Knee Cartilage Surgery: Know All The Facts
Am I a Candidate?Damage to the cartilage of the knee is related to injury, increasing age, higher body mass index, and knee contractures (1). In the past, surgery was the only viable treatment option.
However, with recent developments in orthopedics, several non-surgical alternatives, like mesenchymal stem cell (MSC) therapy, have proven to be just as effective as surgery in some patients, if not better. Let’s delve deeper into the treatment options for knee cartilage injuries.
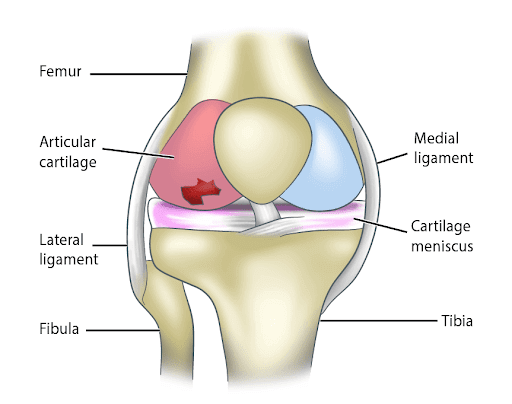
What Is Knee Cartilage?
Knee cartilage is a type of dense connective tissue found in the knee that provides a protective surface for the joint. It is composed of cells called chondrocytes and, unlike other tissues, articular cartilage does not contain blood vessels. As a result, knee cartilage has poor regenerative qualities.
Types Of Cartilage
There are three types of cartilage in the human body: hyaline cartilage, elastic cartilage, and fibrocartilage. Hyaline cartilage is usually found in the growth plate of bones and the ends of the rib. Elastic cartilage is found in the larynx and the ear. It is the fibrocartilage that forms the articular surfaces of bones.
In the knee, articular cartilage lies between the femur and the tibia. The menisci are also made of fibrocartilage. Fibrocartilage is made of type II collagen. It also contains proteoglycans, chondrocytes, and water. In healthy articular cartilage, there is a constant balance between these components, so cartilage degradation and synthesis are well matched.
This balance is carefully maintained by a matrix of enzymes called metalloproteases (MMPs). These enzymes play a huge role in the formation and degradation of cartilage.
The Function Of The Cartilage
Cartilage serves many functions in the body, whether that is fibrocartilage, elastic, or hyaline cartilage. They are listed below:
- Reduces Friction: Cartilage acts like a lubricant for your joints. In the knee, it helps your bones slide without grinding on each other. This smoothens the movement and reduces wear and tear.
- Absorbs Shock: Cartilage cushions the bones and joints. For example, the C-shaped menisci in the knee absorb shock across the knee joint. At the site where the femur and tibia articulate, the menisci also disperse compressive forces during knee movements and transmit it towards the larger bones.
- Supports The Joints: Hyaline cartilage also supports the joint. In the knee, the cartilage is the connective tissue that holds the joint together by connecting to the many tendons, ligaments, bones, and muscles of the joint.
What Can Damage The Cartilage In The Knee?
The articular cartilage and menisci in the knee can be damaged during specific movements, activities, or by certain conditions. The following is a list of the possible causes of knee cartilage damage:
- Osteoarthritis: Osteoarthritis is a common condition that affects the cartilage in the knee. It occurs when cartilage degradation is more rapid than cartilage synthesis. This disrupts the balance between the two, leading to a breakdown of cartilage, pain, and reduced range of motion.
We also now know that damage to the bone underneath the cartilage (subchondral bone) plays a role in cartilage injury.
Other forms of arthritis, like psoriatic arthritis and rheumatoid arthritis, have a similar effect, as the synovial lining of the joint is first attacked and repeated inflammation eventually leads to the destruction of the cartilage.
- Age-related changes: The cumulative effect of years of sustained mechanical load can take a toll on the knees. Alongside this, as you get older there are changes in the articular cartilage.
In combination, the loss of chondrocytes, water, and changes in the matrix play a role in the cartilage becoming thin and stiff, which makes it susceptible to tears and damage.
- Overuse injuries: Overuse injuries, particularly those involving the knee extensor muscles (i.e., the quadriceps) as seen in twisting, jumping, and bending movements, can also damage the knee cartilage over time due to repetitive microtrauma and microtears.
Contact sports and sports where there is rapid acceleration followed by deceleration can also lead to microtears in the cartilage. Microtears can ultimately lead to a partial or full tear in the articular cartilage.
- Osteochondritis dissecans: Osteochondritis dissecans is a condition where a small segment of bone fragments from the surrounding bone due to decreased blood supply. This is most commonly seen in children and adolescents.
Over time, this bone fragment can completely separate, altering the articular surface in the knee. This leads to pain in the joint and decreased range of motion.
- Patellofemoral defects: Patellofemoral defects can be caused by an injury, such as patella dislocation. Patella dislocation can damage the articular cartilage in the knee (especially in violent sporting accidents) where the dislocation occurs. Recurrent injuries can worsen these defects and make them more prone to osteoarthritis.
5 Surgical Procedures To Repair Damaged Knee Cartilage
To repair damaged knee cartilage, there are several different surgical techniques and procedures. Here are the top five surgical procedures for repairing articular knee cartilage:
1. Microfracture Surgery
Knee cartilage surgery used to be the only treatment option for damaged knee cartilage. Short of a total knee replacement surgery, the most common knee surgery to repair knee cartilage was microfracture surgery.
Microfracture surgery is an arthroscopic knee surgery where small fractures are created in the bone with a surgical pick. These small fractures cause the bone deep to the cartilage to release bone marrow cells that can help repair or rebuild local damaged cartilage.
However, it has been shown that most of the cartialged formed after micro farcture is fibrocartilage which is not the desired hyaline cartilage that works best for the knee joint.
This procedure has other limitations as well. It has been found to be less effective in patients who are older, overweight, and have cartilage damage larger than 2.5 cm (2). Apart from pain post-operatively, the most significant drawback from microfracture surgery is that crutches are needed for four to six weeks, alongside daily physical therapy.
2. Cell-Based Cartilage Resurfacing
Cell-based cartilage resurfacing is a novel treatment for repairing cartilage in the knee. It is a process of harvesting, growing, and re-implanting cartilage cells into the knee. Autologous chondrocytes are first taken from another part of the knee with healthy cartilage.
Then, they are grown in a lab under special conditions and introduced into the cartilage of the knee via arthroplasty or open surgery.
This treatment is reserved for small cartilage defects less than 3cm. It is a complicated procedure and recovery can take anywhere from six to eight weeks. Additionally, the surgery can fail if the graft does not “take.”
3. Mosaicplasty
Mosaicplasty is a technique where cylindrical osteochondral plugs are harvested from other low weight-bearing areas in the knee joint. The area of the chondral defect is prepared, with perpendicular vertical edges of normal cartilage around it.
Doctors use the harvested plugs to fill the chondral defect, creating a “mosaic” pattern (hence the name). Any gaps in between the plugs get filled in by fibrocartilage. This can be done via open surgery or arthroscopy.
This procedure is quite technical as it requires special equipment, and because there is considerable difficulty restoring the articular surface due to the cartilage height differences between the defect and the surrounding native cartilage.
After the surgery, it will be four weeks before you can start walking with crutches and partially load the knee. By weeks five to six, you will be able to fully load the knee and walk without crutches. For a full recovery, to return back to competitive sports, it can take as long as six months since cartilage does not have any blood supply.
4. Osteochondral Allograft Transplantation
Osteochondral allograft transplantation (OATS) is a technique that uses the full thickness of viable hyaline cartilage graft from a donor for transplant. The graft typically comes from a cadaver. Fresh frozen allografts are harvested within 21 days from a cadaver in this technique.
Osteochondral allograft transplantation is a good option in younger individuals with defects greater than 3cm. However, it is not advisable for those with advanced degenerative arthrosis or advanced multi-compartmental arthrosis.
It is also relatively contraindicated in individuals with inflammatory arthropathies, obesity, altered bone metabolism due to chronic steroid use, and alcohol abuse.
Primarily, the operation is used for patients who need a salvage procedure due to previous failed restoration treatments. Other conditions where it is used are osteonecrosis, post-traumatic osteochondral defects, osteochondritis dissecans, and patellofemoral arthrosis.
5. Meniscus Transplant
Meniscal allograft transplantation (MAT) is another surgical procedure used in individuals with meniscal damage under the age of 50. The graft comes from a cadaver donor and patients are size matched.
MAT can be completed via mini-open or arthroscopic procedures. However, it cannot be done in patients with an active infection, severe osteoarthritis, malalignment, instability, or inflammatory arthropathy.
While many patients report a significant improvement in the movement of their knee after a MAT, there are high rates of reoperation. Reoperation rates are estimated to be around 32% due to complications. The most common MAT complication is a tear of the meniscal allograft.
Why Knee Cartilage Surgery Is Not Always The Best Option
The number of surgeries for knee cartilage damage significantly outweighs the number of cartilage repair and regenerative medicine techniques used (3).
In many cases, the latter is not even offered to patients. However, orthopedic doctors worldwide and the experts at Centeno-Schultz Clinic (CSC) are moving away from surgery for knee cartilage damage for a few key reasons:
Knee Cartilage Surgery Is Invasive
Most surgical procedures are invasive. A few of them can be done via arthroscopy but, for best results, they are more commonly done via open procedures. The more invasive the surgery, the higher the chances of bleeding, infection, pain, and scarring.
There are also significant risks associated with anesthesia, post-surgery recovery, and pain medications.
Surgeries Are Costly
Knee cartilage surgery is more expensive than regenerative techniques. Knee surgery can range anywhere from $5,000 to $23,000 on average. Add to this the cost of prescription pain medications, antibiotics, additional office visits, and pre-surgical testing, and it shows knee surgery is a very costly process.
Conversely, regenerative medicine is available at a fraction of that cost, with the lowest being $1000 depending on the needs of your knee and what injury you have.
Long Recovery Times
On average, it can take six to eight weeks to move normally after surgery without help from someone or a crutch. However, it can take much longer to make a full recovery. You will also need a dedicated rehab plan to restore strength and movement in the knee post-operatively.
Increased Chances Of Complications
There are lots of complications associated with knee cartilage surgery. The most significant among them is graft failure and the need to reoperate. Higher rates of reoperation lead to higher morbidities and increased inflammation. This puts a person at a greater risk for osteoarthritis in the future.
When it comes to the knee, long-term treatment options like regenerative medicine are the better choice as they do not require corrective surgery, they have less complications, and they have higher success rates than most surgical options.
Non-Surgical Therapy
There are various non-surgical options available at Centeno-Schultz for patients with damaged knee cartilage, including regenerative options.
Regenerative Therapies at the Centeno-Schultz Clinic
There are two different sources of stem cells: bone marrow and fat. Of the two, MSCs from bone marrow have a better research for regeneration capability for cartilage growth.
As a result, at Regenexx, which is the name of the regenerative therapy for orthopedics, bone marrow aspiration concentrate (BMAC) containing stem cells is used for knee cartilage repair.
These cells are injected via percutaneous injections directly into the area of cartilage damage and often also into the subchondral bone. It has been shown that injecting the bone improved outcomes for cartilage defects (4).
In addition, platelet rich plasma (PRP) that has growth factors are injected along with the cells to increase the activity of cells in the injured tissues. The procedures cause pain and inflammation for a few days but recovery is very quick and there is no real “down time.” The procedure is safe and effective, with little risks of complications.
With this method, there is a significant decrease in the need for surgery or total knee replacement in the future, which means it is a suitable procedure for older patients who are not candidates for surgery and in cases where it will be more effective than a graft procedure.
Mesenchymal Stem Cells (MSCs)
The best non-surgical option to treat damaged knee cartilage is cultured autologous mesenchymal stem cells (MSCs), a type of stem cell therapy. MSCs can naturally transform into a host of tissues including bone, cartilage, and fibrous tissue.
Unlike knee cartilage surgery, this procedure is performed using a small needle that is directed under x-ray into the affected area. As a result, recovery time is significantly different than surgery as the patient can bear weight on the affected limb without crutches after just 5-7 days.
In animal studies, it has been demonstrated that MSCs can help repair cartilage (5). A published case report also showed successful cartilage growth in human knees using this procedure (6).
These cultured stem cell procedures are not available in the US any longer unfortunately due to FDA regulations. This has nothing to do with its safety or efficacy but the FDA classifies cultured stem cells as a drug requiring lengthy and very expensive drug trials.
There are some trials underway but can be several years before that process is complete and approved. In the meantime, the doctors at the Centneo Schultz clinic travel to Grand Cayman (link to Cayman website Stem Cell Therapy For Knees | Regenexx Cayman) where their FDA equivalent allows for this more advanced stem cell procedure. In this way patients can still have access to this advanced regenerative care with US physicians.
Knee Cartilage Surgery Is Not Your Only Option Anymore
At CSC, our board-certified doctors will assess your knee and determine if you are a suitable candidate for regenerative medicine treatments. These newer treatments are becoming the treatment of choice because they are safe, effective, and can help heal your knee cartilage without the need for invasive procedures.
Cartilage regeneration technology has the potential to repair cartilage defects and prevent the progression of debilitating cartilage damage.
Costly and complicated surgeries are no longer your only option for knee pain. Check out the other non-surgical treatments available at our clinic!

Christopher J. Centeno, MD
Christopher J. Centeno, M.D. is an international expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate in orthopedics.
Dr. Centeno is one of the few physicians in the world with extensive experience in the culture expansion of and clinical use of adult bone marrow concentrate to treat orthopedic injuries. His clinic incorporates a variety of revolutionary pain management techniques to bring its broad patient base relief and results. Dr. Centeno treats patients from all over the US who travel to Colorado to undergo innovative, non-surgical treatments. Dr. Centeno has chaired multiple international research-based conferences. He also maintains an active research-based practice, with multiple publications listed in the US National Library of Medicine. Dr. Centeno has also served as editor-in-chief of a medical research journal dedicated to traumatic injury.
Dr. Centeno trained at the Baylor College of Medicine, Texas Medical Center, and the Institute for Rehabilitation Research. He hails from both Florida and New York and currently resides in Boulder, Colorado with his wife and three children.

John Schultz, MD
John R. Schultz M.D. is a national expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate for orthopedic injuries. He is board certified in Anesthesiology and Pain Medicine and underwent fellowship training in both. Dr. Schultz has extensive experience with same day as well as culture expanded bone marrow concentrate and sees patients at the CSC Broomfield, Colorado Clinic, as well the Regenexx Clinic in Grand Cayman. Dr. Schultz emphasis is on the evaluation and treatment of thoracic and cervical disc, facet, nerve, and ligament injuries including the non-surgical treatment of Craniocervical instability (CCI). Dr. Schultz trained at George Washington School of…
Read more
John Pitts, M.D.
Dr. Pitts is originally from Chicago, IL but is a medical graduate of Vanderbilt School of Medicine in Nashville, TN. After Vanderbilt, he completed a residency in Physical Medicine and Rehabilitation (PM&R) at Emory University in Atlanta, GA. The focus of PM&R is the restoration of function and quality of life. In residency, he gained much experience in musculoskeletal medicine, rehabilitation, spine, and sports medicine along with some regenerative medicine. He also gained significant experience in fluoroscopically guided spinal procedures and peripheral injections. However, Dr. Pitts wanted to broaden his skills and treatment options beyond the current typical standards of care.
Read more
Jason Markle, D.O.
Post-residency, Dr. Markle was selected to the Interventional Orthopedic Fellowship program at the Centeno-Schultz Clinic. During his fellowship, he gained significant experience in the new field of Interventional Orthopedics and regenerative medicine, honing his skills in advanced injection techniques into the spine and joints treating patients with autologous, bone marrow concentrate and platelet solutions. Dr. Markle then accepted a full-time attending physician position at the Centeno-Schultz Clinic, where he both treats patients and trains Interventional Orthopedics fellows. Dr. Markle is an active member of the Interventional Orthopedic Foundation and serves as a course instructor, where he trains physicians from around the world.
Read more
Brandon T. Money, D.O., M.S.
Dr. Money is an Indiana native who now proudly calls Colorado home. He attended medical school at Kansas City University and then returned to Indiana to complete a Physical Medicine and Rehabilitation residency program at Indiana University, where he was trained on non-surgical methods to improve health and function as well as rehabilitative care following trauma, stroke, spinal cord injury, brain injury, etc. Dr. Money has been following the ideology behind Centeno-Schultz Clinic and Regenexx since he was in medical school, as he believed there had to be a better way to care for patients than the status quo. The human body has incredible healing capabilities…
Read moreReferences
- Ciccotti MC, Kraeutler MJ, Austin LS, et al. The prevalence of articular cartilage changes in the knee joint in patients undergoing arthroscopy for meniscal pathology. Arthroscopy. 2012;28(10):1437-1444. doi: 10.1016/j.arthro.2012.02.029
- Mithoefer K, McAdams T, Williams RJ, Kreuz PC, Mandelbaum BR. Clinical efficacy of the microfracture technique for articular cartilage repair in the knee: an evidence-based systematic analysis. Am J Sports Med. 2009;37(10):2053-2063. doi:10.1177/0363546508328414
- Zamborsky R, Danisovic L. Surgical Techniques for Knee Cartilage Repair: An Updated Large-Scale Systematic Review and Network Meta-analysis of Randomized Controlled Trials. Arthroscopy. 2020;36(3):845-858. doi:10.1016/j.arthro.2019.11.096
- Hernigou Study Hernigou, P., Bouthors, C., Bastard, C., Flouzat Lachaniette, C. H., Rouard, H., & Dubory, A. (2020). Subchondral bone or intra-articular injection of bone marrow concentrate mesenchymal stem cells in bilateral knee osteoarthritis: what better postpone knee arthroplasty at fifteen years? A randomized study. International Orthopaedics. doi:10.1007/s00264-020-04687-7)
- Le H, Xu W, Zhuang X, Chang F, Wang Y, Ding J. Mesenchymal stem cells for cartilage regeneration. J Tissue Eng. 2020;11:2041731420943839. Published 2020 Aug 26. doi:10.1177/2041731420943839
- Martín, A.R., Patel, J.M., Zlotnick, H.M. et al. Emerging therapies for cartilage regeneration in currently excluded ‘red knee’ populations. npj Regen Med 4, 12 (2019). https://doi.org/10.1038/s41536-019-0074-7
Am I a Candidate?
To answer this question, fill out the candidate form below to request a new patient evaluation, and a patient advocate will reach out to you to determine your next steps. Your one-hour, in-office or telemedicine evaluation will be with one of the world’s experts in the field of Interventional Orthopedics.