
L5 S1 fusion is a major surgery typically used to treat severe spinal conditions like degenerative disc disease, herniated discs, or instability. It involves the permanent joining of the lumbar vertebrae (L5) and the sacral vertebra (S1). This procedure is invasive and may lead to complications like nerve damage, extended recovery time, and significant risks, such as infection.
Although this surgery is recommended in cases of disability caused by chronic low back pain, alternatives like those offered at the Centeno-Schultz Clinic can help patients reduce the need for surgery.
How The Spinal Fusion L5 S1 Procedure Works
Spinal fusion is a major surgery where one or more spinal bones (vertebrae) are fused together using screws, bolts, and/or plates. The hardware may be placed in the front (anterior) or the back (posterior) of the spine. The disc between the spinal bones is often removed and replaced with bone or a spacer.There are five spinal bones in the low back, numbered from top to bottom, L1, L2, L3, L4, and L5. Sandwiched between each pair of spinal bones is a disc. The disc is named after the two spinal bones it is sandwiched between.
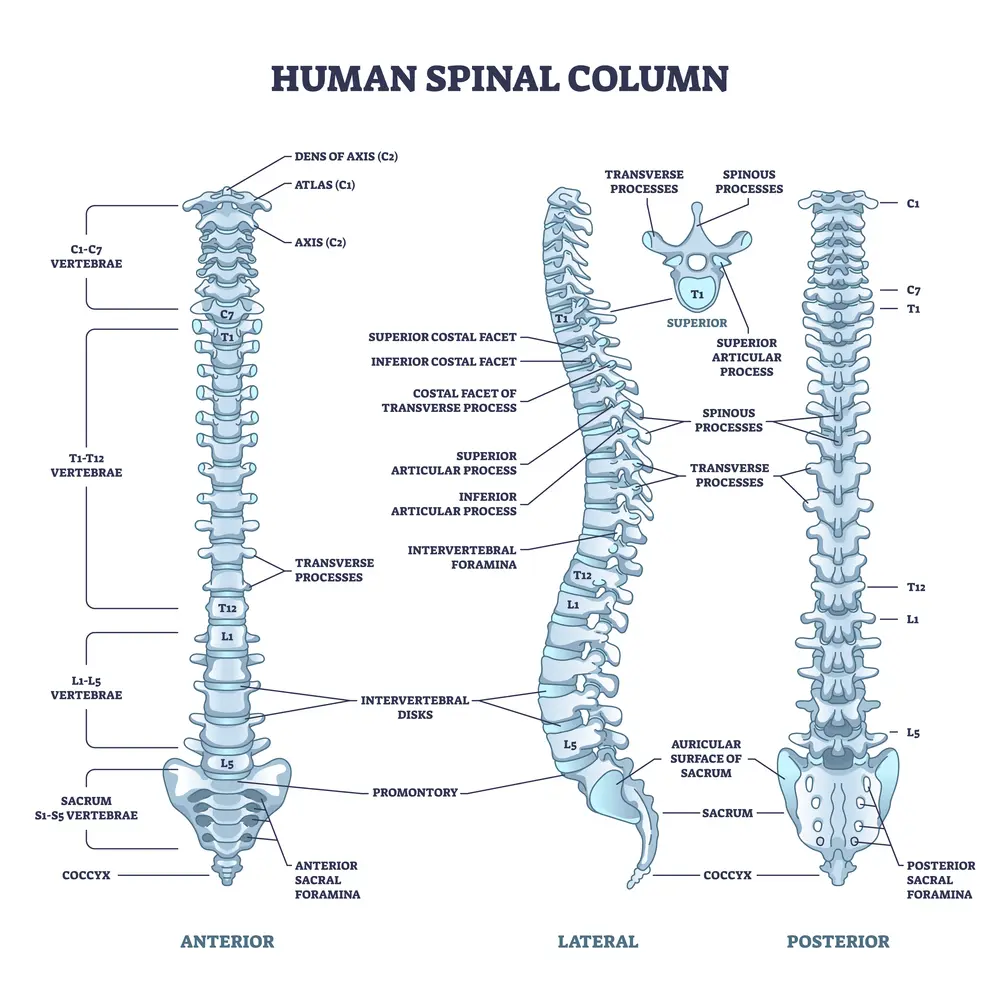
For example, the lowest disc in the low back is the L5/S1 disc. The L5/S1 disc is sandwiched between the L5 and S1 spinal bones. Therefore, L5 S1 fusion surgery involves the surgical removal of the L5/S1 disc and fusing the L5 and S1 spinal bones together. Different surgical techniques and approaches exist. One of these is PLIF, posterior lumbar interbody fusion, which has been reviewed in detail in a previous blog.
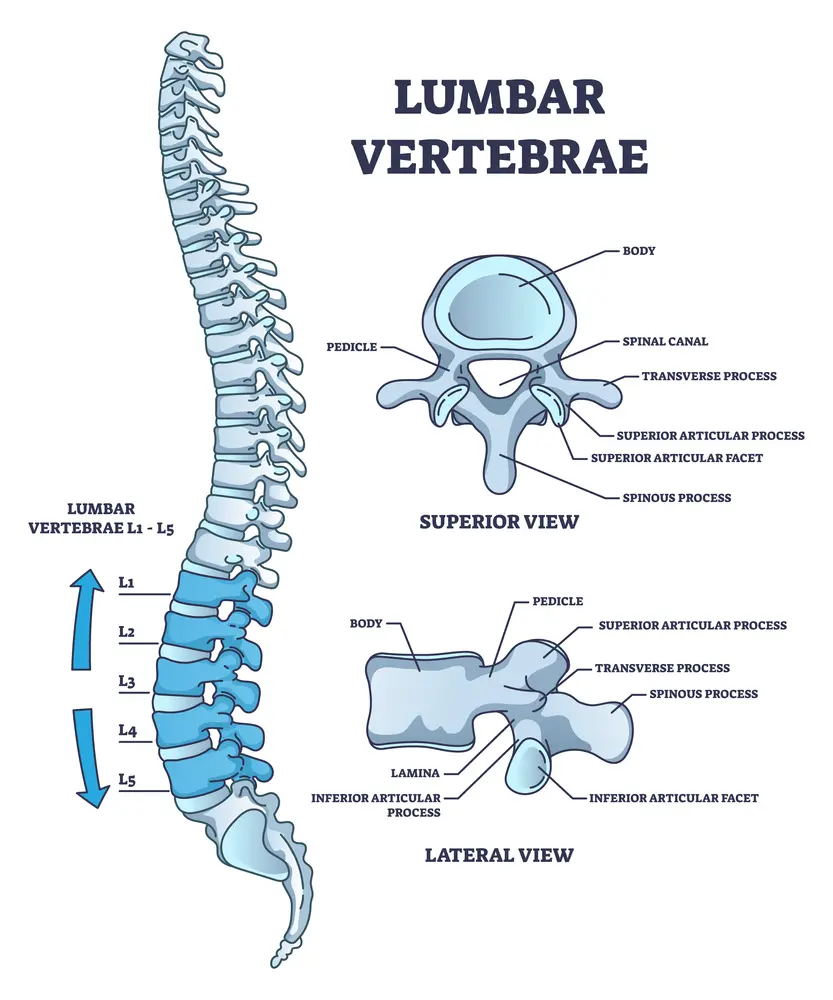
The surgery involves cutting through important muscles, ligaments, and tendons to access the targeted disc. The disc is then removed, and the area is packed with bone and sometimes a spacer. To stabilize the spine, screws are placed into the spinal bones above and below the disc that is removed. The screws are stabilized by additional hardware, including plates and rods.
Conditions Treated By L5 S1 Spinal Fusion
Lumbar fusion is a popular surgery. Between 1998 and 2008, the yearly number of lumbar fusion surgeries performed in the United States increased from 77,682 to 210,407 (1). Lumbar fusion may be recommended for the treatment of several painful and degenerative conditions in the low back.
The most common indications for L5 S1 fusion include:
- Low back disc degeneration
- Slipped disc or spondylolisthesis
- Spinal bone fracture
- Recurrent disc herniation
- Pain radiating down the leg or sciatica
- Side bending in the spine or scoliosis
- Narrowing of the canal or stenosis
- Failed spine surgery with instability
Spondylolisthesis
Spondylolisthesis means that one vertebra is slipping forward or backwards on another. This causes the hole where the nerve exits (foramen) to get smaller (also called foraminal stenosis). It also causes more wear and tear on the facet joint which can lead to arthritis or what’s called “facet hypertrophy”. spondylolisthesis recovery The amount of slippage is graded 1-4, with grade 1 meaning that the one vertebra has slipped up to 25% on the other vertebra. Grade 2 means that one bone has slipped from 25-50% with higher grades indicating more slippage. The vast majority of patients are grade 1 to 2.
Read More About SpondylolisthesisSciatica
Disc herniation, disc protrusion, overgrowth of the facet joint, and thickening of the ligaments can result in nerve root compression or irritation, causing symptoms of sciatic compression. Some causes of sciatic compression can be interrelated with the following conditions: Degenerative disc disease, Spinal stenosis, damage or injuries to the discs, spondylolisthesis, piriformis syndrome, osteoarthritis. The symptoms of sciatica include pain in the lower back, buttock, and down your leg, numbness and weakness in low back, buttock, leg, and/or feet, pain increase with movement, “Pins and needles” feeling in your legs, toes, or feet., loss of bowel control, and incontinence. Sciatica can be treated…
Read More About SciaticaDegenerative Scoliosis
Degenerative Scoliosis, also known as Adult-onset Scoliosis, is a medical condition that involves a side bending in the spine. The bending can be mild, moderate, or severe with side-bending to either the right or the left. The term degenerative means generalized wear and tear and is common as we get older. Degenerative scoliosis is the curvature of the spine that occurs as a result of degeneration of the discs, small joints, and building blocks. The Degenerative Scoliosis curve is often located in the low back and forms a ‘C” shape. There is a convex and a concave side. The convex side is the open side where it curves outward.
Read More About Degenerative ScoliosisSpinal Stenosis
Spinal stenosis is the narrowing of the central spinal canal and is a cause of significant pain and disability. Common causes of spinal stenosis include disc protrusion, facet overgrowth and ligamentum flavum thickening. Surgery is often chosen when conservative therapies fail despite the lack of convincing evidence that it is a superior treatment option. Are there alternatives to back surgery for spinal stenosis? Yes. Regenexx DDD utilizes precise platelet injections into the facets, muscles, and ligaments to treat the lumbar stenosis, treating all of the components of the issue, which is crucial. Spinal stenosis is often an age-related condition attributed…
Read More About Spinal StenosisFailed Back Surgery Syndrome
Failed Back Surgery Syndrome also called failed back is a clinical condition in which patients who have undergone low back surgery continue to have pain and dysfunction. Said another way the surgery that was intended to reduce pain and increase function FAILED. That is right, the surgery failed. You had the surgery, struggled with the pain postoperatively, diligently participated in physical therapy and yet the pain and limitation are still there. Unfortunately, this occurs frequently. Estimates range from 20-40% of patients who undergo low back surgery will develop Failed Back Surgery Syndrome. Pain is the most common symptom of Failed Back Surgery Syndrome…
Read More About Failed Back Surgery SyndromeWhen To Consider Spinal Fusion L5 S1
The L5 S1 region of the spine plays a major role in supporting the body’s weight and facilitating movement. This makes it highly susceptible to issues and vulnerabilities, including:
- Wear and tear: Daily activities, heavy lifting, and aging can cause significant stress, leading to gradual deterioration of the discs and joints.
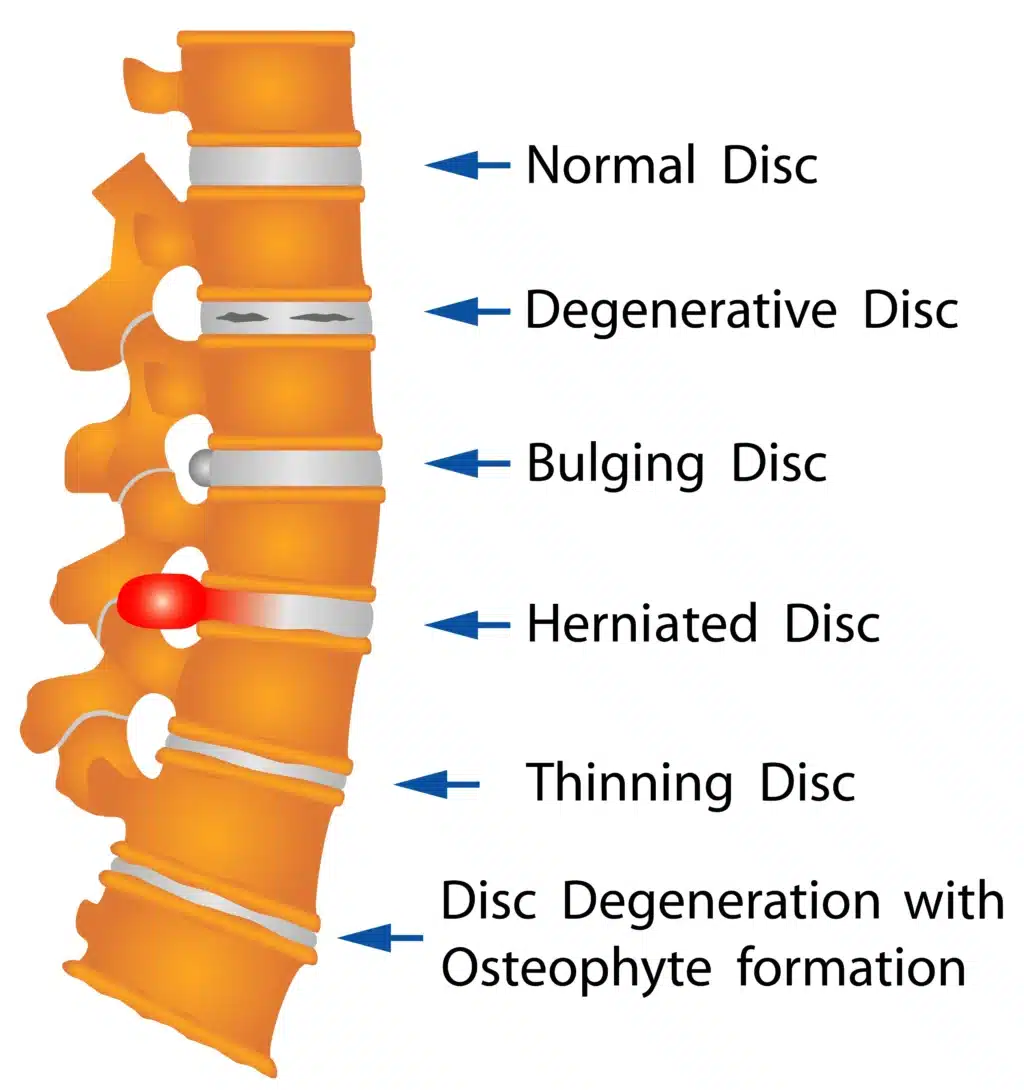
- Disc herniation: The disc between L5 and S1 can become compressed or damaged, leading to reduced cushioning and increased pressure on nearby nerves. Studies estimate that 95% of disc herniations in the lumbar spine affect the L4-L5 or L5-S1 segments.
- Spinal canal narrowing: Over time, the space through which the spinal nerves pass may narrow. This can happen because of inflammation or the development of bone spurs. A narrow spinal canal can press on the spinal nerves, causing pain, numbness, or weakness.
- Facet joint overload: Facet joints are small, stabilizing joints located between two vertebrae, which facilitate spine movement and flexibility. Excessive strain on these joints can lead to pain and instability, making it difficult to move and maintain posture.
Fusion is typically considered when these structural issues severely impact mobility or quality of life and non-surgical treatments have failed to provide relief.
Advantages Of L5 S1 Fusion
Low back pain is considered one of the leading causes of years lived with disability worldwide by a study published in The Lancet in 2021. L5 S1 fusion can offer significant benefits for those with chronic spinal conditions, especially when conservative treatments fail. These include:
- Pain relief: Fusing two vertebrae together eliminates movement and inflammation. This can reduce pain but may significantly impact mobility.
- Improved stability: By stabilizing the spine, fusion helps prevent further damage to surrounding nerves, muscles, and joints.
- Improved function: Although fusion limits movement at the L5 S1 segment, it often improves overall spine function by reducing pain and inflammation.
Risks Of L5 S1 Fusion
While L5 S1 fusion can be beneficial in some cases, it is not without risks. Potential complications include infection, hardware failure, or adjacent segment disease, where nearby spinal levels may become stressed after the fusion.
A 2015 study reports that the rate of complications for this type of surgery is as high as 12.5%, with this figure doubling when both the L5 S1 and the L4 L5 segments require fusion.
Some of the risks of this surgery include:
Non-Union
Non-union occurs when the spinal bones that are bolted together fail to fuse or grow together. Rates vary depending upon the specific type of lumbar spinal fusion procedure. For procedures that require more bone, like a posterior fusion, the non-union rates are as high as 26-36% (5,6).
Hardware Breaking
Lumbar fusion involves using screws, bolts, and plates to stabilize the spinal bones. There are significant forces placed on the low back and the hardware. As a result of these forces, the hardware can break, creating spinal instability and pain.
One study reported the rate of hardware breaking at an alarming 36% (7). Treatment of hardware failure often requires additional surgery to remove the broken hardware and replace it.
Hardware Coming Loose
Screws are used in lumbar fusion to stabilize the spine. The same forces that can cause the hardware to break can also cause the screws to become loose. This, in turn, can create spinal instability and pain. Collectively, about 1 in 10 patients who have a low back fusion will need a second surgery to fix non-union or hardware failure (8).
Complications From L5 S1 Fusion
There are a number of problems that can arise as a result of lumbar fusion itself. The two most important are adjacent segment disease and spinal muscle injury.
Adjacent Segment Disease
Intervertebral discs are important shock absorbers. Fusion surgery removes this important shock absorber, which may place additional stress and forces on the discs and facet joints above and below the level of the fusion. This additional force, in turn, can lead to injury of these facet joints and discs, increasing the risk of degeneration and arthritis. One study reported that this complication occurs in 9% of cases (9). Over time, this can lead to additional surgeries, including fusions. To learn more about this tragic complication please click on the video below.
Spinal Muscle Injury
The spinal muscles provide critical stability and support for the spine. Lumbar fusion can significantly compromise the health and integrity of these muscles. This, in turn, can lead to spine instability and additional injuries, including degeneration and arthritis.
Success Rate Of L5 S1 Fusion
Success, as it relates to spinal fusion surgery, is difficult to judge. This is because there are a significant number of variables involved, including:
- The specific surgical approach
- Preoperative MRI and X-ray findings
- The results from pressuring the disc
- Patient’s age
- Medical history
- Parameters studied
Consider the following results: In one study, 53 patients were followed for an average of 20 months after fusion surgery. In those patients with normal MRIs before the surgery, only 50% improved after surgery (2).
Two years after lumbar fusion, 40% of patients were unsure/dissatisfied with the outcomes, reporting ongoing back pain and limited daily function (3). Another study demonstrated that the overall failure rate of lumbar spine surgery was estimated to be 10%–46% (4).
Long-Term Effects Of L5 S1 Fusion
L5 S1 fusion can have significant long-term effects on both spinal health and overall quality of life. For some, the surgery provides long-lasting relief from chronic pain and allows for improved functionality. However, it is important to understand how fusion impacts the spine and body over time:
- Potential for complications: After the surgery, some patients may experience reduced pain levels. Additionally, the removal of the disc can decrease the risk of degeneration, herniation, and inflammation in the affected spine segment.
However, in the long term, the vertebrae above and below the fused segment may face additional stress, potentially leading to degeneration in these areas. Additionally, patients can face other risks, including failure of the hardware and non-union. These complications can require further surgeries, with associated risks.
- Limited spinal flexibility: Fusion offers stability and reduced pain associated with inflammation. However, the fused segment will no longer be able to move. Unlike other segments of the spine, which are naturally less flexible, the L5 S1 segment is crucial for spine flexibility. This can lead to reduced mobility and can cause the rest of the spine to have to compensate for the loss of movement.
- Extended recovery times: Because of the invasive nature of this surgery, recovery can take up to eight weeks. One study found that, out of several lumbar spine surgery types, fusion is the one requiring the longer recovery times, with patients returning to work on average 90 days after the surgery.
Alternatives To L5 S1 Fusion
At the Centeno-Schultz Clinic, we believe in a comprehensive approach to the treatment of spinal pain. We view and approach the spine as a functional spinal unit. This functional unit includes discs, facet joints, ligaments, fascia, and muscles.
These structures work with one another in a highly specialized and dependent manner. Therefore, for the very best results, the spine and all its parts need to be evaluated and treated together. This novel, comprehensive approach can help you reduce the risk of lumbar fusion and its complications. Treatment options include platelet-rich plasma (PRP). PRP is rich in growth factors that can increase blood flow and healing. To better understand how to avoid lumbar fusions by using precisely guided PRP injections, please click on the video below.
Make Sure To Treat Your Spinal Condition The Best Way
Deciding whether to undergo L5 S1 fusion or explore less invasive options is a critical choice that can greatly impact your long-term health and quality of life.
At the Centeno-Schultz Clinic (CSC), our Functional Spinal Unit approach can help you reduce the need for surgery by supporting the body’s ability to heal naturally. Get in touch with our physicians to learn whether this approach is right for you.
Get a second opinion before getting risky procedures. Contact us today for an appointment.
References
- Rajaee SS, Bae HW, Kanim LE, Delamarter RB. Spinal fusion in the United States: analysis of trends from 1998 to 2008. Spine (Phila Pa 1976) 2012;37:67–76.
- Gill K, Blumenthal SL. Functional results after anterior lumbar fusion at L5-S1 in patients with normal and abnormal MRI scans. Spine. 1992;17(8):940-2.
- Greenwood J, McGregor A, Jones F, Hurley M. Evaluating rehabilitation following lumbar fusion surgery (REFS): study protocol for a randomised controlled trial. Trials. 2015;16:251.
- Thomson S. Failed back surgery syndrome: definition, epidemiology and demographics. Br J Pain. 2013;7:56–59.
- Tsutsumimoto T, Shimogata M, Yoshimura Y, Misawa H. Union versus nonunion after posterolateral lumbar fusion: a comparison of long-term surgical outcomes in patients with degenerative lumbar spondylolisthesis. Eur Spine J. 2008;17(8):1107–1112. doi: 10.1007/s00586-008-0695-9.
- Herkowitz HN, Kurz LT. Degenerative lumbar spondylolisthesis with spinal stenosis. A prospective study comparing decompression with decompression and intertransverse process arthrodesis. J Bone Joint Surg Am. 1991 Jul; 73(6):802-8. https://www.ncbi.nlm.nih.gov/pubmed/2071615/
- Harris IA, Traeger A, Stanford R, Maher CG, Buchbinder R. Lumbar spine fusion: what is the evidence. Intern Med J. 2018;48(12):1430-4.
- Greiner-Perth R, Boehm H, Allam Y, Elsaghir H, Franke J. Reoperation rate after instrumented posterior lumbar interbody fusion: a report on 1680 cases. Spine (Phila Pa 1976). 2004 Nov 15;29(22):2516-20. 9..Okuda S, Yamashita T, Matsumoto T, et al. Adjacent Segment Disease After Posterior Lumbar Interbody Fusion: A Case Series of 1000 Patients. Global Spine J. 2018;8(7):722-7.
Am I a Candidate?
To answer this question, fill out the candidate form below to request a new patient evaluation, and a patient advocate will reach out to you to determine your next steps. Your one-hour, in-office or telemedicine evaluation will be with one of the world’s experts in the field of Interventional Orthopedics.