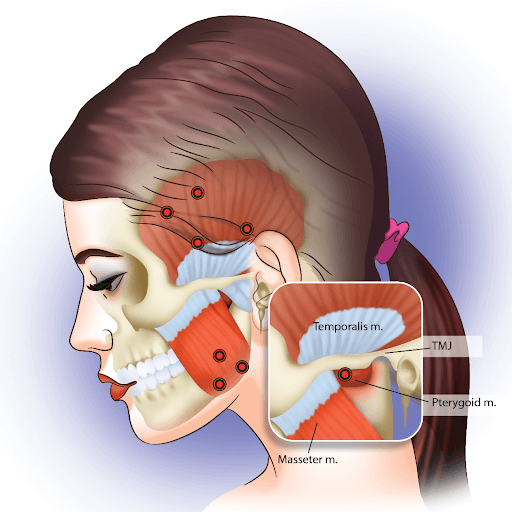
Temporomandibular joint (TMJ) headaches are associated with dysfunction or issues in the temporomandibular joint, which connects the jawbone to the skull. The TMJ serves as the hinge that connects the jawbone to the skull, allowing for essential functions such as chewing, speaking, and yawning. It is a complex joint involving muscles, ligaments, and the jawbone, working together to enable smooth and coordinated jaw movements.
Issues with the TMJ can lead to various symptoms, including headaches, jaw pain, and difficulties in jaw movement. TMJ headaches specifically arise when dysfunction in the TMJ triggers pain that radiates to the head and neck. Let’s delve into the details of TMJ headaches.
What Does a TMJ Headache Feel Like, Compared to Other Tension Headaches?
When experiencing a TMJ headache, the symptoms are distinct from other tension headaches.
- Clicking and popping sound from the mouth: An individual with a TMJ headache may notice unusual sounds, such as clicking or popping when moving their jaw.
- Difficulty and pain while chewing: Chewing can be accompanied by discomfort and difficulty, especially if there is an issue with the temporomandibular joint.
- Aching pain in and around the ears: TMJ headaches often cause aching sensations in and around the ears, reflecting the interconnectedness of the jaw and ear structures.
- Jaw movement difficulties: A limited range of motion or difficulties in moving the jaw smoothly may be experienced during a TMJ headache episode.
- Pain in one or both of the temporomandibular joints: The pain is specifically linked to the temporomandibular joints on one or both sides of the face.
- Changes in the manner of biting: Individuals may notice alterations in how their teeth come together, indicating potential issues with the temporomandibular joint.
- Headache from jaw movements: Headaches are often triggered or exacerbated by jaw movements, distinguishing TMJ headaches from other tension headaches.
- Pain when clenching the teeth: Clenching the teeth, a common symptom of stress, can intensify the pain during a TMJ headache.
Location of TMJ Headaches
TMJ headaches can be differentiated from other headaches by the specific areas where individuals experience pain. Unlike other headaches, TMJ headaches tend to cause discomfort in the following areas:
- Cheeks: TMJ headaches may result in aching sensations in the cheeks, especially around the TMJ region.
- Ears: Pain or aching in and around the ears is a common symptom of TMJ headaches, reflecting the proximity of the temporomandibular joint to the ear structures.
- Jaw: TMJ headaches often manifest as pain or discomfort directly in the jaw, particularly around the temporomandibular joint.
- Other parts of the face: Pain may extend to various areas, not limited to the jaw and cheeks. TMJ-related discomfort can be felt in different facial regions.
- Top of your head: While many headaches may cause pain on the top of the head, TMJ headaches may contribute to or intensify pain in this area, especially if jaw movements are involved.
- Neck pain: TMJ headaches can be associated with neck pain, as the muscles and structures surrounding the jaw and neck are interconnected.
- Shoulder pain: In some cases, individuals with TMJ headaches may experience referred pain that extends to the shoulders, further distinguishing these headaches from other types.
Likely Reasons You Are Experiencing TMJ Headaches
The symptoms of TMJ headaches can be attributed to various causes, and these may include:
- Consistent teeth grinding: Habitual teeth grinding or clenching, often done unconsciously, can lead to excessive strain on the temporomandibular joint, causing headaches.
- Tense jaw muscles: Chronic tension in the muscles surrounding the jaw, which can result from stress, anxiety, or other factors, may contribute to TMJ headaches.
- Misalignment of the jaw: If the jaw joint (temporomandibular joint) is not properly aligned, it can lead to dysfunction and pain, including headaches.
- Uneven bite: Irregularities in the alignment or positioning of the teeth, leading to an uneven bite, can place stress on the temporomandibular joint and trigger headaches.
- Hormonal imbalance: Fluctuations in hormonal levels, particularly in women, may contribute to TMJ issues and associated headaches.
- Mental stress: High levels of stress, anxiety, or emotional tension can lead to increased muscle tension in the jaw and surrounding areas, potentially resulting in TMJ headaches.
- Malocclusion: Abnormalities in the way the upper and lower teeth fit together, known as malocclusion, can be a contributing factor to TMJ headaches.
- Inflammatory conditions: Conditions such as arthritis affecting the temporomandibular joint can cause inflammation and pain, leading to headaches.
- Trauma or injury: Previous injuries to the jaw or head, such as fractures or dislocations, can contribute to TMJ issues and subsequent headaches.
- Genetic factors: There may be a genetic predisposition to temporomandibular joint disorders, increasing the likelihood of experiencing TMJ headaches.
Do TMJ Headaches Go Away on Their Own?
TMJ headaches and associated TMJ issues typically do not resolve on their own without medical intervention. Unlike certain minor aches or pains that might be alleviated with time and rest, TMJ-related problems often require targeted treatment to address the underlying causes and provide relief.
Possible Medical Conditions Causing the Pain
Here are some possible medical conditions that could be causing the pain:
Temporomandibular Disorder (TMD)
Temporomandibular disorder (TMD) refers to a group of conditions affecting the temporomandibular joint and the muscles responsible for jaw movement. TMD can manifest in various ways, causing pain and dysfunction in the jaw, head, and surrounding areas.
It is a degenerative joint disease that can affect the TMJ, causing pain, inflammation, and reduced joint mobility. Excessive joint movement, beyond the normal range, can lead to instability and discomfort in the TMJ. In severe cases, osteoporosis may affect the bones of the TMJ, potentially leading to pain and structural changes.
Bruxism (Teeth Grinding)
Bruxism is a condition characterized by the grinding or clenching of teeth, often occurring involuntarily during sleep. This repetitive behavior can have significant consequences for the jaw and surrounding structures.
Diagnosis and Examination
If you are experiencing symptoms suggestive of a temporomandibular joint disorder, your doctor or dentist will likely follow a systematic approach to diagnose the issue. The diagnosis may involve a combination of physical examination, observation, and imaging studies. Here is an outline of the general diagnostic process:
- Physical Examination:
- Jaw examination: Your healthcare provider will physically examine your jaw, assessing its movement, alignment, and any signs of tenderness or abnormalities.
- Range of motion observation: The healthcare professional will observe how well your jaw moves when you open and close your mouth, checking for any limitations or irregularities.
- Palpation:
- Touching painful regions: The doctor may gently press on specific areas around your jaw, feeling for tenderness, swelling, or discomfort. This helps pinpoint areas that may be affected.
- Diagnostic Imaging:
- Dental X-rays: X-rays are commonly used to examine the teeth and jaw, providing detailed images of the bone structure. This can reveal issues such as misalignment, arthritis, or fractures.
- CT scans: Computed tomography scans offer more detailed images of the bones involved in the joint, providing a clearer picture of structural abnormalities.
- MRI (magnetic resonance imaging): MRI is particularly useful for detecting problems in the TMJ’s soft tissues, including the disks and surrounding structures.
- TMJ Arthroscopy:
- Aid to diagnosis: In some cases, TMJ arthroscopy may be recommended. This involves inserting a thin tube (cannula) into the joint space, followed by a small camera (arthroscope). The arthroscope allows visualization of the joint, aiding in the diagnosis of internal issues.
- Diagnostic benefits: TMJ arthroscopy is useful for assessing the condition of the joint’s interior, and detecting problems that may not be apparent through other diagnostic methods.
- Additional Considerations:
- Medical history: Your doctor may inquire about your medical history, including any history of jaw trauma, dental procedures, or habits such as teeth grinding.
- Collaboration with specialists: In complex cases, your primary care provider may collaborate with specialists such as oral and maxillofacial surgeons or rheumatologists for a comprehensive evaluation.
Common Treatment Options
The following are some common treatment options for TMJ headaches:
Lifestyle and Diet Changes
These changes can relieve TMJ headaches:
- Diet modification: Avoiding hard or chewy foods and opting for a soft diet can reduce strain on the jaw.
- Stress management: Techniques such as relaxation exercises, meditation, and stress reduction can alleviate tension contributing to TMJ headaches.
- Posture improvement: Maintaining good posture and avoiding habits like jaw clenching can positively impact TMJ function.
Medication
Short-term use of NSAIDs, such as aspirin, ibuprofen, or naproxen, can help reduce pain and inflammation associated with TMJ headaches.
Dental and Orthodontic Treatments
Customized oral splints or mouthguards can be designed to alleviate jaw clenching and grinding, reducing TMJ strain.
Therapy
Various therapies can also relieve TMJ headaches. These include:
- Physical therapy: Targeted exercises and manual techniques can improve jaw muscle strength and flexibility and reduce pain. For more information, refer to this related article on the Centeno-Schultz Clinic’s (CSC’s) Physical Therapy.
- Chiropractic care: Some individuals find relief through chiropractic adjustments aimed at improving jaw alignment and reducing tension.
- Ortho-biologic: The Regenexx Procedure offered by the CSC biologics such as bone marrow concentrate or platelet rich plasma (depending on severity). This innovative approach uses the patient’s own blood or bone marrow to promote healing and stability in the affected joint.
Surgical Treatments
While surgical interventions are generally considered a last resort for treating TMJ disorders, they may be recommended in cases where conservative measures have not provided sufficient relief, and the pain persists. Common surgical treatment options include:
- Arthrocentesis: Arthrocentesis involves the insertion of small needles into the joint space to irrigate and remove debris, reducing inflammation and promoting healing. It is used for certain types of TMJ disorders, particularly those involving joint effusion and inflammation.
- Arthroscopy: Arthroscopy involves the insertion of a small camera (arthroscope) into the joint space through a small incision. This allows for visualization of the joint and, in some cases, the performance of minor surgical procedures. It is useful for diagnosing and treating internal derangements of the TMJ.
- Open-joint surgery (arthrotomy): In open-joint surgery, a larger incision is made to directly access the TMJ. This approach allows for more extensive repairs or modifications to the joint. It is reserved for severe cases where other less invasive options have been unsuccessful.
- Joint replacement (prosthetic TMJ replacement): In cases of advanced degeneration or damage, joint replacement may be considered. This involves removing the damaged joint and replacing it with an artificial joint. It is typically considered when other surgical options are not viable, and the joint function is severely compromised.
Exercises You Can Do to Help Your Temporomandibular Joint
These exercises are designed to restore your jaw’s range of motion and alleviate minimal discomfort associated with TMJ issues. It is crucial to perform these exercises cautiously and slowly. If you experience severe pain, it’s advisable to stop, readjust the intensity, or consult your doctor before continuing.
Goldfish Exercise
- Sit or stand in an upright position with your spine straight.
- Keep your mouth closed and lips together.
- Place the tip of your tongue against the roof of your mouth.
- Smile widely without opening your lips.
- Hold the smile for 10 seconds, feeling a gentle stretch in your jaw.
- Relax your jaw and return to the starting position.
- Repeat this exercise 5-10 times.
Mandibular Stabilization Exercise
- Sit or stand comfortably.
- Place your thumb under your chin.
- Gently push your chin downward against the resistance of your thumb.
- Hold the position for 3-5 seconds.
- Release the pressure slowly.
- Repeat this exercise 5-10 times.
Cervical Retraction “Chin Tucks”
- Sit or stand with your spine straight.
- Gently tuck your chin in towards your chest, keeping your back straight.
- Hold the position for 3-5 seconds.
- Relax and return to the starting position.
- Repeat this exercise 5-10 times.
Side-to-Side Jaw Exercise
- Sit or stand comfortably.
- Slowly move your jaw to the right side, maintaining a smooth and controlled motion.
- Hold the position for 3-5 seconds.
- Return your jaw to the center.
- Repeat the same motion to the left side.
- Hold the position for 3-5 seconds.
- Repeat this exercise 5-10 times on each side.
Tongue Up Exercise
- Sit or stand with your spine straight.
- Slowly open your mouth as wide as possible.
- While keeping your mouth open, touch the roof of your mouth with your tongue.
- Hold this position for 5-10 seconds.
- Close your mouth slowly.
- Repeat this exercise 5-10 times.
Improve Jaw Movement and Don’t Leave Symptoms Untreated
The intricacies of how we chew or the tension in our jaw muscles often go unnoticed until our temporomandibular joints start clicking, popping, and triggering relentless headaches. The discomfort of having difficulty chewing or resorting to a liquid diet is not something anyone desires to endure indefinitely.
Therefore, it is imperative to take proactive steps and seek professional evaluation to identify the root cause of your TMJ headaches as soon as possible. Early intervention can pave the way for effective management and relief, ensuring a better quality of life and minimizing the impact of TMJ-related symptoms on your daily activities.
Don’t let TMJ pain linger – consult with your healthcare provider or a specialist in temporomandibular disorders to address your symptoms promptly and embark on a journey towards improved jaw health.
Free yourself from pain and get your symptoms diagnosed. Get yourself an appointment with us.