Any kind of spinal surgery is a scary thought. Each week we evaluate and see patients dealing with neck pain for weeks to months and some, many years—failing multiple treatments for their disc herniations, annular tears, and overall degenerative spine conditions.
Many patients are seeking an alternative to cervical disc replacement surgery. So today, let’s dig into what an Artificial Disc Replacement (ADR) is; is it a good option compared to other cervical spine surgeries such as fusions, and do we have a good alternative….!
Understanding What Disc Replacement Surgery On Your Neck Is
In the 1980s, Dr. Karin Büttner-Janz, a German surgeon, developed the first ball-and-socket artificial disc, which was implanted into a patient’s cervical spine in 1984. This design provided a greater range of motion than previous implants but was also associated with high implant migration and subsidence rates.
In the early 2000s, several new cervical disc replacement systems were developed that incorporated newer materials and designs to improve outcomes. In 2007, the FDA approved the first cervical disc replacement system for use in the United States, the Prestige Cervical Disc, manufactured by Medtronic.
Since then, the FDA has approved several other cervical disc replacement systems, including the Mobi-C and ProDisc-C, designed to mimic the natural movement of the cervical spine.


The Purpose of Cervical Disc Arthroplasty
Also known as cervical disc replacement is a surgical procedure designed to alleviate neck pain and other symptoms caused by a herniated disc, annular tears, and degenerative discs that fail conservative treatments.
Types Of Cervical Disc Replacement Surgery
Several types of cervical disc replacement surgery are available. The most common types of cervical disc replacement include:
- One-level disc replacement: This surgery involves replacing a single cervical disc with an artificial disc implant. It is the most common type of cervical disc replacement surgery and is often recommended for patients with a single level of disc degeneration or herniation.
- Two-level disc replacement: In some cases, patients may have degeneration or herniation in two adjacent cervical discs. In these cases, a two-level disc replacement surgery may be recommended, which involves replacing both discs with artificial disc implants.
Most surgeons will not replace 3 levels because additional levels add to the instability of the cervical spine. - Hybrid surgery: Hybrid surgery involves combining cervical disc replacement with a cervical fusion procedure. This may be recommended for patients with more extensive damage or instability in the cervical spine that cannot be fully addressed with disc replacement alone.
- Revision surgery: Sometimes, patients may undergo revision surgery to replace an existing artificial disc implant that has failed or become displaced.
The type of cervical disc replacement surgery recommended will depend on the patient’s needs and the extent of the cervical spine damage or degeneration. Patients need to discuss the different options with their surgeons and weigh the benefits and risks of each approach before making a decision.
The Conditions That Artificial Cervical Disc Replacement Can Be A Help To
While our job is to help patients get back to their lives without the need for invasive surgeries-there are always situations that need surgery. Here are a few examples of what we are looking for as indications that surgery may be a better option than injection-based treatment
Herniated Disc
A cervical herniated disc, also known as a slipped or ruptured disc, occurs when the soft, jelly-like material inside a cervical disc in the neck protrudes through a tear or crack in the disc’s outer layer.
This alone can cause various types of pain but would not warrant surgery. It’s when there is weakness in the arms or hands and difficulty with fine motor skills.
The severity of symptoms can vary depending on the location and size of the herniation and the extent of nerve or spinal cord compression. But progressive weakness from a disc herniation is an indication for a surgical referral!
Spine Myelopathy
Radiculopathy is when nerves are irritated for various reasons, such as disc herniations or other degenerative conditions that pressure the spine’s nerves. But when that progresses to nerve compression, we start to get nerve damage that results in weakness in the arms and, in some cases, can even cause weakness in the legs. This is known as cervical myelopathy.
Spinal Stenosis
Cervical spinal stenosis is when the spinal canal in the neck region narrows, leading to compression or irritation of the spinal cord and nerves. Symptoms may include neck pain, weakness, numbness in the arms or legs, and even paralysis in severe cases.
Patients can manage mild cases without surgery, but severe cases may require surgery to relieve pressure on the spinal cord when symptoms progress from pain/numbness to functional decline and progressive weakness (myelopathy); that is when surgery is needed!
Cervical Radiculopathy And Artificial Disc Replacement
Cervical radiculopathy is a condition characterized by nerve root compression or irritation in the cervical spine. ADR surgery may be an effective treatment option in some cases, but not all patients may be good candidates for the procedure.
Other more conservative treatment options are likely to be effective before you should have surgery.
The Procedure Of Replacing The Disc In Your Cervical Spine
The surgical approach for cervical spine ADR typically involves the following steps:
- Anesthesia: The patient is given general anesthesia, which means they are asleep during the procedure.
- Incision: The surgeon makes a small incision in the front of the neck, typically on the side opposite the affected disc.
- Exposure: The surgeon carefully moves aside the muscles, blood vessels, and other tissues to expose the affected cervical disc.
- Removal of the damaged disc: The surgeon removes the damaged or degenerated disc and any bone spurs or other tissue that may be compressing the nerves or spinal cord.
- Insertion of the artificial disc: The surgeon inserts the artificial disc implant into the space where the damaged disc was removed. The implant is typically made of metal or a combination of metal and plastic and is designed to mimic the natural movement and function of the cervical spine.
- Closure: The incision is closed with sutures or staples, and a bandage or dressing is applied to the neck.
Following the procedure, patients typically stay in the hospital for a day or two and may need to wear a neck brace or collar for several weeks to support healing. Physical therapy and other rehabilitation may also be recommended to help restore strength, mobility, and function in the neck.
The Challenges Of Cervical Disc Replacement Surgery
While this technology is still new, the promise from surgeons and the companies that are producing the device touted it as a solution to the ASD – adjacent segment disease that comes with fusion of the cervical spine: learn more about adjacent segment disease here.
In reality, that didn’t happen, but it has reduced ASD. Research has shown that ACDF (anterior cervical discectomy with fusion) can result in ASD 7-8 out of 10 times…ADR has reduced this to 5-6 out of 10 times. BUT hasn’t eliminated ASD as promised!
The Complications Of A Disc Replacement Surgery On Your Neck
Like any surgical procedure, it does carry some potential risks and complications. Some of the possible complications associated with cervical disc replacement include:
- Infection: As with any surgical procedure, there is a risk of infection at the surgical site. Antibiotics can treat this but may require additional surgery to remove infected tissue.
- Nerve damage: The spinal cord and nerves in the neck are delicate structures, and there is a risk of damage during surgery. This can cause symptoms such as pain, weakness, or numbness in the arms or legs.
- Implant failure: The artificial disc implant may loosen or fail over time, which can cause pain, instability, and other symptoms.
- Bleeding: There is a risk of bleeding during or after the procedure, which may require additional treatment or surgery.
- Allergic reaction: Some patients may be allergic to the materials used in the artificial disc implant.
- Difficulty swallowing: Some patients may experience difficulty swallowing after the procedure.
Cervical Artificial Disc Replacement Recovery Time
In the immediate postoperative period, patients may experience some discomfort and swelling at the surgical site and may need to wear a neck brace or collar for several weeks to months to support the healing process.
Patients may also need to participate in physical therapy and rehabilitation to regain strength, mobility, and function in the neck.
While recovery can be faster than traditional fusion, it can still take up to 3 months to return to full activity.
Why You Should Not Take This Treatment
Several contraindications or factors may make cervical artificial disc replacement (ADR) surgery inappropriate or less effective for certain patients. Some of these contraindications may include the following:
- Severe osteoporosis: Patients with severe osteoporosis, a condition characterized by weak and brittle bones, may not be good candidates for ADR surgery.
- Spinal deformity: Patients with significant spinal deformities, such as scoliosis, may not be good candidates for ADR surgery.
- Infection: Patients with an active infection, such as a spinal infection, may need to wait until the infection has cleared before undergoing ADR surgery.
- Allergies: Patients allergic to the materials used in the artificial disc implant may not be good candidates for ADR surgery.
- Pregnancy: Women who are pregnant or planning to become pregnant may need to delay ADR surgery until after giving birth.
- Prior cervical spine surgery: Patients who have undergone cervical spine surgery may not be good candidates for ADR surgery due to the risk of scar tissue and other complications.
Why You Might Want To Take This Treatment
With my patients, there is only one reason to have surgery – if there is a progressive weakness in the arm or leg associated with the disc herniation or disc injury. When patients present with these symptoms, I recommend going straight to a surgeon for an evaluation.
BUT IMHO, that is not that often, and I see many patients getting operated on far too soon. While pain and limitations are difficult, setting someone up for the possible need for multiple surgeries down the road isn’t good medicine!
Artificial Disc Replacement Vs. Anterior Cervical Discectomy And Fusion (ACDF), What Is Better For You?

ACDF is a disc replacement with a fusion all at the same time! This only makes sense if there is significant instability in the spine, and fusion is the only option! Most likely myelopathy (spine cord damage) cases; otherwise, the long-term consequences of ASD are not worth it!
Regenerative Treatments As Alternatives To This Surgery
Over the last decade, great strides have been made to understand disc injuries and, more importantly, how to heal them! PRP = Platelet Rich Plasma is a growth factor-rich injectate that can stimulate healing in disc injuries.
There have been randomized controlled trials on using PRP for lumbar discs showing excellent results with long-term follow-ups. As well as dosing studies show: the BIGGER the dose – the BETTER the results can be!
Click this link to understand PRP better.
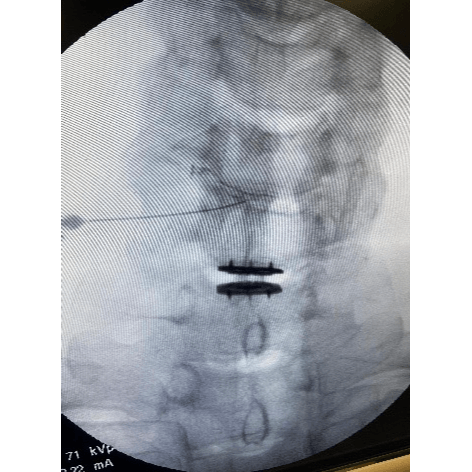
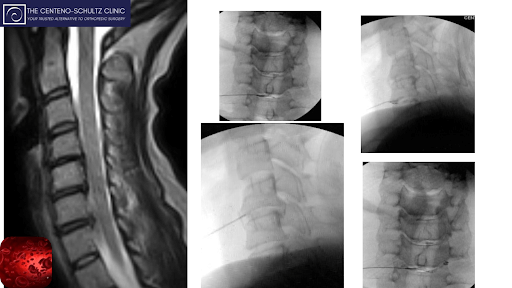
While most current research is for the lumbar spine, cervical spine discs can be saved as well! The problem with cervical spine is the access to the disc takes expert-level skill with both ultrasound guidance and fluoroscopy to guide the needle into the disc while avoiding vital neurovascular structures.
Luckily at The Centeno Schultz Clinic, we have two of a handful of physicians in the country capable of doing this. Dr. Jason Markle and Dr. John Pitts have pioneered disc treatments with excellent success.
If you or any loved one has been dealing with a cervical disc injury and looking to avoid surgery. Give us a call and set up an evaluation with one of our cervical disc experts. We can discuss if you are a candidate for intradiscal PRP!
Epidural PRP
https://centenoschultz.com/epidural-injections/
Regenerative Treatment
https://centenoschultz.com/epidural-injections/
What can we do to help you with your spine injury?

Christopher J. Centeno, MD
Christopher J. Centeno, M.D. is an international expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate in orthopedics.
Dr. Centeno is one of the few physicians in the world with extensive experience in the culture expansion of and clinical use of adult bone marrow concentrate to treat orthopedic injuries. His clinic incorporates a variety of revolutionary pain management techniques to bring its broad patient base relief and results. Dr. Centeno treats patients from all over the US who travel to Colorado to undergo innovative, non-surgical treatments. Dr. Centeno has chaired multiple international research-based conferences. He also maintains an active research-based practice, with multiple publications listed in the US National Library of Medicine. Dr. Centeno has also served as editor-in-chief of a medical research journal dedicated to traumatic injury.
Dr. Centeno trained at the Baylor College of Medicine, Texas Medical Center, and the Institute for Rehabilitation Research. He hails from both Florida and New York and currently resides in Boulder, Colorado with his wife and three children.

John Schultz, MD
John R. Schultz M.D. is a national expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate for orthopedic injuries. He is board certified in Anesthesiology and Pain Medicine and underwent fellowship training in both. Dr. Schultz has extensive experience with same day as well as culture expanded bone marrow concentrate and sees patients at the CSC Broomfield, Colorado Clinic, as well the Regenexx Clinic in Grand Cayman. Dr. Schultz emphasis is on the evaluation and treatment of thoracic and cervical disc, facet, nerve, and ligament injuries including the non-surgical treatment of Craniocervical instability (CCI). Dr. Schultz trained at George Washington School of…
Read more
John Pitts, M.D.
Dr. Pitts is originally from Chicago, IL but is a medical graduate of Vanderbilt School of Medicine in Nashville, TN. After Vanderbilt, he completed a residency in Physical Medicine and Rehabilitation (PM&R) at Emory University in Atlanta, GA. The focus of PM&R is the restoration of function and quality of life. In residency, he gained much experience in musculoskeletal medicine, rehabilitation, spine, and sports medicine along with some regenerative medicine. He also gained significant experience in fluoroscopically guided spinal procedures and peripheral injections. However, Dr. Pitts wanted to broaden his skills and treatment options beyond the current typical standards of care.
Read more
Jason Markle, D.O.
Post-residency, Dr. Markle was selected to the Interventional Orthopedic Fellowship program at the Centeno-Schultz Clinic. During his fellowship, he gained significant experience in the new field of Interventional Orthopedics and regenerative medicine, honing his skills in advanced injection techniques into the spine and joints treating patients with autologous, bone marrow concentrate and platelet solutions. Dr. Markle then accepted a full-time attending physician position at the Centeno-Schultz Clinic, where he both treats patients and trains Interventional Orthopedics fellows. Dr. Markle is an active member of the Interventional Orthopedic Foundation and serves as a course instructor, where he trains physicians from around the world.
Read more
Brandon T. Money, D.O., M.S.
Dr. Money is an Indiana native who now proudly calls Colorado home. He attended medical school at Kansas City University and then returned to Indiana to complete a Physical Medicine and Rehabilitation residency program at Indiana University, where he was trained on non-surgical methods to improve health and function as well as rehabilitative care following trauma, stroke, spinal cord injury, brain injury, etc. Dr. Money has been following the ideology behind Centeno-Schultz Clinic and Regenexx since he was in medical school, as he believed there had to be a better way to care for patients than the status quo. The human body has incredible healing capabilities…
Read moreReferences:
(1) MacDowall A, Canto Moreira N, Marques C, Skeppholm M, Lindhagen L, Robinson Y, Löfgren H, Michaëlsson K, Olerud C. Artificial disc replacement versus fusion in patients with cervical degenerative disc disease and radiculopathy: a randomized controlled trial with 5-year outcomes. J Neurosurg Spine. 2019 Jan 11;30(3):323-331. doi: 10.3171/2018.9.SPINE18659. PMID: 30641852.
(2) Wachowski MM, Weiland J, Wagner M, Gezzi R, Kubein-Meesenburg D, Nägerl H. Kinematics of cervical segments C5/C6 in axial rotation before and after total disc arthroplasty. Eur Spine J. 2017 Sep;26(9):2425-2433. doi: 10.1007/s00586-017-5073-z. Epub 2017 Apr 4. PMID: 28378073.
(3) Yang X, Janssen T, Arts MP, Peul WC, Vleggeert-Lankamp CLA. Radiological follow-up after implanting cervical disc prosthesis in anterior discectomy: a systematic review. Spine J. 2018 Sep;18(9):1678-1693. doi: 10.1016/j.spinee.2018.04.021. Epub 2018 May 8. PMID: 29751126.
(4) MacDowall A, Skeppholm M, Lindhagen L, Robinson Y, Löfgren H, Michaëlsson K, Olerud C. Artificial disc replacement versus fusion in patients with cervical degenerative disc disease with radiculopathy: 5-year outcomes from the National Swedish Spine Register. J Neurosurg Spine. 2018 Nov 2;30(2):159-167. doi: 10.3171/2018.7.SPINE18657. PMID: 30485205.
(5) Chang CC, Huang WC, Wu JC, Mummaneni PV. The Option of Motion Preservation in Cervical Spondylosis: Cervical Disc Arthroplasty Update. Neurospine. 2018 Dec;15(4):296-305. doi: 10.14245/ns.1836186.093. Epub 2018 Dec 14. PMID: 30545210; PMCID: PMC6347355.
(6) Gao X, Yang Y, Liu H, Meng Y, Zeng J, Wu T, Hong Y. A Comparison of Cervical Disc Arthroplasty and Anterior Cervical Discectomy and Fusion in Patients with Two-Level Cervical Degenerative Disc Disease: 5-Year Follow-Up Results. World Neurosurg. 2019 Feb;122:e1083-e1089. doi: 10.1016/j.wneu.2018.10.231. Epub 2018 Nov 9. PMID: 30415055.
(7) Spivak JM, Zigler JE, Philipp T, Janssen M, Darden B, Radcliff K. Segmental Motion of Cervical Arthroplasty Leads to Decreased Adjacent-Level Degeneration: Analysis of the 7-Year Postoperative Results of a Multicenter Randomized Controlled Trial. Int J Spine Surg. 2022 Feb;16(1):186-193. doi: 10.14444/8187. Epub 2022 Feb 17. PMID: 35177528.
(8) Lutz G. Platelet-rich plasma as a potential treatment for degenerative disc disease: a review of the current literature. Current Orthopaedic Practice. 2016;27(6):601-606.
(9) Lutz G. Platelet-rich plasma therapy for degenerative disc disease: a case report. Journal of Chiropractic Medicine. 2016;15(4):289-294.
(10) Lutz G. Platelet-rich plasma as a treatment for chronic low back pain: a prospective, randomized controlled trial. BMC Musculoskeletal Disorders. 2019;20(1):510.
(11) Lutz G. Intradiscal platelet-rich plasma therapy for lumbar discogenic low back pain: preliminary results from a prospective, randomized, double-blind, placebo-controlled trial. Pain Medicine. 2020;21(11):e558-e567.
Am I a Candidate?
To answer this question, fill out the candidate form below to request a new patient evaluation, and a patient advocate will reach out to you to determine your next steps. Your one-hour, in-office or telemedicine evaluation will be with one of the world’s experts in the field of Interventional Orthopedics.