Baxter’s Neuropathy
Causes, Symptoms, Treatment, & Other Resources
Good afternoon, Dr. Markle of Centeno-Schultz Clinic, and today we’re discussing a condition called Baxter’s Neuropathy. It’s one of the many things that can create some chronic and intense heel pain. So we’ll be discussing
- what exactly causes Baxter’s neuropathy,
- some symptoms, as well as
- some underlying issues that can create it.
And, in addition, discussing some Regenerative Medicine and non-surgical interventional techniques for successful treatment of Baxter’s Neuropathy.
What is Baxter’s Neuropathy?
It is an entrapment syndrome, like carpal tunnel syndrome in your hand. This is an entrapment of a nerve in your foot, right around your heel, on the inside part compressing a branch of your tibial nerve called your inferior calcaneal nerve, and that is the Baxter’s nerve. Now, the inferior calcaneal nerve is the first branch of the lateral plantar nerve, which is a branch off your tibial nerve. It lives between a muscle belly called your abductor hallucis muscle, as well as the medial calcaneal tuberosity, which is a small bump where a common heel spur occurs in the foot.
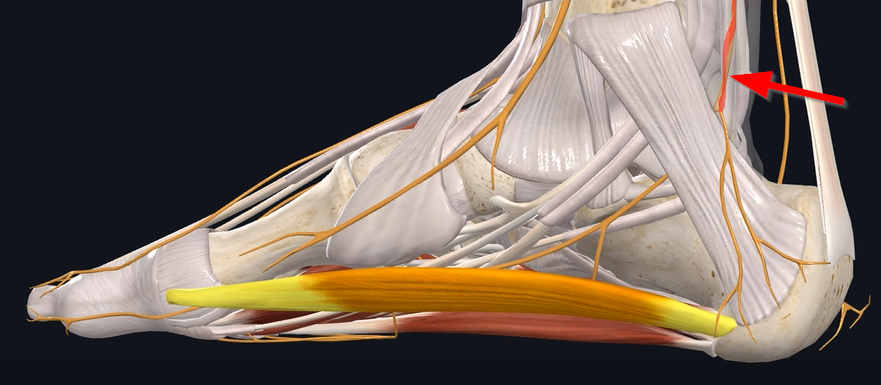
Now, if we look at the way the nerve travels – So the tibial nerve comes down (see Figure 1).
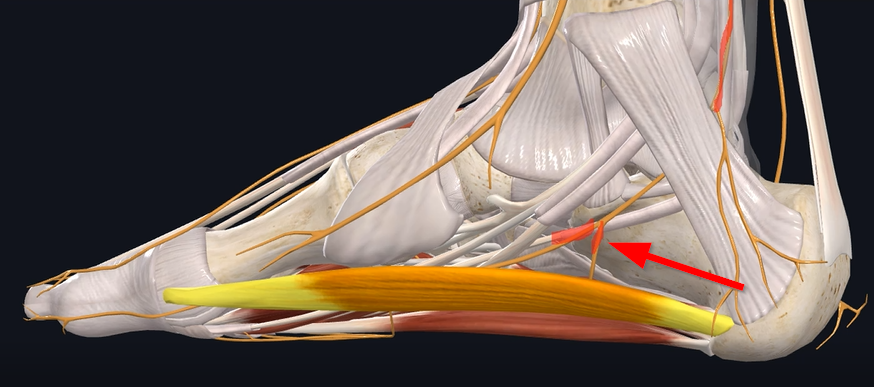
and then branches into your medial and lateral plantar nerve and then the nerve branches again into that Baxter’s nerve (see Figure 2).
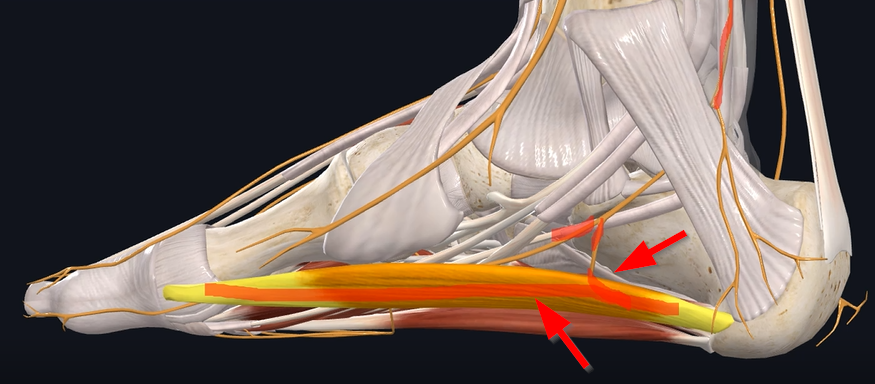
It goes by this muscle right here, which is to your abductor hallucis muscle. And then, after it gets past that muscle, it goes adjacent to your calcaneal tuberosity and your quadratus plantae muscle, which is at the base of the foot right there, and here’s the nerve going right under it, and then it traverses (see Figure 3).
posteriorly around. Sometimes, there are common heel spurs in this area. Those three areas are the main regions and potential entrapments that create the entrapment itself.
Causes of Baxter’s Neuropathy
Now causes of Baxter’s Neuropathy – sometimes you have some predisposing conditions, one such as muscle hypertrophy, meaning if one of those two muscles in the foot become overworked and hypertrophied, they can compress the nerves traveling around it. Obesity can be problematic. Then foot and ankle conditions such as hyper-pronation or flat feet can create some compression of that nerve.
If you have some bone spurs that were created from plantar fasciitis, or just irritation around the nerves, that can also create some bony compression of that nerve.
Symptoms
Now Symptoms. A common – if we are looking at heel pain in general – diagnosis has always been plantar fasciitis. Now plantar fasciitis, typically, historically, has been pain first thing in the morning; you have pain directly into the heel bone. That first step or two in the morning becomes excruciating, and it loosens up as you stretch out the tissue.
Now, Baxter’s neuropathy is the exact opposite – meaning: you really don’t have any pain in the morning but towards the end of the day. Meaning: you’re walking on a nerve that’s getting irritated. So, the more you walk on it, the more that nerve gets irritated. So, pain tends to be at the end of the day. Irritation of that nerve can create some paresthesia, meaning numbness and tingling, along the bottom part of the heel.
As well as from an examination, if you can palpate the course of where the nerve is, you can elicit and aggravate the patient’s pain and replicate it.
Now, if you have these symptoms, how do you prove its back neuropathy?
You can get an x-ray that can show the pathology of a potential bone spur in that area. MRI can show if the muscles have hypertrophied around it, causing some compression of that nerve, as well as compression of the nerve does create some fluid and inflammation around that nerve and some thickening of the fascia itself.
Deeper Dive Into Baxter’s Neuropathy Symptoms
Ankle Pain After Walking
More than any other joint, our ankles bear the burden of all of our body weight. The ankles aren’t large weight-bearing joints, like our hips or knees; comparatively speaking, the ankles are rather small for the tasks they are assigned to do. If the ankles are normal and healthy and there isn’t a weight issue placing excess stress on the ankles, the ankles can typically bear the forces of walking, running, hiking, and so on quite well. However, when the ankles are weak or carrying too much weight, any additional forces placed upon them—even something as simple as walking—can create problems. Do your ankles get sore after walking? What about foot and ankle pain after hiking? If so, it’s a good idea to proactively address it now, before it gets worse, rather than resigning yourself to it and decreasing or stopping the activities you enjoy. We’ll explain more in a moment, but first let’s take a closer look at the structure of the ankle.
Read More About Ankle Pain After WalkingAnkle Pain When Running
There are multiple causes of ankle pain while running. The six major causes are: Stress Fracture A stress fracture is a small crack in the bone due to overuse and repeated impact. They are a common cause of pain in runners, accounting for up to 16% of injuries. The shin bone (tibia) is the most commonly affected bone accounting for approximately 40 % of stress fractures. Pain is the most common symptom. Plantar Fasciitis. The plantar fascia is the thick connective tissue that extends from your heel to your toes. Plantar fasciitis is the inflammation of the plantar fascia and is the most…
Read More About Ankle Pain When RunningPain In The Back Of The Heel
Heel pain can be intense and, despite rest and trying a variety of other conservative measures, it can often also be persistent. Every year, there are over a million visits to primary physicians for plantar heel pain. Plantar heel pain affects both men and women equally, and there are many causes of plantar heel pain. Therefore, it is important to diagnose the cause of the heel pain so that it can be treated appropriately. We will review the causes, complications, and treatment options for plantar heel pain.
Read More About Pain In The Back Of The HeelHow Do You Treat Baxter’s Neuropathy?
One of the common ways would be medications. So typically your primary care physician or physician starts you off on some sort of anti-inflammatory, or if you describe some burning neuropathic pain symptoms, they’ll put you on a neuropathic pain medication such as Gabapentin, Lyrica or a host of any other neuropathic medications. If you have any underlying issues, such as the flat fee or hyper-pronation, there are foot and ankle braces. They can help to help take some pressure off the nerve.
If all those fail, then injection-based treatments would be corticosteroid injections, where if there’s any inflammation around the nerve, those steroids help shut down that inflammation. But the problem with this long-term is it actually is toxic to the nerve cells. So, it could potentially make those symptoms worse, long term-wise, which, when it does come back, it could create damage to the muscles or tendons around it also re-aggravating that area. Opposite to that would be a surgical treatment, which is surgical decompression.
Now, here at Centeno-Schultz Clinic, we pride ourselves as some of the founders of the field of Regenerative Medicine, and, utilizing regenerative medicine such as platelet-rich plasma in the form of a platelet lysate, we’ve been able to utilize this in treating nerve pain for many years. We have published multiple papers, such as sciatica using PRP epidurals in the extremities. A lot of times we use musculoskeletal ultrasound to hydrodissect the nerve with the platelets. And that accomplishes two things at once.
- We’re creating some space around the nerve that was getting entrapped.
- We’re putting growth factors around the nerve to help those nerves repair.
And if one of the issues is a potential bone spur, then we can also utilize a technique called a Tenex Osteotomy, where we take a small device, under ultrasound guidance, and actually, break up the bone spur and remove the bone spur subcutaneously, or percutaneously – meaning through the skin just with a simple needle.
If we look at this video, we can see the nerve in the elbow right here:
And here is the bone spur. And we can see the machine, under ultrasound guidance, breaking up the bone spur. This gentleman was having intense pain in the elbow, as well as numbness and tingling. Within probably a week or two, he was nearly asymptomatic, and the pain has not come back since doing this procedure. Again, this was a combined Tenex procedure to remove the bone spur and then utilizing the PRP as an injectate to hydrodissect the nerve around it and give that nerve some space around it.
So, if you have been dealing with any heel pain issues and numbness and tingling and potentially been diagnosed with Baxter’s neuropathy, give us a call. We are happy to evaluate you either via telemedicine or in-person evaluation and discuss potential treatment options and further evaluate you to see some of the small details of exactly what is causing some of your symptoms.
Nerve Hydrodissection
Nerve Hydrodissection is a medical procedure that aims to free up scar tissue or adhesions on a given peripheral nerve. The procedure utilizes ultrasound guidance to visualize both the needle and the targeted nerve. Medication is then injected through the needle to free up the scar tissue. Nerve Hydrodissection is a minimally invasive treatment option for many peripheral nerves that are compressed or entrapped by scar tissue.Pain is an uncomfortable and at times painful sensation. It varies significantly from patient to patient. There are many different types of pain which include inflammatory, nociceptive, and neuropathic. Neuropathic pain is pain that arises from nerve compression or injury.
Read More About Nerve HydrodissectionNeuro-Prolotherapy (Neural-Prolo)
Neural-Prolo, is also known as Neurofascial Prolotherapy (NPT). Born from traditional prolo-therapy, Neural-Prolo is described as: Subcutaneous peri-neural injection of 5% dextrose. It was created by a New Zealand physician, Dr. John Lyftogt while he was treating a series of Achilles tendon injuries. Similar to how traditional prolotherapy helps strengthen loose ligaments and damaged tendons, Dr. Lyftogt discovered that a low concentration of dextrose (5%) in the subcutaneous tissue can help in resolving chronic nerve inflammation and restoring the normal physiology of the nerve cell. Neuritis is also thought to be a contributing factor to chronic pain syndromes and why sometimes the pain continues…
Read More About Neuro-Prolotherapy (Neural-Prolo)NSAIDs
The other day I was evaluating a patient and reviewing the treatment options for their spine condition. After discussing prior treatments, we got to the topic of medications taken for pain relief. She explained that she mainly utilized anti-inflammatory (NSAID) medications and then she told me to hold much she takes and has been for many years…..she takes close to 2 grams (2000 milligrams) on a daily basis which equated to about 9-10 capsules of medication per day. I was shocked, considering she was pre-diabetic and with high blood pressure plus the kicker of it is that her PCP (primary care physician) is ok with this…
Read More About NSAIDsProlotherapy Injections
It has been successful in the treatment of many disorders including neck, shoulder, knee, and ankle pain. Dr. Centeno recently published an article in The Journal of Prolotherapy in which he discusses the use of x-ray guidance with prolotherapy. This ensures that the injection is in the correct place to maximize clinical results. Dr. Centeno discusses the use of prolotherapy for the treatment of neck, knee, sacroiliac joint, ankle, ischial tuberosity, and shoulder pain. At the Centeno-Schultz Clinic x-ray guided prolotherapy is just one of the therapies utilized in the successful treatment of pain. Regenerative injection therapy (RIT) or prolotherapy…
Read More About Prolotherapy InjectionsPRP for Nerve Damage
Peripheral nerves are comprised of various combinations of motor, sensory, and autonomic neurons. Nerve injuries are a common condition with a broad range of symptoms depending on the severity of nerve damage which presents various challenges to patients, ranging from mild discomfort to life-long impairment. PRP for nerve damage has been shown to be effective. Let’s dig in. Nerve injuries can be classified based on the severity of damage and which structures in the nerve have been damaged. The most severe case is the complete transection of the nerve, called neurotmesis. The most common is neuropraxia from acute or chronic compression of the nerve.
Read More About PRP for Nerve DamagePRP Injections
PRP is short for platelet-rich plasma, and it is autologous blood with concentrations of platelets above baseline values. The potential benefit of platelet-rich plasma has received considerable interest due to the appeal of a simple, safe, and minimally invasive method of applying growth factors. PRP treatments are a form of regenerative medicine that utilizes the blood healing factors to help the body repair itself by means of injecting PRP into the damaged tissue. In regenerative orthopedics, it is typically used for the treatment of muscle strains, tears, ligament and tendon tears, minor arthritis, and joint instability. There have been more than 30 randomized controlled trials of PRP…
Read More About PRP InjectionsOur Doctors That Treat Baxter’s Neuropathy

Christopher J. Centeno, MD
Christopher J. Centeno, M.D. is an international expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate in orthopedics.
Dr. Centeno is one of the few physicians in the world with extensive experience in the culture expansion of and clinical use of adult bone marrow concentrate to treat orthopedic injuries. His clinic incorporates a variety of revolutionary pain management techniques to bring its broad patient base relief and results. Dr. Centeno treats patients from all over the US who travel to Colorado to undergo innovative, non-surgical treatments. Dr. Centeno has chaired multiple international research-based conferences. He also maintains an active research-based practice, with multiple publications listed in the US National Library of Medicine. Dr. Centeno has also served as editor-in-chief of a medical research journal dedicated to traumatic injury.
Dr. Centeno trained at the Baylor College of Medicine, Texas Medical Center, and the Institute for Rehabilitation Research. He hails from both Florida and New York and currently resides in Boulder, Colorado with his wife and three children.

John Schultz, MD
John R. Schultz M.D. is a national expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate for orthopedic injuries. He is board certified in Anesthesiology and Pain Medicine and underwent fellowship training in both. Dr. Schultz has extensive experience with same day as well as culture expanded bone marrow concentrate and sees patients at the CSC Broomfield, Colorado Clinic, as well the Regenexx Clinic in Grand Cayman. Dr. Schultz emphasis is on the evaluation and treatment of thoracic and cervical disc, facet, nerve, and ligament injuries including the non-surgical treatment of Craniocervical instability (CCI). Dr. Schultz trained at George Washington School of…
Read more
John Pitts, M.D.
Dr. Pitts is originally from Chicago, IL but is a medical graduate of Vanderbilt School of Medicine in Nashville, TN. After Vanderbilt, he completed a residency in Physical Medicine and Rehabilitation (PM&R) at Emory University in Atlanta, GA. The focus of PM&R is the restoration of function and quality of life. In residency, he gained much experience in musculoskeletal medicine, rehabilitation, spine, and sports medicine along with some regenerative medicine. He also gained significant experience in fluoroscopically guided spinal procedures and peripheral injections. However, Dr. Pitts wanted to broaden his skills and treatment options beyond the current typical standards of care.
Read more
Jason Markle, D.O.
Post-residency, Dr. Markle was selected to the Interventional Orthopedic Fellowship program at the Centeno-Schultz Clinic. During his fellowship, he gained significant experience in the new field of Interventional Orthopedics and regenerative medicine, honing his skills in advanced injection techniques into the spine and joints treating patients with autologous, bone marrow concentrate and platelet solutions. Dr. Markle then accepted a full-time attending physician position at the Centeno-Schultz Clinic, where he both treats patients and trains Interventional Orthopedics fellows. Dr. Markle is an active member of the Interventional Orthopedic Foundation and serves as a course instructor, where he trains physicians from around the world.
Read more
Brandon T. Money, D.O., M.S.
Dr. Money is an Indiana native who now proudly calls Colorado home. He attended medical school at Kansas City University and then returned to Indiana to complete a Physical Medicine and Rehabilitation residency program at Indiana University, where he was trained on non-surgical methods to improve health and function as well as rehabilitative care following trauma, stroke, spinal cord injury, brain injury, etc. Dr. Money has been following the ideology behind Centeno-Schultz Clinic and Regenexx since he was in medical school, as he believed there had to be a better way to care for patients than the status quo. The human body has incredible healing capabilities…
Read moreOther Resources
-
Stem Cell Treatment for Foot Pain: Learn the Truth.
Foot pain can be debilitating. Dr. Schultz discusses the 7 major causes of foot pain, traditional treatment options, stem cell treatment options, the different types of stem cells, factors that will influence the specific stem cell treatment plan, and the advantages of stem cells over steroids and surgery.
-
Tibial Nerve Injury: Symptoms, Diagnosis, and Treatment Options
Introduction Today we’re going to be talking about how to treat tibial nerve injury. We’ll be discussing exactly what is the tibial nerve is, the muscles the tibial innervates, how the nerve can be injured, as well as potential treatments for this. So let’s start off with what muscles are innervated by the tibial nerve.…
-
Morton’s Toe And Morton’s Neuroma: What You Need To Know
Morton’s Toe vs. Morton’s Neuroma – A small course on what they are and what can be done to treat them. Transcript Dr. John Schultz Hi, everybody. This is Dr. Schultz with the Centeno-Schultz Clinic. I thought we’d have a little fun today. You know, summer’s here and we’re having fun. Some of us are…
-
3 Things to Know About Navicular Bone Pain
Foot pain can be crippling. Where is Navicular Bone? Why Does my Navicular Bone Hurt? How do you treat Navicular bone pain? Let’s dig in. Where is Navicular Bone? There are 26 bones in the foot. The Navicular Bone is a small C-shaped bone located on the inside portion of the midfoot. It is nestled…
-
Life After Talonavicular Fusion: What You Should Know
Ankle pain can be excruciating often times making a simple step almost impossible. What is a Talonavicular fusion? What are the indications for a Talonavicular fusion? What are the complications from a Talonavicular fusion? What does life look like after talonavicular fusion? Let’s dig in. Foot Anatomy The foot is compromised of 26 bones. The…
-
Heel Pain In the Morning
Heel pain in the morning can make the first several steps excruciating. Given that, what are the causes of pain in the heel? What is plantar fasciitis? Can plantar fasciitis go away on its own? Are steroid injections helpful? Let’s dig in What Causes Pain in the Heel? Heel pain is a common foot disorder…