spondylosis can all cause pressure on the spinal nerves and spinal cord. Surgeons using the ACDF procedure can relieve this pressure by removing the affected discs and stabilizing the vertebral column by fusing the bone graft to the vertebra above and below.
What To Expect During Recovery
So, what can you expect during recovery following an ACDF procedure? Some of the restrictions, incision care instructions, and medications that are used during recovery are explained below:
Restrictions
The surgeon will usually outline certain restrictions after an ACDF surgery to ensure you are safe during the recovery period following surgery. These restrictions include:
- Avoid smoking as cigarettes contain nicotine, which is a potent vasoconstrictor. Nicotine can affect the smaller blood vessels in the spine and reduce the blood supply to the area. Avoiding cigarettes will help ensure adequate blood supply and proper healing.
- Avoid alcohol as it can thin the blood. Alcohol can cause excess bleeding and delay your healing. It can also prolong the effect of your anesthesia.
- Avoid heavy lifting – do not lift anything heavier than 5 lbs for at least four weeks. Lifting can put pressure on the spine, as the added pressure can inflame the surgical area, cause edema, and delay healing.
- Avoid strenuous activities that cause the neck to turn sharply, including getting dressed, driving, and sexual intercourse. The cervical spine needs time to recover, so it’s important to restrict these activities until your follow-up visit.
Incision Care
The incision site must be protected as this can be a source of infection if it’s not cared for properly. To this end, take the following steps:
- Follow the instructions of your surgeon.
- Do not shower for at least two days after your surgery if staples or sutures were used.
- Keep the dressing dry at all times.
- If the incision was closed with glue, then avoid touching this area. If you have to wash, do it gently with soap and water.
- Always cover the incision with a dry gauze dressing.
- If you find that the incision is draining fluid or blood beyond two dry gauze dressings within two to four hours, then call your doctor.
- Do not apply any creams, lotions, or ointments to the incision area.
- Use clean dressings, clean clothes, and clean linens to avoid contaminants and microbes. Additionally, use clothes that are not too restrictive or tight around the neck area.
- Keep an eye on the incision area. If there is any swelling, separation of the edges of the incision site, or worsening pain, call your doctor.
Medications
After your procedure, you will be prescribed pain medications and anti-inflammatory medications. It’s important to take your medications as prescribed. Some of the medications that may be prescribed are as follows:
- Pain medications: Non-steroidal anti-inflammatories (NSAIDs) and opiate medications may be prescribed, depending on your level of pain. NSAIDs are a class of drugs that reduce inflammation and relieve pain by nullifying the action of various inflammatory chemicals.
- Anti-acidity medications: To counter the acidity negative effects of the pain medications, you may be prescribed proton pump inhibitors and other antacids.
- Stool softeners: Pain medications can also cause constipation and so it is necessary to hydrate and eat fiber-rich foods. However, doctors may also prescribe stool softeners or laxatives to loosen the stool and encourage bowel movements.
- Anticoagulants: Depending on your age and medical history, doctors may prescribe anticoagulants for a short period of time after the surgery.
Follow-Up Post-Operatively
Your recovery doesn’t just end after your first follow-up visit. There are several steps you can take between follow-up appointments to minimize pain and avoid revision surgeries in the future. They are summarized below:
- Wear a cervical brace or collar to support the neck during the first few weeks (as directed by a health professional).
- Avoid activities that strain the neck.
- Follow an exercise program that eases the pressure on the spine as prescribed by your rehab team. Additionally, you can work with a trainer to learn how to use proper lifting techniques.
- Maintain a normal body weight as this will ease the pressure on your spine.
- Use an ergonomic desk and chair for your work as well if you are using a computer.
- Show up for all follow-up appointments. Your surgeon will likely request x-rays at each of these visits to ensure that the fusion is healing and confirm the procedure was successful.
How To Ensure ACDF Surgery Is A Success And Mitigate Any Risks
Here are some steps that a person undergoing ACDF surgery can take before, during, and after the procedure to ensure the success of the surgery and mitigate any risks.
What To Do Before The ACDF Surgery
Before the ACDF surgery, the following must be done:
- The patient must quit smoking, ideally a month before the surgery. This will help avoid unwanted blood vessel constriction and lessen the chances of pneumonia. If the patient needs help quitting smoking, they can talk to their doctor about additional resources to help, such as medications or cognitive behavioral therapy.
- The patient must shower the neight before surgery using antibacterial soap as the skin houses microbes.
- Ideally, the patient should stop all herbal remedies one week before surgery.
- The patient should not eat or drink after midnight before surgery.
- All jewelry, makeup, nail polish, and piercings should be taken off the day before the surgery.
- A list of all current medications and allergies must be carried for the anesthesiologist.
What Happens During ACDF Surgery
Here’s what happens during the procedure:
- The patient is given an anesthetic to put them to sleep.
- The surgeon then inserts a breathing tube in the mouth. IV antibiotics are started as a precautionary measure to prevent infections.
- Calf compression devices are also used to lessen the risk of developing blood clots in the legs.
- An incision is made in the front of the throat. After the dissection of muscles and fascia, the doctors then insert a needle into the disc space and take an x-ray to identify the affected disc.
- The affected disc is then removed.
- The doctor uses a microscope or special surgical magnifying glasses to see the spinal canal and nerves.
- Parts of the vertebral bone adjacent to the transverse process are removed and the posterior longitudinal ligament is examined. Each nerve root is identified and decompressed using a process called rhizolysis.
Also known as radiofrequency lesioning, rhizolysis is a process of burning the nerves to prevent them from sending pain signals to the brain. The heating temperature that is used is 80 degrees and the heat is applied for about 2-3 minutes.
- The vacant space is filled with a cage made out of polyetheretherketone (PEEK), carbon fiber, or titanium. The cage is filled with bone shavings and granules of tricalcium phosphate. It can also be filled with an allograft, which is bone that is grafted from another patient. The bone will eventually grow through the cage and fuse the vertebrae.
- Medical-grade screws with or without a plate may be used to add stability to the spine.
- The surgeon will do another x-ray to confirm the position of the cage, plate, and screws, and to check the alignment of the spine.
- The incision is closed with dissolving sutures, staples, or glue.
What Happens After The Surgery
Here’s what happens after the surgery:
- You will be allowed to move around a few hours after surgery and this is encouraged to prevent the development of blood clots.
- Four hours after surgery, you may be allowed to drink and eat small amounts. It may be slightly difficult to swallow since the surgery involves the throat and neck region. However, this will resolve after a couple of days.
- Pain medications are usually started after surgery.
- Once you are comfortable you will be discharged and sent home.
When To Choose ACDF Surgery
ACDF surgery is recommended by surgeons for many patients who experience pain caused by a pinched nerve. Since there are so many advances in grafting technology, the techniques used for ACDF surgery may vary.
Advances In Bone Graft Technology
Bone graft technology is constantly changing as new advances are made. In the last decade, various bone graft options have emerged. They are listed below:
- Autograft Bone: Autograft bone is bone that is grafted from and used by the same person. This has the highest rate of fusion as it has the highest percentage of biological factors required for a functional graft. The graft usually comes from the fibula or the iliac bone.
- Allograft Bone: Allograft bone is bone that is grafted from another person, usually during their knee or hip replacement surgery. This can reduce surgery time but is usually more expensive.
- Bone Graft Substitute: The third graft option is a composition of various synthetic materials that can substitute autografts. The composite materials are made of light and less dense cancellous bone packed into cages.
There are two different types of cages: plastic or metal. The plastic, or polyetheretherketone, cages are packed with materials such as cancellous autobone, demineralized bone matrix (DBM), or ceramics, and are as rigid as bone.
In contrast, the metal cages are made of stainless steel, titanium, and tantalum, and are packed with autobone taken from the iliac crest of your own hip.
Typical Results And Success Rates For ACDF Surgery
Studies have shown that the overall success rate for patients undergoing ACDF is typically about 50%. However, if a two-level disc ACDF is done, the success rate is about 34.2% (1).
Another result of undergoing ACDF surgery is that the use of pain medications for the primary disease that was affecting the disc decreased significantly after recovery. Additionally, neurological deficits were completely resolved after the ACDF surgery and 88% of patients in the study were happy with their ACDF surgery.
However, 19% of patients had some morbidity or complications with their surgery (2). In general, resolution of symptoms lasted for about 7-10 years. However, the pain returned with the degeneration of other discs, especially in the case of DDD.
It’s important to remember that the success of the surgery depends on many factors, including the extent of degeneration, the skill of the surgeon, the type of graft, and the general medical condition of the patient.
In some cases, if the primary fusion from the ACDF surgery is not successful, a revision surgery may be necessary. Whilst this is rare, it’s important to be aware that this is a possibility.
What Are The Complications Of ACDF Surgery?
There are many potential complications of ACDF. Some of them are listed below:
- Failure Of Surgery: There is a chance that the fusion can fail. A history of steroid use, poor bone quality, smoking, prior surgeries, and even genetics can negatively influence the outcome of ACDF surgery.
- Abnormal Curving Of The Spine: In patients who have lax ligaments, there can be abnormal curving of the spine. This includes forward exaggeration (called kyphosis) or backward exaggeration (called lordosis), and atlantoaxial subluxation.
- Hardware Fracture: The hardware can loosen or may even fracture, requiring a revision surgery.
- Bone Graft Migration: The graft can get extruded if plates and screws were not used to fix the graft or if there were multiple discs that were replaced. The graft can move out of the intended position within just a few weeks or over the course of a few years. Revision surgery is needed to fix this.
- Adjacent Segment Disease: About 3% of patients develop adjacent segment degenerative arthritis changes within 10 years (3). These are degenerative changes that occur near the fusion level.
The movement of the vertebrae above and below the fusion can become restricted, forcing the neighboring vertebrae to compensate. As a result of the extra forces, the adjacent vertebrae and discs may degenerate faster after ACDF surgery.
- Other Complications: Other complications of the surgery include dysphagia or difficulty of swallowing, hematoma formation, muscle pain, recurrent laryngeal nerve palsy (which can present as hoarseness of voice), dura mater tears, and CSF leaks (which can lead to brain infection).
Additionally, complications include wound infection (which can cause septic shock), radiculopathy and neurological symptoms like paralysis, and esophageal perforation (food escaping the GI tract into the chest and abdomen). All of these complication can be life-threatening conditions and require medical help immediately.
Can The Pain Come Back?
There is a possibility that pain can recur in the months or even years after ACDF surgery. In the short term, the pain may be a result of the surgery itself, but post-operative pain usually resolves within a few weeks.
However, the pain may also be accompanied by worsening myelopathy (a condition where the spinal cord is compressed) in the long term.This may be caused by the development of fibrous tissue which can trap or impinge the nerve. If the graft fails to take, then the myelopathy can worsen over time. This can take months and years to develop as the bone heals.
The results of ACDF may last for about 7-10 years. It is possible after 10 years that the graft may loosen or extrude, which can cause pain again due to compression of the spinal cord and the nerve roots.
Why ACDF Surgery May Not Be Your Answer
While ACDF can successfully alleviate painful symptoms for a while, it is not always the best solution for cervical pain. Here are a few reasons why:
- Invasive Procedure: ACDF is an invasive procedure that involves general anesthesia and can lead to doctor- or treatment-induced complications.
- Inconsistent Results: There is a high percentage of morbidity with the ACDF surgery. Not all of ACDF surgeries are successful and the results differ according to age, previous medical history, and the skill of the surgical team.
Nearly 19% of individuals undergoing ACDF have morbidities following the surgery, which negatively affects the recovery and long-term results of the surgery.
- High Incidence Of Complications: There is a long list of complications from ACDF surgery. Dura tears, CSF leaks, recurrent laryngeal nerve palsy leading to hoarseness, difficulty swallowing, kyphosis, and adjacent segment disease are just some of the complications a patient can develop after the procedure.
- Possibility Of Repeat Surgery: Failure of the fusion, cervical instability, and worsening myelopathy can lead to the possibility of a revision or repeat surgery. A second invasive procedure comes with a higher chance of complications and a higher chance of fibrosis, which may complicate the second surgery itself.
Are There Better Alternative Treatment Options?
There are better alternatives to ACDF surgery. These are safer and have less side effects. They are not offered everywhere, but at Centeno Schultz Clinic (CSC) our doctors love to consider these options for people with intervertebral disc disease. You can try these treatments before surgery and see if they help. Some of them are listed below:
Platelet-Rich Plasma (PRP)
PRP for cervical radiculopathy has become very popular for patients with neck pain. It involves using platelet-rich plasma from the patient (to reduce the change of any reaction), which the doctor injects into the intervertebral disc space.
This PRP concentrate is rich in platelets and platelet growth factors that can stimulate other cells to repair and grow, promoting local tissue healing.
The best thing about PRP is that it has very few side effects or complications when compared to ACDF. It is also a quicker procedure and encourages the body to heal itself with platelet growth factors.
At Centeno-Schultz, we continue to innovate and have advanced PRP to now platelet lysate (currently in our 4th generation) for these advanced cervical procedures! Platelet lysate provides multiple benefits as compared to regular PRP:
- Safer to use as compared to PRP in the cervical spine, PRP are stipped of the platelet shells and isolated concentration of immediate release growth-factors
- The quantity of growth factors are much higher which provides a greater probability of success!
Be Informed Of The Consequences Of ACDF
There are many pros and cons of ACDF surgery. Patients are usually recommended anterior cervical discectomy and fusion surgery for cervical radiculopathy if their symptoms are very severe.
However, there are many factors to consider before the surgery, including age, history of steroid use, history of previous surgeries, history of radiation, and morbidity. Since there are many complications of ACDF, your doctor should inform you of the risks before undertaking the procedure.
However, there are also better alternatives available. Regenerative therapies are safer as they use your own cells to naturally facilitate healing. Talk to your doctor about PRP to see if they offer this therapy. If they don’t, get in touch with our doctors at CSC to discuss your regenerative therapy options.
Invasive surgery isn’t always the best option for your pain. Consult our team to learn about all your options.

Christopher J. Centeno, MD
Christopher J. Centeno, M.D. is an international expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate in orthopedics.
Dr. Centeno is one of the few physicians in the world with extensive experience in the culture expansion of and clinical use of adult bone marrow concentrate to treat orthopedic injuries. His clinic incorporates a variety of revolutionary pain management techniques to bring its broad patient base relief and results. Dr. Centeno treats patients from all over the US who travel to Colorado to undergo innovative, non-surgical treatments. Dr. Centeno has chaired multiple international research-based conferences. He also maintains an active research-based practice, with multiple publications listed in the US National Library of Medicine. Dr. Centeno has also served as editor-in-chief of a medical research journal dedicated to traumatic injury.
Dr. Centeno trained at the Baylor College of Medicine, Texas Medical Center, and the Institute for Rehabilitation Research. He hails from both Florida and New York and currently resides in Boulder, Colorado with his wife and three children.

John Schultz, MD
John R. Schultz M.D. is a national expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate for orthopedic injuries. He is board certified in Anesthesiology and Pain Medicine and underwent fellowship training in both. Dr. Schultz has extensive experience with same day as well as culture expanded bone marrow concentrate and sees patients at the CSC Broomfield, Colorado Clinic, as well the Regenexx Clinic in Grand Cayman. Dr. Schultz emphasis is on the evaluation and treatment of thoracic and cervical disc, facet, nerve, and ligament injuries including the non-surgical treatment of Craniocervical instability (CCI). Dr. Schultz trained at George Washington School of…
Read more
John Pitts, M.D.
Dr. Pitts is originally from Chicago, IL but is a medical graduate of Vanderbilt School of Medicine in Nashville, TN. After Vanderbilt, he completed a residency in Physical Medicine and Rehabilitation (PM&R) at Emory University in Atlanta, GA. The focus of PM&R is the restoration of function and quality of life. In residency, he gained much experience in musculoskeletal medicine, rehabilitation, spine, and sports medicine along with some regenerative medicine. He also gained significant experience in fluoroscopically guided spinal procedures and peripheral injections. However, Dr. Pitts wanted to broaden his skills and treatment options beyond the current typical standards of care.
Read more
Jason Markle, D.O.
Post-residency, Dr. Markle was selected to the Interventional Orthopedic Fellowship program at the Centeno-Schultz Clinic. During his fellowship, he gained significant experience in the new field of Interventional Orthopedics and regenerative medicine, honing his skills in advanced injection techniques into the spine and joints treating patients with autologous, bone marrow concentrate and platelet solutions. Dr. Markle then accepted a full-time attending physician position at the Centeno-Schultz Clinic, where he both treats patients and trains Interventional Orthopedics fellows. Dr. Markle is an active member of the Interventional Orthopedic Foundation and serves as a course instructor, where he trains physicians from around the world.
Read more
Brandon T. Money, D.O., M.S.
Dr. Money is an Indiana native who now proudly calls Colorado home. He attended medical school at Kansas City University and then returned to Indiana to complete a Physical Medicine and Rehabilitation residency program at Indiana University, where he was trained on non-surgical methods to improve health and function as well as rehabilitative care following trauma, stroke, spinal cord injury, brain injury, etc. Dr. Money has been following the ideology behind Centeno-Schultz Clinic and Regenexx since he was in medical school, as he believed there had to be a better way to care for patients than the status quo. The human body has incredible healing capabilities…
Read moreReferences
- Radcliff K, Davis RJ, Hisey MS, et al. Long-term Evaluation of Cervical Disc Arthroplasty with the Mobi-C© Cervical Disc: A Randomized, Prospective, Multicenter Clinical Trial with Seven-Year Follow-up. Int J Spine Surg. 2017;11(4):31. Published 2017 Nov 28. doi:10.14444/4031
- Fountas KN, Kapsalaki EZ, Nikolakakos LG, et al. Anterior cervical discectomy and fusion associated complications. Spine (Phila Pa 1976). 2007;32(21):2310-2317. doi:10.1097/BRS.0b013e318154c57e
- Cho SK, Riew KD. Adjacent segment disease following cervical spine surgery. J Am Acad Orthop Surg. 2013;21(1):3-11. doi:10.5435/JAAOS-21-01-3
Am I a Candidate?
To answer this question, fill out the candidate form below to request a new patient evaluation, and a patient advocate will reach out to you to determine your next steps. Your one-hour, in-office or telemedicine evaluation will be with one of the world’s experts in the field of Interventional Orthopedics.