Interstitial Cystitis
Also known as bladder pain syndrome, interstitial cystitis is a chronic condition (i.e. it lasts more than six weeks) that affects the bladder, and usually its cause, such as infection, cannot be found.
One often overlooked potential cause of this problem is low back issues that irritate the nerves of the sacrum. The sacrum is the triangular bone towards the base of the spine. The cause of interstitial cystitis remains unclear, despite research into this condition.
This article is a complete guide on interstitial cystitis and also discusses how the lower back can be the cause, and if so, what can be done to ease this condition.
Are you a Candidate?
What Is Interstitial Cystitis?
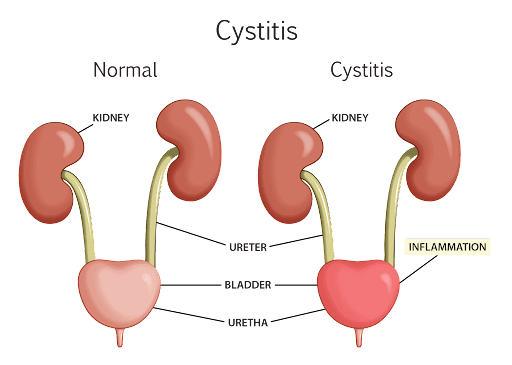
Interstitial cystitis is an inflammatory condition that affects the bladder. The bladder epithelium (the bladder lining) becomes inflamed due to an abnormal immune response in the bladder wall. Interstitial cystitis does not have an infectious cause and is usually a diagnosis of exclusion.
This means that doctors will investigate many other causes to rule them out before finally diagnosing interstitial cystitis. As a result, it can take a while before a patient is diagnosed, and sometimes patients are misdiagnosed.
Symptoms Of Interstitial Cystitis
The symptoms of interstitial cystitis can overlap with other conditions, such as endometriosis, urinary tract infection, and bladder carcinoma. So, while the symptoms of interstitial cystitis may not be confined to this condition, here are some common symptoms:
Pelvic Pain
A few characteristics of the pelvic pain seen in interstitial cystitis are listed below:
- Pain from interstitial cystitis is usually experienced in the pelvis or in the suprapubic area (the upper pubic area).
- The pain is commonly worse when the person needs to urinate and dissipates when they have emptied their bladder.
- In women, this pain can extend further into the area between the vagina and the anus.
Problems With Urination
A few characteristics of the urinary problems in interstitial cystitis are explained below:
- It is common for people with interstitial cystitis to experience an urgent need to pee, known as urgency.
- Additionally, people may also want to urinate more often, known as frequency. Urinary frequency can be more prevalent at night, which is known as nocturia.
- Some individuals also have discomfort while urinating, called dysuria.
Pain During Sexual Intercourse
Interstitial cystitis may cause pain during sexual intercourse:
- Women with interstitial cystitis may experience pain during sexual intercourse, called dyspareunia.
- In men, interstitial cystitis does not usually affect sexual intercourse.
Common Causes Of Bladder Pain Syndrome
The exact cause of interstitial cystitis is unclear in the literature. At present, it is thought that the reason is multifactorial. A few identified causes are listed below:
Epithelium Leak
An observed pathology of interstitial cystitis is urothelial permeability. Urothelial permeability means the epithelium of the bladder is leaky because of structural abnormalities of the lining. It is also due to low glycosaminoglycans (GAG) levels.
GAGs are complex compounds present in all mammals, which repair scarring and damage to the epithelium. It’s not known why some people have low GAG levels and leaky epithelium.
As a result of the leaky epithelial cells, various substances (immunoglobulin, and immune mediator chemicals and proteins) leak into the urine, causing interstitial cystitis. These findings have been identified on cystoscopy, a procedure where the bladder lining can be examined.
Autoimmune Reaction
Another possible cause of interstitial cystitis is autoimmune conditions. Autoimmune conditions occur when the body attacks itself, causing inflammation. Antibodies produced against the bladder’s cells have been seen in interstitial cystitis.
These antibodies usually target the nucleus and the epithelium. The presence of these antibodies may indicate this is an autoimmune condition.
Allergies
Allergies are a surprising cause of interstitial cystitis, in particular, from the use of illegally sourced and incorrectly prescribed ketamine. This is surprising, because ketamine prescribed at the right dose does not have the same effect.
Illegally sourced ketamine, either at the wrong dose or containing the wrong chemical substance, is believed to cause a range of undesirable conditions (urothelial damage, microvascular changes, autoimmunity, and infections).
It is not known whether it is the drug or its metabolites that cause this effect, but there is a strong association that leads to ketamine-induced cystitis.
Lumbosacral Spine Pathology
When the above causes are ruled out, consideration to low back issues should be given. The nerves that control the bladder run down from the brain through the spinal cord to the sacral nerve roots. If these nerves are irritated anywhere along that course, they can lead to bladder pain and dysfunction.
The most typical area for nerve irritation is the L5-S1 area of the spinal cord. If there is a spinal disk bulge, protrusion, or extrusion at that level, the disk can irritate or compress the sacral nerve roots as they come down. See pictures below:
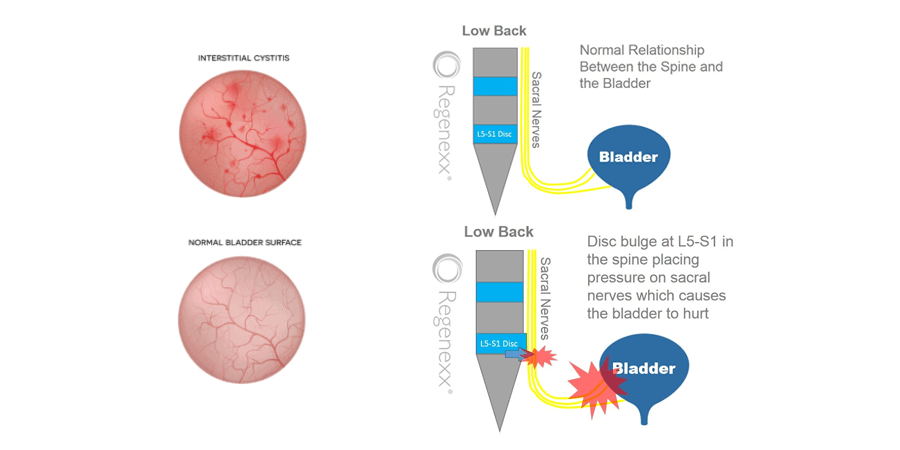
Other potential causes of sacral nerve root irritation could be:
a cyst (fluid sac) coming from an injured facet joint or injured lining of the sacral nerves (Tarlov cyst).
Often, these are asymptomatic (they show no symptoms) but sometimes can cause back or tailbone pain, or nerve pain down the leg or to the bladder. There can be some associated weakness.
Other rarer causes of sacral nerve irritation would be a mass such as a hematoma (bleed) or a tumor. These typically would cause significant back and/or nerve pain. They would be seen on an MRI and would require surgical removal.
What Low Back Symptoms Can Be Associated With Interstitial Cystitis?
Patients may or may not have low back pain. They could have pain in the tailbone or hips. There may be sciatica or pain radiating down one or both legs.
There can be associated numbness, tingling, or weakness down the leg(s). The bladder pain may be worse with certain activities that can irritate the back such as heavy lifting, sitting for prolonged periods, excessive twisting, high-impact activities, etc. There may have been a history of trauma or a fall on the back or tailbone.
Common Treatments For Bladder Pain Syndrome
The American Urological Association (AUA) recommends that people who have bladder pain syndrome should be made aware of how complex the condition is.
People should also understand that most patients may need a combination of treatments to relieve their symptoms. A visual chart or a patient-recorded bladder diary is necessary to document changes.
The common treatments for bladder pain syndrome are listed below:
Lifestyle Changes
Here are some details about the lifestyle changes that may be recommended for interstitial cystitis:
- Lifestyle changes usually include non-medical treatments that involve changing habits and learned behaviors.
- This includes a timed voiding (emptying) protocol where a person overcomes the urge to urinate. Instead, the voiding of urine is done as per a schedule.
If the urge occurs before it is time, the person is instructed to do quick contractions of the pelvic floor muscles to quieten the bladder until the urge passes. The time is gradually increased to two hours between each voiding.
Medications
Various classes of medications are used to treat interstitial cystitis. They include analgesics like paracetamol and ibuprofen, antihistamines, and antidepressants like amitriptyline, pentosan polysulfate, oxybutynin, and gabapentin. The doctor may use a combination of these medications to treat the condition.
Therapy And Injections
Neuromodulation therapy, bladder ulcer cauterization, and Botox injections have also been used with some success in individuals with bladder pain syndrome.
- Neuromodulation is the direct stimulation of sacral nerve roots using an implantable neuroprosthetic device, such as Interstim®. The procedure involves surgery to pass a lead through the S3 foramen (the gap in the S3 vertebra), and the patient wears a temporary external stimulator.
If their symptoms improve, a permanent lead and generator can be implanted for long-term stimulation. - Bladder ulcer cauterization is a procedure where the doctors identify an area of inflammation and then burn (or cauterize) it.
- Clinical trials have shown that Botox can relieve symptoms of interstitial cystitis by inhibiting muscle contraction and sensory nerve control and curbing the inflammation in the bladder.1 There is a significant improvement in the symptoms as the bladder relaxes. The treatment can last for about nine months.
- Physical therapy aimed at tightening pelvic floor muscles that support the bladder may also provide relief of symptoms.
Treatments If The Bladder Pain Is Coming From The Lower Back
Diagnostic injections around the nerves that are suspected to cause the problem may help temporarily with pain and aid in the diagnosis. These injections are called epidural injections. A local anesthetic can be used for diagnostic purposes only.
Steroids can sometimes be added to provide a few weeks or months of relief. However, if steroid injections only help temporarily, it is not advisable to repeat them regularly as they can have many potential side effects.
At the Centeno-Schultz Clinic, our physicians are musculoskeletal and spine specialists who treat spinal problems with injections of regenerative/reparative substances called orthobiologics. These are typically platelet-rich plasma (PRP) type injections.
At the Centeno-Schultz Clinic, we process our PRP via a lab so that we can customize treatments much better for each patient’s needs. We have found that using a specialized form of PRP, called platelet lysate, helps best to repair irritated or damaged nerves.
Platelet lysate is platelets that have been burst open so that all of the growth factors have been released. Platelet lysate has basic science evidence that it can help repair damaged nerves. (See references at the end of this article.)
Precisely injecting platelet lysate around the irritated nerves can help the bladder pain and dysfunction by reducing the inflammation and repairing the sacral nerves that service the bladder, thus treating the interstitial cystitis at the root cause.
Surgery For Interstitial Cystitis
Surgery is a last resort for interstitial cystitis. It is usually reserved for patients with severe or persistent symptoms for whom all other conservative treatments have failed. Here are some surgical options for those with bladder pain syndrome:
- Cystoscopy with hydrodistension: This is a process where the bladder is stretched to its full capacity with a liquid, under anesthesia. Hydrodistension can temporarily improve the symptoms of interstitial cystitis.
- Cystoplasty: Bladder augmentation surgery where the bladder is enlarged using part of the intestine, so it can hold more urine. This prevents any leakage of urine. Any residual urine flows into the new bladder. In some people, it is drained into a catheter (called a Mitrofanoff channel).
- Cystoplasty with supra trigonal resection: This is a procedure where the upper part of the bladder is reduced to achieve a normal-sized bladder. The trigone (the neck of the bladder) and ureters (tubes that carry the urine from the kidney to the bladder) are preserved.
The inflamed portion of the bladder is removed, and the trigone and ureters are kept, so the patient has normal urinary function. - Cystoplasty with subtrigonal resection: This is a rare procedure where the subtrigonal part of the bladder muscle is removed. The portion below the trigone is resected to achieve a normal-sized bladder and relieve the interstitial cystitis symptoms.
- Urinary diversion: This procedure involves making a urostomy – a reconstructed or re-routed urinary tract – to allow urine to exit the body safely. (This can be with or without cystectomy and urethral resection.)
Who Is At Risk Of Getting This Condition?
Currently, there are no screening tools to identify bladder pain in the early stages. Additionally, epidemiological studies on interstitial cystitis are limited. However, based on the limited existing studies, a few identifying features have been observed:
- It occurs most commonly in women between 50-59 and men between 56-74 years of age.
- It is five times more common in women than men.
- It is commonly seen in individuals with autoimmune conditions, chronic pain syndrome, and hypothyroidism.
- It is also commonly seen in people with mood disorders and depression.
When To See Your Doctor
Initially, it is common for individuals to think their symptoms might be caused by a urinary tract infection. However, you must see a doctor if you experience the following:
- Severe suprapubic pain uncontrolled by painkillers
- Blood in the urine
- A burning sensation while urinating
- Changes in the flow of urine
- Swollen lymph nodes in the inguinal (groin) area
- Unexplained weight loss
Be sure to tell your doctor if you also have low back pain, sacral pain, sciatica, previous low back injuries or trauma.
Examination And Diagnosis
As mentioned above, the diagnosis of bladder pain syndrome is through excluding other causes. Here are the steps the doctor will take to diagnose this condition:
- Physical examination: The doctor will do a thorough abdominal examination. (This will include a per rectal examination, external genitalia, and hernia orifices examination).
- Gynecological examination: This is done for women. (The doctor will look for vulvar pain, cervical excitation, and any prolapses/masses, as well as evaluate the anatomy and structures attached to the uterus.)
- Neurological examination: The doctor will do a complete neurological examination. This is because damage to the nerves can affect the filling and emptying of the bladder, which leads to bladder abnormalities. The nerves are responsible for bladder distension and contraction and so the nerves have to be examined. The doctor will check muscle tone, reflexes, power, and sensations and examine the cranial nerves.
- Blood tests: Various blood tests, including tests for glucose, glycosylated hemoglobin (HbA1c), and autoimmune panels will be done to check if there are other conditions affecting the bladder.
- Urine tests: Urine tests are used to test for microbiological causes of interstitial cystitis. These tests include urinalysis with a urine dipstick, urine microscopy, culture, and sensitivity of the urine to identify microbes in the urine.
- Sexual health screening: Individuals will also undergo sexual health screening with cervical or urethral swabs for sexually transmitted diseases like herpes and chlamydia.
- Urodynamic studies: Urodynamic studies are a group of tests done to evaluate how the body stores and releases urine. This will include the bladder, urethral sphincters, and urethra. These tests are painless and do not require sedation. Testing can include uroflowmetry, cystoflowmetry, electromyogram, pressure flow study, and video cystourethrography.
- Cystoscopy: Doctors use cystoscopy to examine and see inside the bladder, and even possibly take a biopsy of the bladder if they see a lesion.
- Lumbar MRI: If the back is the suspected cause of the bladder pain, the patient could be referred for an MRI (to help in diagnosing lumbosacral pathology).
Further Complications If Left Untreated
For many people, the symptoms of interstitial cystitis fluctuate so the tendency is to watch and wait. However, if it is left untreated and does not resolve spontaneously, the bladder may not heal. Additionally, scar tissue or fibrosis can develop.
The problem with fibrous scar tissue is that it reduces the volume of the bladder and can make the symptoms worse. The patient may also experience sleep disturbances, sexual dysfunction, anxiety, and depression. The urinary symptoms can also cause social and psychological effects.
What You Can Do To Prevent Recurrence
It is possible to prevent interstitial cystitis by hydrating adequately (ensuring you drink plenty of fluids), quitting smoking, and avoiding caffeinated beverages. If the low back is the cause, then therapeutic exercises to help your low back and hip posture, core and glute muscle strength, and a spine and hip mobility program can help prevent recurrence.
Interstitial cystitis can be effectively treated, however if it is left untreated it can get worse. If you’re experiencing symptoms of this condition and suspect your low back may be the cause, then make an appointment to talk to one of our board-certified musculoskeletal and regenerative medicine experts.
Are you a Candidate?

Christopher J. Centeno, MD
Christopher J. Centeno, M.D. is an international expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate in orthopedics.
Dr. Centeno is one of the few physicians in the world with extensive experience in the culture expansion of and clinical use of adult bone marrow concentrate to treat orthopedic injuries. His clinic incorporates a variety of revolutionary pain management techniques to bring its broad patient base relief and results. Dr. Centeno treats patients from all over the US who travel to Colorado to undergo innovative, non-surgical treatments. Dr. Centeno has chaired multiple international research-based conferences. He also maintains an active research-based practice, with multiple publications listed in the US National Library of Medicine. Dr. Centeno has also served as editor-in-chief of a medical research journal dedicated to traumatic injury.
Dr. Centeno trained at the Baylor College of Medicine, Texas Medical Center, and the Institute for Rehabilitation Research. He hails from both Florida and New York and currently resides in Boulder, Colorado with his wife and three children.

John Schultz, MD
John R. Schultz M.D. is a national expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate for orthopedic injuries. He is board certified in Anesthesiology and Pain Medicine and underwent fellowship training in both. Dr. Schultz has extensive experience with same day as well as culture expanded bone marrow concentrate and sees patients at the CSC Broomfield, Colorado Clinic, as well the Regenexx Clinic in Grand Cayman. Dr. Schultz emphasis is on the evaluation and treatment of thoracic and cervical disc, facet, nerve, and ligament injuries including the non-surgical treatment of Craniocervical instability (CCI). Dr. Schultz trained at George Washington School of…
Read more
John Pitts, M.D.
Dr. Pitts is originally from Chicago, IL but is a medical graduate of Vanderbilt School of Medicine in Nashville, TN. After Vanderbilt, he completed a residency in Physical Medicine and Rehabilitation (PM&R) at Emory University in Atlanta, GA. The focus of PM&R is the restoration of function and quality of life. In residency, he gained much experience in musculoskeletal medicine, rehabilitation, spine, and sports medicine along with some regenerative medicine. He also gained significant experience in fluoroscopically guided spinal procedures and peripheral injections. However, Dr. Pitts wanted to broaden his skills and treatment options beyond the current typical standards of care.
Read more
Jason Markle, D.O.
Post-residency, Dr. Markle was selected to the Interventional Orthopedic Fellowship program at the Centeno-Schultz Clinic. During his fellowship, he gained significant experience in the new field of Interventional Orthopedics and regenerative medicine, honing his skills in advanced injection techniques into the spine and joints treating patients with autologous, bone marrow concentrate and platelet solutions. Dr. Markle then accepted a full-time attending physician position at the Centeno-Schultz Clinic, where he both treats patients and trains Interventional Orthopedics fellows. Dr. Markle is an active member of the Interventional Orthopedic Foundation and serves as a course instructor, where he trains physicians from around the world.
Read more
Brandon T. Money, D.O., M.S.
Dr. Money is an Indiana native who now proudly calls Colorado home. He attended medical school at Kansas City University and then returned to Indiana to complete a Physical Medicine and Rehabilitation residency program at Indiana University, where he was trained on non-surgical methods to improve health and function as well as rehabilitative care following trauma, stroke, spinal cord injury, brain injury, etc. Dr. Money has been following the ideology behind Centeno-Schultz Clinic and Regenexx since he was in medical school, as he believed there had to be a better way to care for patients than the status quo. The human body has incredible healing capabilities…
Read moreOther Resources for Interstitial Cystitis
-
Everything You Need to Know about Hip Ligaments
The hip joint is a large ball and socket joint that’s important for lower extremity movement. The joints consist of the articulation of the femur (upper thigh bone/ball) and the acetabulum (the socket). The bones are lined with cartilage and the acetabulum is lined with a fibrocartilage called the labrum. The hip joints, as with…
-
Biceps Femoris Tendonitis Stem Cell Treatment: aka Hamstring Treatment Options
Hamstring injuries are a common sports injury. Dr. Schultz describes what the biceps femoris is, what tendonitis is, what biceps femoris tendonitis is, what causes it, the symptoms, treatment, and biceps femoris tendonitis stem cell treatment options.
-
Pelvic Ligaments: The Uncomfortable Truth You Need to Know!
The pelvis is held together by three principal ligaments: the iliolumbar, sacrotuberous and sacrospinous. Dr. Schultz discusses the causes of pelvic ligament injuries, symptoms, and novel new treatment options.
-
Groin Pain after Hip Replacement: What Is Being Missed?
Your hip replacement surgery was 6 months ago and you are still having pain. Is it normal to have groin pain after total hip replacement? What are the causes of groin pain after total hip replacement? What are the signs of a failing hip replacement? What treatment options exist? Let’s dig in. Is it Normal…
-
8 Reasons for Hip Replacement Failure
Hip replacement surgery replaces a worn out or damaged hip joint with an artificial joint called a prosthesis. The symptoms of hip replacement failure are pain and limited mobility. Dr. Schultz discusses the 8 major causes of hip replacement failure and important treatment options.
-
Levator Scapulae Massage: Options When It Doesn’t Work
The Levator Scapulae is an important neck muscle that lifts and rotates the scapulae. Dr. Schultz discusses the causes of levator scapulae pain and tightness and new, natural treatment options.
References
Research showing that platelet lysate can help repair damaged nerves:
- Platelet-derived growth factors (PDGFs) stimulate neurotrophic factors to be released, which promote the regeneration of peripheral nerves. Glia. 2009 Jul;57(9):947-61
- Insulin-like Growth Factor-1 (IGF-1) directly binds to IGF-1 receptors to stimulate the first step in fatty acid synthesis for re-myelination. Glia. 1997 Mar;19(3):247-58
- Vascular endothelial factor (VEGF) induces angiogenesis, which is a critical step that precedes axon regeneration in animal models. Exp Neurol. 2001 Dec;172(2):398-406.
- In both animal models and case reports that the application of PRP can significantly improve peripheral nerve axon regeneration with gaps varying from 3 – 12 cm. Prog Neurobiol. 2014 May;116:1-12 and Neurosurgery. 2011 Dec;69(6):E1321-6.
- It also has an inflammatory effect around nerves. We have used platelet lysate and PRP to treat spinal problems for years with supporting research. Centeno C, Markle J, Dodson E, Stemper I, Williams CJ, Hyzy M, Ichim T, Freeman M. Treatment of lumbar degenerative disc disease-associated radicular pain with culture-expanded autologous mesenchymal stem cells: a pilot study on safety and efficacy. J Transl Med. 2017 Sep 22;15(1):197. doi: 10.1186/s12967-017-1300-y. PMID: 28938891; PMCID: PMC5610473.
- Treatment of lumbar degenerative disc disease-associated radicular pain with culture-expanded autologous mesenchymal stem cells: a pilot study on safety and efficacy – PubMed (nih.gov) Centeno C, Markle J, Dodson E, Stemper I, Hyzy M, Williams C, Freeman M. The use of lumbar epidural injection of platelet lysate for treatment of radicular pain. J Exp Orthop. 2017 Nov 25;4(1):38. doi: 10.1186/s40634-017-0113-5. PMID: 29177632; PMCID: PMC5701904.
- The use of lumbar epidural injection of platelet lysate for treatment of radicular pain – PubMed (nih.gov)). Wongjarupong A, Pairuchvej S, Laohapornsvan P, Kotheeranurak V, Jitpakdee K, Yeekian C, Chanplakorn P.
- “Platelet-Rich Plasma” epidural injection an emerging strategy in lumbar disc herniation: a Randomized Controlled Trial. BMC Musculoskelet Disord. 2023 Apr 28;24(1):335. doi: 10.1186/s12891-023-06429-3. PMID: 37118707; PMCID: PMC10141936. Le VT, Nguyen Dao LT, Nguyen AM.
- Transforaminal injection of autologous platelet-rich plasma for lumbar disc herniation: A single-center prospective study in Vietnam. Asian J Surg. 2023 Jan;46(1):438-443. doi: 10.1016/j.asjsur.2022.05.047. Epub 2022 May 28. PMID: 35637114. Saraf A, Hussain A, Sandhu AS, Bishnoi S, Arora V.
- Transforaminal Injections of Platelet-Rich Plasma Compared with Steroid in Lumbar radiculopathy: A Prospective, Double-Blind Randomized Study. Indian J Orthop. 2023 May 5;57(7):1126-1133. doi: 10.1007/s43465-023-00898-3. PMID: 37384009; PMCID: PMC10293530. Bise S, Dallaudiere B, Pesquer L, Pedram M, Meyer P, Antoun MB, Hocquelet A, Silvestre A.
- Comparison of interlaminar CT-guided epidural platelet-rich plasma versus steroid injection in patients with lumbar radicular pain. Eur Radiol. 2020 Jun;30(6):3152-3160. doi: 10.1007/s00330-020-06733-9. Epub 2020 Feb 24. PMID: 32095875.)
- Jhang JF. Using Botulinum Toxin A for Treatment of Interstitial Cystitis/Bladder Pain Syndrome-Possible Pathomechanisms and Practical Issues. Toxins (Basel). 2019;11(11):641. Published 2019 Nov 4. doi:10.3390/toxins11110641