
Pudendal neuralgia, or cyclist’s syndrome, is a condition characterized by chronic pelvic pain due to compression or irritation of the pudendal nerve. It can result from prolonged activities like cycling, causing discomfort, numbness, and burning sensations. Pudendal neuralgia is frequently misdiagnosed because its symptoms are varied, sometimes resembling those of conditions like sciatica or chronic pelvic pain syndrome.
At Centeno-Schultz Clinic, we emphasize the importance of accurate diagnosis, which can guide personalized treatment plans that target the root cause of pain, not just the symptoms. Our approach utilizes advanced regenerative orthopedic techniques and prioritizes non-invasive, non-surgical methods, aiming to provide effective relief while minimizing risks and reliance on medications.
Why Is Pudendal Neuralgia Difficult to Diagnose?
Accurate diagnosis of pudendal neuralgia is crucial for effective treatment, but many patients face difficulties and delays in getting a proper diagnosis. Research shows that it is often misdiagnosed or missed entirely, resulting in inappropriate treatments and significant delays in symptom management.
These delays can severely impact the quality of life and lead to addiction to medications that don’t address the root of the problem, such as opioids. Some of the reasons why pudendal neuralgia remains difficult to diagnose include:
- Overlapping symptoms: The symptoms of pudendal neuralgia, like pelvic pain, numbness, and burning sensations, often overlap with other conditions, such as sciatica or interstitial cystitis. This makes it difficult to distinguish pudendal neuralgia from these other conditions.
- Limited provider awareness: Many healthcare providers may not be fully aware of pudendal neuralgia or the challenges that come with this condition. This lack of awareness can result in misdiagnosis or a delayed diagnosis. This happens because symptoms are attributed to more common conditions, such as sciatica.
- Varied symptom presentation: Symptoms of pudendal neuralgia can vary widely among individuals. Some may experience burning sensations, while others might feel numbness or a sharp pain. These differences can complicate the diagnostic process, as providers may find it difficult to rule out a range of other possible conditions.
A 2024 study suggests that delays in getting a proper diagnosis when suffering from chronic pelvic pain can lead to ongoing discomfort, reduced physical activity, and unnecessary exposure to high-dose opioids. It can also increase stress and worsen the financial burden.
Commonly Known Symptoms of the Condition
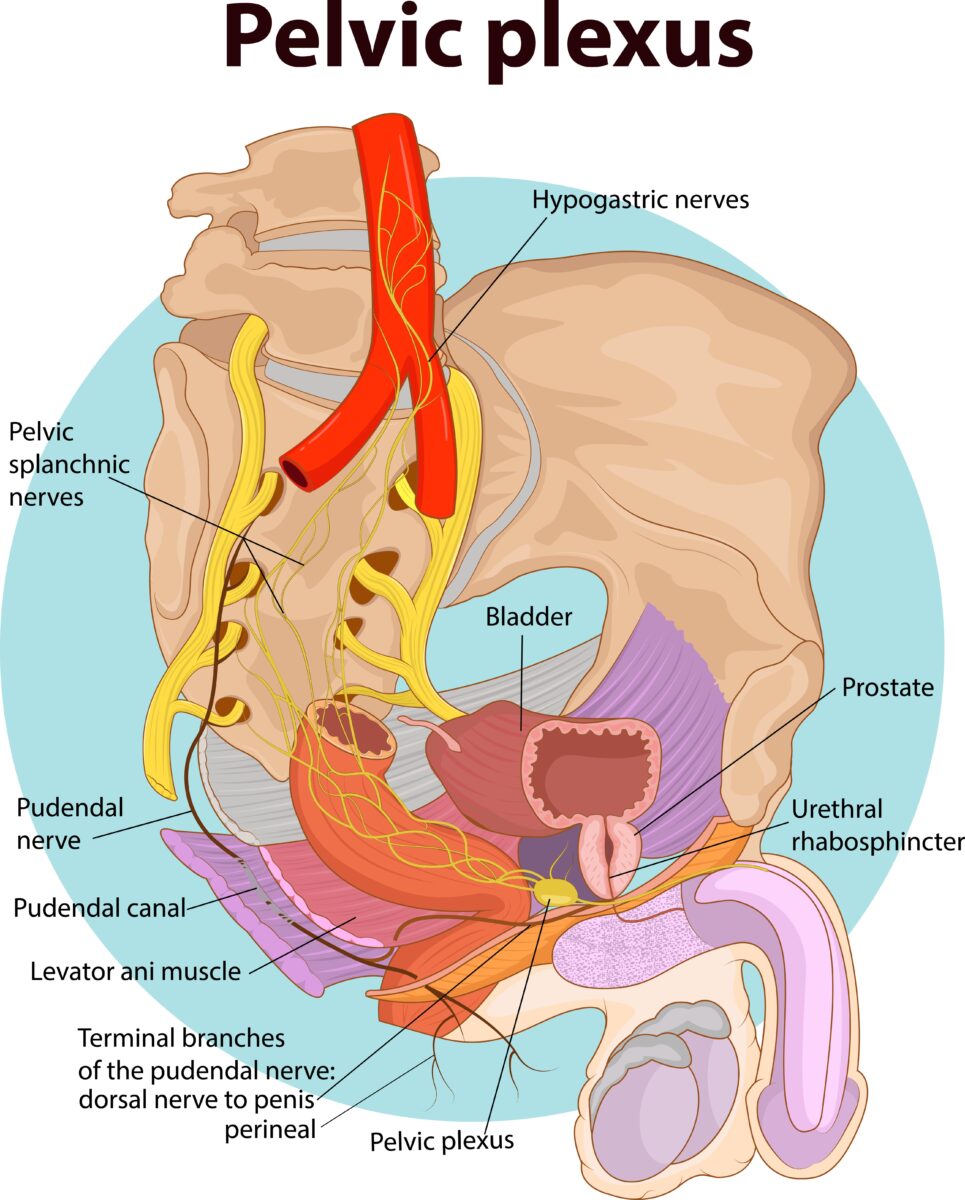
The pudendal nerve is a key nerve in the pelvic region, originating from the spinal nerves S2, S3, and S4. It is responsible for providing sensation and motor control in areas around the genitals and rectum. This nerve controls important functions:
- Sensory function: Provides sensations such as touch and temperature to the genitals and anal area.
- Motor function: Controls muscles in the perineum and pelvic floor, supporting functions like urination and bowel control.
When to See a Doctor for an Accurate Diagnosis
After cycling or other activities that involve prolonged sitting, you might experience minor pain or discomfort, which is often a normal consequence. However, when these symptoms persist or worsen, it may be time to seek a more accurate diagnosis.
Consider seeing a doctor if you experience:
- Pain lasting several weeks: If the pain persists for a few weeks or worsens, it could indicate nerve compression or irritation.
- Increasing discomfort while sitting: If you experience ongoing pain when sitting, it may be because the pudendal nerve becomes increasingly compressed in this position.
- New numbness or tingling: Sudden or increasing numbness and tingling can suggest that the nerve has become more compressed or irritated. Adequate treatment is necessary to prevent further nerve damage.
- Pain disrupting daily activities: If the pain begins to interfere with everyday activities, like walking or working, it is important to not let this issue go untreated. Research suggests that pudendal neuralgia affects around 8% of long-distance cyclists. Due to delays in getting the right diagnosis, athletes suffer from this condition an average of 2-10 years. During this time, both quality of life and sports performance can be affected.
- Emotional distress from symptoms: Persistent symptoms can take a toll on emotional well-being. If you find that your mood and mental health are affected by your symptoms, seeking medical advice can provide relief and guidance.
How Experts Diagnose Pudendal Neuralgia
Healthcare providers use several tools to diagnose the causes of chronic pelvic pain. These include:
- Patient history and symptom assessment: This initial step involves evaluating information about your symptoms, lifestyle, and medical history. This knowledge can help providers identify patterns that may point to pudendal neuralgia.
- Physical examination: During the examination, a healthcare expert will gently palpate areas of the pelvis to check for tenderness and pain, which can indicate nerve issues. This hands-on approach can help identify specific regions where the pudendal nerve may be compressed or irritated.
- Diagnostic nerve block: This technique involves injecting a local anesthetic near the pudendal nerve to temporarily alleviate pain. If the injection works in reducing symptoms, it confirms the involvement of the pudendal nerve.
Other Tests to Confirm Diagnosis
The methods above work as a starting point to diagnose the causes behind pelvic pain. However, often, they are not enough to determine the root cause of pain. This could be because the symptoms of pudendal neuralgia overlap the ones of other conditions or due to the lack of provider awareness.
That is why a more comprehensive approach to the diagnostic process is essential. Alongside the diagnostic tools seen above, a specialist may also use the following tests:
CT Scan
A CT scan uses X-rays to provide detailed cross-sectional images of internal structures, such as the pelvis. This test helps identify structural abnormalities that may trap or place undue stress on the pudendal nerve, such as bone spurs, tumors, cysts, or fractures.
Pudendal Nerve Motor Latency Test (PNMLT)
The PNMLT measures the time it takes for an electrical impulse to travel along the pudendal nerve. The healthcare provider will place electrodes on relevant muscles and then use a mild electric current to stimulate the nerve. This test helps assess the speed and response of the nerve pathway. Delays in nerve conduction can indicate compression or dysfunction.
Electromyography (EMG)
EMG involves inserting a needle electrode into the muscles that are innervated by the pudendal nerve to measure its electrical activity.
This test evaluates muscle response and can detect abnormalities in the nerve or muscles, helping the physician understand how the nerve’s dysfunction is affecting motor control. It can also help distinguish between nerve disorders and problems related to muscles.
3T MRI Scans
3T MRI scans produce highly detailed images using a stronger magnetic field than standard MRIs, which are traditionally used to view soft tissues like ligaments and nerves.
This test helps identify nerve compressions, swelling, or other soft tissue changes that may impact the pudendal nerve. The clarity of 3T imaging makes MRIs more precise and efficient in diagnosing problems with the pudendal nerve and its surrounding structures.
Pudendal Nerve Entrapment Care at Centeno-Schultz Clinic
At Centeno-Schultz Clinic, we are dedicated to providing comprehensive care for pudendal nerve entrapment. Our approach begins with an in-depth diagnostic process to identify the root cause of your pelvic pain. Diagnostic precision will then guide personalized treatment decisions that go beyond easing pain by targeting the reasons behind symptoms and dysfunction.
We prioritize non-invasive treatments and utilize advanced regenerative orthopedics, like platelet lysate therapy, which promotes nerve healing and symptom relief without surgery. We also offer precise, image-guided nerve hydrodissection to reduce nerve compression and inflammation safely.
By focusing on restoring function and alleviating pain, we aim to help you regain your quality of life without the risks, side effects, and downtime associated with traditional approaches.
Take Control of Your Recovery with the Right Diagnosis
Understanding your symptoms is just the first step–identifying the root cause of pain is essential to guide treatment decisions and promote recovery.
At Centeno-Schultz Clinic, we use advanced diagnostic techniques and regenerative orthopedics to address pudendal neuralgia. This ensures not just symptom management but a comprehensive treatment approach tailored to you, helping you return to the activities you love pain-free!
Get focused care treatment for Pudendal Nerve Entrapment. Let the healthcare professionals help you!